Introduction
The aim of this study was to investigate whether proclination of the maxillary central incisor near a cleft leads to gingival recession in patients born with unilateral cleft lip and palate.
Methods
Forty patients with unilateral cleft lip and palate were retrospectively enrolled. By using intraoral slides, casts, and cephalograms, changes in gingival recession and proclination were measured. The 2-sample t test, correlation, and stepwise logistic regression analyses were applied.
Results
There were statistically significant differences in proclination variations between subjects with and without increased gingival recession ( P <0.0001). A positive correlation was shown between proclination and gingival recession. Bone grafting during treatment resulted in a significant difference in gingival recession ( P <0.05). Every 2° of increase in the angle between the long axis of the maxillary central incisors and the sella-nasion plane had a 3.06 times greater risk for gingival recession (odds ratio, 3.06; 95% confidence interval, 1.329-7.046; P = 0.0086).
Conclusions
Proclination of the maxillary central incisor adjacent to the cleft is positively correlated with gingival recession in patients with unilateral cleft lip and palate. Proclination should be limited to prevent gingival recession and its esthetic and functional problems. It is better for a borderline cleft patient to have orthognathic surgery rather than camouflage treatment. Bone grafting during treatment might benefit gingival recession. The angle between the long axis of the maxillary central incisors and the sella-nasion plane is considered the strongest predictor of gingival recession.
Cleft lip and palate is the most common congenital developmental deformity of the oral and maxillofacial region in China. According to the latest data from the Chinese National Birth Defects Monitoring Network, the prevalence of overall clefts was 16.63 per 10,000 births from 1996 to 2005.
Sequential treatment as the widely accepted therapy protocol for cleft subjects involves multidisciplinary, including surgical and orthodontic, management, which might contribute to mucogingival alterations. Gingival recession, a mucogingival disorder, was found frequently in the teeth near the cleft, especially on the mesial side, such as the maxillary central incisors. Andlin-Sobocki et al proposed that gingival recession occurs preoperatively only for teeth mesial to the cleft. Almeida et al further demonstrated that the prevalence of gingival recession in teeth close to the cleft area was 10 times greater in patients with a cleft.
Since gingival recession initiates unpleasant esthetics and in some cases functional problems such as root sensitivity and increased susceptibility to root caries, its detriment for physical and mental health can never be ignored. Thus, many studies have explored its predisposing and precipitating factors.
Previous studies have mainly focused on the sequelae of surgeries as possible predisposing factors, such as narrow width of keratinized gingiva, abnormal frenum attachment, and reduced marginal bone height. Parfitt and Mjör observed predispositions to the development of gingival recession when there are frena. Andlin-Sobocki et al demonstrated that bone grafting before the eruption of canines resulted in satisfactory periodontal conditions involving gingival recession for teeth in the cleft region. Almeida et al concluded that there might be recession reduction in increased keratinized mucosa.
However, few studies have addressed the correlation between orthodontic treatment and gingival recession. The effect of tooth movement during orthodontic treatment on gingival recession remains unclear. Andlin-Sobocki and Bodin reported a reasonable frequency of gingival recession when lingually tipped teeth achieved adequate positioning in the dental arch, or when well-aligned teeth were tipped bucally. Slutzkey and Levin found a strong correlation between the severity and extent of recession with past orthodontic treatment. Nevertheless, Almeida et al observed no statistically significant association between tooth position and gingival recession. Djeu et al concluded that there was no correlation between the degree of proclination of the incisors and the gingival recession in their patient sample. Allais and Melsen proposed that proclination is a valuable alternative to extraction without clinically relevant deterioration of the periodontium, such as gingival recession.
Dorfman suggested that a thin or nonexistent labial plate of bone and inadequate or absent keratinized gingiva resulted in gingival recession of the mandibular incisors in a normal population. As to subjects with unilateral cleft lip and palate, the decreased bone support and reduced keratinized gingiva width adjacent to the cleft area can never be doubted; these might pose a great threat to gingiva. Therefore, a labially tipped maxillary central incisor near the cleft region seems to be a critical factor for enhancing gingival recession in patients with unilateral cleft lip and palate during orthodontic treatment.
In this study, we aimed to assess the influence of maxillary central incisor proclination on gingival recession near the cleft area in patients with unilateral cleft lip and palate.
Material and methods
A group of 86 subjects with clefts seeking orthodontic treatment at Shanghai Ninth People’s Hospital in China within the past 5 years was screened. Included were patients with unilateral cleft lip and palate having complete records who had started orthodontic therapy involving a fully erupted maxillary central incisor adjacent to the cleft region for more than 6 months. Exclusion criteria comprised the presence of maxillary deciduous incisors, maxillary incisors severely rotated and tipped toward the cleft, unreadable intraoral slides, gingivitis, extractions in the cleft area, systemic disorders, history of smoking, and medications related to gingival alterations. A total of 40 patients who met the criteria were selected for this study.
According to the analysis of the pretreatment and posttreatment study casts and clinical intraoral slides, patients whose gingival recession occurred or had been exacerbated after treatment were enrolled in the experimental group. They were regarded as patients with increased gingival recession. Those whose recession remained the same or decreased after therapy were included in the control group. They were considered as subjects without increased recession. No institutional review board approval or written consent was obtained, but the patients were informed about the purpose of this study. Their confidentiality and rights were protected.
Among the 40 subjects, 15 were female and 25 were male. Their average age at the beginning was 13.2 years (range, 8-26 years). Five subjects were over 18 years old. The range of treatment duration was 7 to 38 months, with a mean of 21.9 months. Fourteen patients had a successful alveolar bone graft during their orthodontic treatment without bone resorption or inflammation.
On the study models, crown height was measured from the highest point of the curvature of the gingival margin to the lowest level of the incisal edge along the long axis of the central incisor ( Figure ). The pretreatment and posttreatment measurements were made by using a vernier caliper (American Bunker Tools International, Linyi City, China) accurate to 0.02 mm.
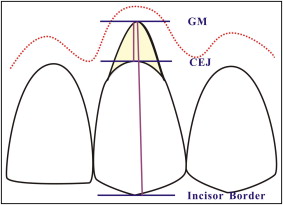
In line with the description of Coatoam et al, all intraoral slides were projected onto a piece of blank construction paper measuring 9 × 11 in to obtain all data at the same magnification. Just as cast crown length was surveyed, so was photographic crown height. For photographic gingival recession, the measurements were made from the deepest point of the curvature of the gingival margin to the cementoenamel junction along the axis by using calipers ( Figure ).
After collection of all the data described above, the actual gingival recession was calculated as follows: actual gingival recession = photographic recession × cast crown height ÷ photographic crown height.
Using Dental Studio NX 2006 software (version 6.0; Software Nemotec, Madrid, Spain), we measured the sagittal variations in proclination of the maxillary central incisors close to the cleft area that appeared during orthodontic treatment on pretreatment and posttreatment lateral cephalograms. The maxillary central incisors were the most visible teeth in the dentition on the lateral cephalometric radiographs. To further identify their inclination, their positioning on cephalograms was ascertained after comparisons with the study models and intraoral slides. Measurements had an accuracy of 0.1° or 0.1 mm.
All cephalometric films were taken with the Digital Panoramic and Cephalometric System (8000C; Eastman Kodak, Rochester, NY) at Shanghai Ninth People’s Hospital. No correction was made for radiographic enlargement.
Three measurements from 2 cephalometric analyses were used to determine incisor position. The sella-nasion plane, a line from sella turcica to the junction between the nasal and frontal bones, is an easily and reliably detected horizontal reference line on cephalometric films. To quantify incisor proclination, the angle between the long axis of the maxillary central incisor and the sella-nasion plane (U1-SN angle) was measured by using roentgen cephalometric analysis, which represents the axial proclination of the maxillary incisor to the anterior cranial base.
The Steiner analysis evaluates the relationship of the maxillary incisor to the NA line (the line from nasion to Point A), thus establishing the relative protrusion of the dentition. The distance between the maxillary central incisor tip and the NA line was measured, as well as the angle between the long axis of the maxillary central incisors and the NA line. This distance establishes how prominent the incisor is relative to its supporting bone, and the inclination indicates whether the tooth has been tipped to its position or has moved there bodily.
Statistical analysis
The Statistical Analysis System (version 9.13; SAS Institute, Cary, NC) was used to analyze the measurements. The 2-sample t test analysis was used to determine whether the differences between the increased gingival recession group and not increased group lie in the range of proclination variations. Furthermore, correlation analysis was performed to identify a correlation coefficient between each of the 3 measurement changes and the gingival recession changes, and whether there was a positive or negative association between them. Finally, 1-way analysis of variance (ANOVA) was used to determine whether age, sex, treatment duration, alveolar bone grafting during the treatment, and U1-SN angle were possible influential factors for gingival recession. Stepwise logistic regression analysis was used among the good predictor variables that were selected by the analyses above, while evaluating the chances for gingival recession in the maxillary central incisor near the cleft area under these risk indicators. A P value of 0.05 or less was deemed to be statistically significant.
Results
After the original measurements, all variables were measured again in 2 weeks to determine the reproducibility of measurements. The coefficient of reliability (1 − Se 2 /St 2 ) was used to evaluate the errors between these measurements. The first series of measurements was taken as representative, and all coefficients of reliability were more than 0.9 ( Table I ). Therefore, the measurements in this study should be reliable.
| Gingival recession (mm) | U1-SN angle (°) | U1-NA angle (°) | U1-NA distance (mm) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 | T2 | D | T1 | T2 | D | T1 | T2 | D | T1 | T2 | D | |
| Mean | 0.30 | 0.30 | 0.00 | 8.05 | 8.65 | 0.61 | 8.30 | 8.54 | 0.23 | 2.83 | 3.45 | 0.61 |
| Variance | 0.19 | 0.19 | 0.00 | 51.98 | 64.43 | 4.12 | 62.71 | 69.35 | 1.07 | 10.90 | 12.58 | 1.07 |
| SD | 0.44 | 0.44 | 0.04 | 7.21 | 8.03 | 2.03 | 7.92 | 8.33 | 1.03 | 3.30 | 3.55 | 1.03 |
| SE | 0.07 | 0.07 | 0.01 | 1.14 | 1.27 | 0.32 | 1.25 | 1.32 | 0.16 | 0.52 | 0.56 | 0.16 |
| Coefficient of reliability | 99.67% | 96.04% | 99.15% | 95.11% | ||||||||
The severity of pretreatment and posttreatment amounts of gingival recession is shown in Table II . At baseline, all recessions were scored as mild (<3 mm). After orthodontic treatment, 2 subjects had moderate recessions (3 mm). Eleven patients (27.5%) showed recession of 2 mm or more, compared with 2 patients (5%) before treatment ( P = 0.0064). There was a trend for increasing severity of gingival recession after treatment in this sample of patients with unilateral cleft lip and palate.
| Gingival recession (mm) | Patients (n) | |
|---|---|---|
| Pretreatment | Posttreatment | |
| 0-1 | 23 | 11 |
| 1-2 | 15 | 18 |
| 2-3 | 2 | 11 |
The average amounts of maxillary central incisor proclination changes in all patients, experimental and control, are shown in Table III . A positive difference between the final and the initial angle or distance was considered as a proclined incisor. A negative difference or no difference was deemed a retroclined tooth. For the U1-SN angle, the average changes for the experimental and control groups were 10.40° and −1.35°, respectively. For the U1-NA distance, the average alterations were 3.94 and −1.60 mm, respectively. For the U1-NA angle, the average variations were 10.96° and −2.31°, respectively. The proclination changes in the experimental group were greater than those in the control group.
| U1-SN angle (°) | U1-NA distance (mm) | U1-NA angle (°) | Recession (mm) | |
|---|---|---|---|---|
| (Normal, 102.5 ± 3.4) | (Normal, 6.0 ± 1.0) | (Normal, 22.8 ± 5.2) | ||
| All patients | ||||
| Pretreatment | 91.00 ± 8.90 | 1.85 ± 3.00 | 14.78 ± 8.45 | 0.96 ± 0.57 |
| Posttreatment | 99.05 ± 8.02 | 4.68 ± 2.45 | 23.08 ± 8.37 | 1.25 ± 0.69 |
| Change | 8.05 ± 7.21 | 2.83 ± 3.30 | 8.30 ± 7.92 | 0.30 ± 0.44 |
| Experimental group | ||||
| Pretreatment | 89.28 ± 8.57 | 1.01 ± 2.56 | 13.06 ± 8.30 | 0.98 ± 0.55 |
| Posttreatment | 99.68 ± 8.09 | 4.95 ± 2.40 | 24.02 ± 8.45 | 1.40 ± 0.62 |
| Change | 10.40 ± 5.53 | 3.94 ± 2.10 | 10.96 ± 5.66 | 0.41 ± 0.41 |
| Control group | ||||
| Pretreatment | 97.89 ± 6.94 | 5.18 ± 2.28 | 21.64 ± 5.12 | 0.84 ± 0.69 |
| Posttreatment | 96.54 ± 7.73 | 3.58 ± 2.50 | 19.33 ± 7.33 | 0.69 ± 0.70 |
| Change | −1.35 ± 5.28 | −1.60 ± 3.61 | −2.31 ± 6.81 | −0.15 ± 0.17 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


