Introduction
Placement torque and damping capacity may increase when the orthodontic anchor screws make contact with an adjacent root. If this is the case, root contact can be inferred from the placement torque and damping capacity. The purpose of this study was to verify the detectability of root proximity of the screws by placement torque and damping capacity. For this purpose, we investigated the relationship among placement torque, damping capacity, and screw-root proximity.
Methods
The placement torque, damping capacity, and root proximity of 202 screws (diameter, 1.6 mm; length, 8.0 mm) were evaluated in 110 patients (31 male, 79 female; mean age, 21.3 ± 6.9 years). Placement torque was measured using a digital torque tester, damping capacity was measured with a Periotest device (Medizintechnik Gulden, Modautal, Germany), and root contact was judged using cone-beam computed tomography images.
Results
The rate of root contact was 18.3%. Placement torque and damping capacity were 7.8 N·cm and 3.8, respectively. The placement torque of screws with root contact was greater than that of screws with no root contact ( P <0.05; effect size, 0.44; power, <0.8). Damping capacity of screws with root contact was significantly greater than that of screws with no root contact ( P <0.01; effect size, >0.5; power, >0.95).
Conclusions
It was suggested that the damping capacity is related to root contact.
Highlights
- •
We examined damping capacity to verify the detectability of screw-root proximity.
- •
Our hypothesis: Periotest values (PTV) cannot be used to estimate root proximity of screws.
- •
Placement torque and PTV were measured, and root contact was judged with cone-beam computed tomography.
- •
PTV was strongly related to root contact; the null hypothesis was rejected.
- •
In addition to PTV, x-ray exploration is recommended for accurate diagnosis.
Orthodontic anchor screws have been used widely as anchors in orthodontic treatment over the last decade. Lately, the self-drilling method has been adopted worldwide because self-drilling screws require short operating times, cause little bone debris and thermal damage, and are associated with less morbidity and minimal patient discomfort. Screws can reduce patients’ burden and the need for their cooperation, such as with the use of headgear or a holding arch; however, many patients have complications, such as loosening of screws, pain and swelling around the placement site, and adjacent tooth-root contact. Tooth-root contact is thought to be an important risk factor for the failure of screws. Many researchers have investigated the influence of screw-root proximity on stability and have concluded that root proximity clearly influences the stability and success rate of screws as anchorage.
Stability and resistance to screw loosening can be evaluated using placement torque and damping capacity. Motoyoshi et al investigated the relationship between placement torque and the success rate of screws; they recommended placement torque of 5 to 10 N·cm to enhance the success rate. Suzuki et al also measured maximum placement torque when tightening screws and indicated that screws placed with torque greater than 10 N·cm tended to have a lower success rate. However, Uemura et al evaluated the relationship between the damping capacity measured with the Periotest device (Medizintechnik Gulden, Modautal, Germany) (Periotest value [PTV]) of the screws during the healing phase and the prognosis for screw stability, and they suggested that a significant decrease in the PTV of the screws indicates a good prognosis for subsequent screw stability. Damping capacity is a material property to absorb vibration, which can be recorded by the Periotest device. The tapping head of the device returns rapidly under rigid bone-screw conditions; the head’s contact time increases under pliable conditions, and the average contact time is the PTV. Motoyoshi et al reported that the rate of a screw touching an adjacent tooth root eventually increased to about 20%, and a PTV greater than 6 could be used clinically to estimate the root proximity of self-drilling screws. In addition to the damping capacity, placement resistance when inserting screws into bone may increase when the screws make contact with an adjacent root; this can increase the placement torque. If this is the case, root contact can be inferred from the PTV and the placement torque. Motoyoshi et al could not substantiate a significant relationship between placement torque and root contact, although they found greater placement torque in their subjects with root contact on average. Further examinations should be performed to verify whether screws with root contact show higher placement torque than those without contact.
In this study, we investigated the rates of root contact and screw stability, as well as the relationship among placement torque, PTV, and screw-root proximity. Our null hypothesis was that PTVs cannot be used to estimate the root proximity of self-drilling screws.
Material and methods
This study included 110 patients (31 male, 79 female; average age, 21.3 ± 6.9 years; 202 screws) who underwent screw placement surgery with a self-drilling method. All screws were placed in the maxillary buccal alveolar bone between the second premolar and the first molar as absolute anchors for anterior tooth retraction in patients needing first premolar extractions at Nihon University Dental Hospital in Japan.
This study was approved by the ethical review board of Nihon University School of Dentistry (No. 2012-2). All patients consented to participate in the study.
The screws used were 1.6 mm in diameter and 8 mm long (Biodent, Tokyo, Japan). Local anesthesia was administered, and the screws were placed with a hand driver without predrilling. We then measured the maximum placement torque in the terminal turning of the screws using a torque tester (nominal accuracy, ±0.5%; DIS-RL05; Sugisaki Meter, Ibaraki, Japan) and PTV using the Periotest device immediately after placement. Periotest measurements were determined in the mesial direction for each screw by holding the tip of the instrument’s handpiece perpendicular to the long axis of the screw. Each measurement was repeated 3 times, and the average value was calculated. An orthodontic force of about 2 N was then applied to the screw, and cone-beam computed tomography (CBCT) images were taken for each subject to determine root proximity. Screws that endured the orthodontic force for 6 months or more without mobility were considered successful.
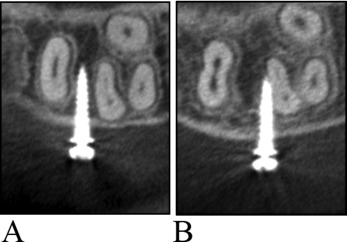
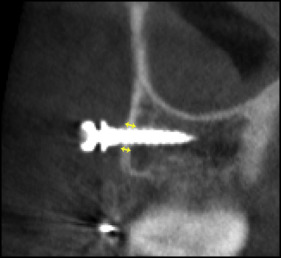
CBCT (3D Accuitomo; J. Morita, Osaka, Japan) was used for diagnostic imaging of the placement site, with a voxel size of 0.125 mm 3 in super-high resolution mode, an x-ray tube voltage of 80 kV, and a current of 5.5 mA. A 3-dimensional viewer program (One Volume Viewer, version 1.6.1.13; J. Morita) was used to define the tomographic cross sections that corresponded to the long axis of the screw and to simultaneously observe the cross sections of the adjacent tooth root. One examiner (M.I.) determined the root proximity ( Fig 1 ) to eliminate interexaminer error. Cortical bone thickness at the placement site ( Fig 2 ) was also measured by the examiner. To evaluate intraexaminer error, we randomly selected the CBCT images of 10 subjects and reevaluated root proximity and cortical bone thickness 2 weeks after the initial evaluation. Measurement error of the cortical bone thickness was calculated using the Pearson correlation coefficient. The chi-square or Fisher exact test was used to evaluate the variability of the success rate and the rate of root contact according to placement location and sex. The Fisher exact test was used when more than 20% of the cells had an expected value less than 5 in a contingency table. The unpaired t test was used to evaluate placement torque and PTV according to root proximity, cortical bone thickness at the placement site according to sex, and PTV according to cortical bone thickness. The Pearson correlation coefficient was also calculated to investigate associations between PTV and cortical bone thickness, and between PTV and placement torque. A retrospective (post hoc) power analysis was used to evaluate sample power and to calculate effect sizes. These analyses were performed with software (version 18.0; SPSS, Tokyo, Japan). P values less than 0.05 were considered statistically significant.
Results
In the 2 root-proximity determinations, there was no difference between the first and the second measurements in the 10 randomly selected CBCT images. The reliability test for measurements of cortical bone thickness showed a significant correlation ( r = 0.85; P <0.01), confirming the accuracy of the measurements. The rate of root contact was 18.3%, and there was no significant difference in root contact between the right and left sides, or between male and female subjects ( Table I ). A significantly lower success rate was seen in the root-contact group than in the no-contact group ( Table II ). The success rate on the right and in the female patients was significantly better in the no-contact group than in the contact group ( P <0.01). The mean placement torque and PTV were 7.8 N·cm and 3.8, respectively, and there was no significant difference in these measurements between the right and left sides or between the sexes ( Table III ). There was a significant difference, with a medium effect size, in PTV between the no-contact and contact groups ( Table IV ); furthermore, a significantly greater PTV was seen in the failure group, with a large effect size ( Table V ). In the root-contact group, 33 screws contacted the distal teeth (first molars), and 4 screws contacted the mesial teeth (second premolars); screws placed on the right side tended to contact the distal teeth significantly more often than did the screws on the left side ( Table VI ). Cortical bone in the male subjects was significantly thicker than in female subjects ( Table VII ). There were no significant differences between PTVs when cortical bone thickness was greater than 0.8 mm and less than 0.8 mm ( Table VIII ). In addition, the Pearson correlation coefficient was used to calculate associations between PTV and cortical bone thickness, and between PTV and placement torque; we found no significant correlations ( Table IX ). Table X lists the numbers of screws with and without root contact with PTVs greater than 6 and less than 6.
| No contact | Contact | |||
|---|---|---|---|---|
| n | % | n | % | |
| Right | 81 | 79.4 | 21 | 20.6 |
| Left | 84 | 84.0 | 16 | 16.0 |
| Effect size | 0.06 | |||
| Power | 0.14 | |||
| Male | 45 | 83.3 | 9 | 16.7 |
| Female | 120 | 81.1 | 28 | 18.9 |
| Effect size | 0.03 | |||
| Power | 0.07 | |||
| Total | 165 | 81.7 | 37 | 18.3 |
| No contact | Contact | Effect size | Power | Total | ||||
|---|---|---|---|---|---|---|---|---|
| Failure | Success rate (%) | Failure | Success rate (%) | Failure | Success rate (%) | |||
| Right | 1 | 98.8 | 5 | 76.2 † | 0.39 | 0.98 | 6 | 94.1 |
| Left | 1 | 98.8 | 2 | 87.5 ∗ | 0.24 | 0.67 | 3 | 97.0 |
| Male | 1 | 97.8 | 1 | 88.9 | 0.18 | 0.26 | 2 | 96.3 |
| Female | 1 | 99.2 | 6 | 78.6 † | 0.38 | 0.99 | 7 | 95.3 |
| Total | 2 | 98.8 | 7 | 81.1 † | 0.33 | 0.99 | 9 | 95.5 |
| n | Torque (N·cm) | PTV | |||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Right | 102 | 8.0 | 3.0 | 3.3 | 3.8 |
| Left | 100 | 7.6 | 3.2 | 4.2 | 3.7 |
| Effect size | 0.13 | 0.24 | |||
| Power | 0.15 | 0.40 | |||
| Male | 54 | 7.9 | 3.0 | 3.3 | 3.0 |
| Female | 148 | 7.7 | 3.1 | 4.0 | 4.0 |
| Effect size | 0.07 | 0.20 | |||
| Power | 0.07 | 0.24 | |||
| Total | 202 | 7.8 | 3.1 | 3.8 | 3.8 |
| No contact | Contact | Effect size | Power | |
|---|---|---|---|---|
| Torque (N·cm) | ||||
| Mean | 7.5 | 8.9 ∗ | 0.44 | 0.68 |
| SD | 3.0 | 3.3 | ||
| PTV | ||||
| Mean | 3.3 | 6.0 † | 0.69 | 0.96 |
| SD | 3.5 | 4.3 |
| Success | Failure | Effect size | Power | |
|---|---|---|---|---|
| Torque (N·cm) | ||||
| Mean | 7.8 | 8.1 | 0.10 | 0.06 |
| SD | 3.1 | 2.9 | ||
| PTV | ||||
| Mean | 3.5 | 9.2 ∗ | 1.40 | 0.98 |
| SD | 3.6 | 4.5 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


