The standard of care in patients who have a complete cleft is to perform secondary bone grafting of the absent bone in the alveolus and anterior maxilla with autogenous cancellous bone somewhere between 6 and 9 years of age. Although other treatment regimens have been suggested, no regimen has proved to be equal, and certainly not superior, to this regimen. The exact timing of secondary bone reconstruction has been a source of contention for years, and there is currently good evidence that secondary bone reconstruction is best done somewhere between 6 and 9 years of age. This does not negate later secondary reconstruction; yet, the overall result in terms of toot eruption, orthodontic tooth movements into the grafted area, and periodontal health is superior when it is done at an earlier age. One of the major factors that the author has observed in delayed or late secondary reconstruction occurs when orthodontic treatment is performed in the area before bone grafting. This generally has an adverse effect on the adjacent (central or lateral incisor or cuspid) teeth in that they are moved inadvertently into an area of inadequate bone, and therefore lose significant periodontal support. Conversely, when no orthodontic treatment is performed in the older patient and adequate adjacent periodontal bone support exists, secondary bone grafting can be done with subsequent orthodontic treatment and a successful outcome can be achieved ( Fig. 1 ).
The indications for alveolar anterior maxillary bone reconstruction are multiple, but the primary reason is still, and always has been, to provide a sufficient quantity and quality of bone in the cleft area to allow for eruption of coadjacent teeth and the subsequent orthodontic movement of teeth into the cleft bone grafted area. Additional reasons include closure of the vestibular and oral nasal fistulas, providing adequate support of the nasal base on the unilateral cleft side, and possibly allowing for osseointegrated implants to be placed when teeth are missing.
This article sequentially describes the details of the surgical procedure for reconstruction of the alveolar-anterior maxillary bone defect in unilateral and then bilateral cleft cases. Additional and alternative techniques have been suggested; however, these basic techniques can be used in most instances and have provided the author with ideal results.
Surgical technique: unilateral cleft
About 10 minutes before initiating surgery, infiltration of 2% lidocaine with 1/100,000 epinephrine is performed palatally and throughout the vestibular sulcus in the areas of planned surgery.
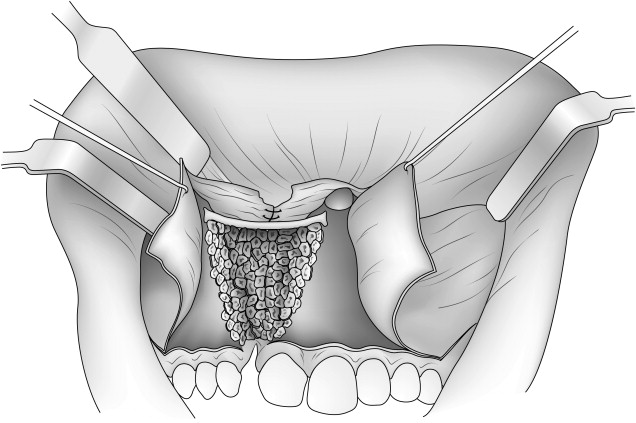
Attention is first given to developing soft tissue flaps to reconstruct the nasal floor, palate, and labial mucosa and attached gingiva. The initial incisions are planned to preserve adequate attached gingiva around the erupted teeth and permit the advancement of attached gingiva into the area of future tooth eruption (see Fig. 1 ). In the region of the molar teeth, this incision is carried superiorly posteriorly into the free mucosa and sulcus approximately 1.0 to 1.5 cm to permit relaxation for advancement of this flap. This is completed bilaterally.
Incisions are next made along the outer margins of the bony cleft and carried superiorly into the depth of the vestibule. While making these incisions along the cleft margin, the underlying bone is palpated with an instrument to ensure that the incisions remain over bone. At their superior extent in the depth of the vestibule, each of the incisions becomes horizontal and extends laterally approximately 1.0 to 2.0 cm from either side of the cleft (see Fig. 1 ).
Beginning inferior-medially, the mucoperiosteal tissues are undermined subperiosteally off the outer aspect of the alveolus and anterior maxilla along the entire length of both cleft margins. Medially, this dissection is carried until the anterior nasal spine and the floor of the contralateral (noncleft side) nasal floor are identified. Laterally, the dissection is carried superiorly on the maxilla to the level of the infraorbital neurovascular bundle (see Fig. 1 ).
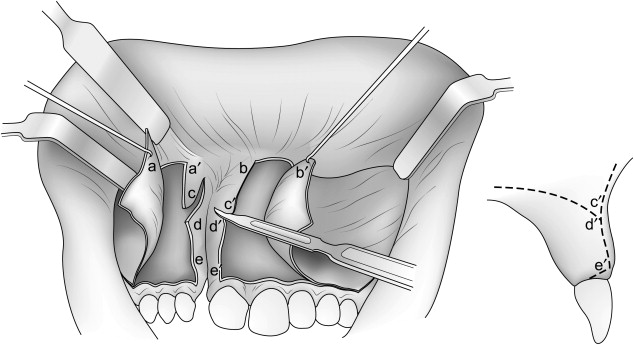
Once the labial subperiosteal dissections are completed, the remainder of the soft tissue incisions and flaps necessary to reconstruct the floor of the nose and palatal aspect of the osseous defect are developed. Two additional incisions, following the palatal plane posteriorly approximately 15 mm, are made on each side of the margin (c–d and c′–d′; see Fig. 1 ). Next, the subperiosteal dissection is extended into the defect on both sides of the bony cleft, beginning inferiorly and proceeding posteriorly. The lateral dissection is extended well up the lateral nasal wall superiorly, and the medial dissection is extended to the base of the cartilaginous nasal septum.
In the final development of the soft tissue flaps to reconstruct the nasal floor and palate, it is important that the flaps extend well into the nasal cavity and onto the horizontal portions of the palatal shelves. This helps to ensure that adequate bony reconstruction of the alveolus and anterior maxilla can be achieved by the subsequent bone grafting. This can often be accomplished from the labial aspect, except when the bony cleft is quite small or narrow. In these instances, their full development needs to be accomplished from a palatal approach.
The superior flaps are sutured to reconstruct the nasal floor ( Fig. 2 ). The inferior flaps are sutured to establish continuity of the palatal soft tissue and can often be sutured from the labial aspect, especially when the bony cleft is wide, rather than from the palatal aspect. Ideally, horizontal mattress sutures are placed to maximize raw tissue interphase, and thereby reduce the risk for dehiscence and secondary healing. When the tissue release or suturing is to be done from the palatal approach, inserting and using a Dingman mouth prop may aid in visualization.
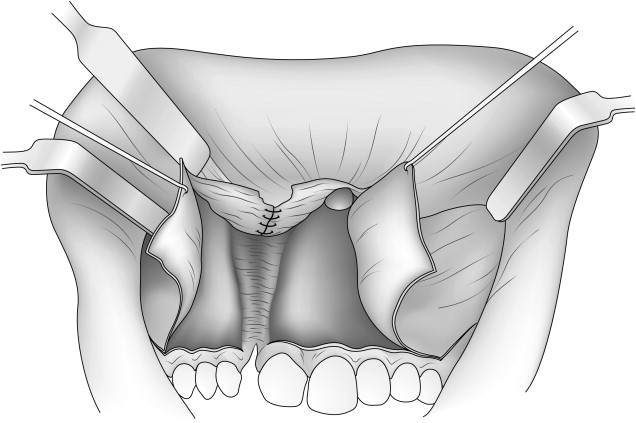
The bony reconstruction must be precise to achieve a good result (piriform fullness and alar base support) and to permit orthodontic movement of the adjacent teeth into the reconstructed alveolus ( Fig. 3 ). The nasal floor is reconstructed by firmly wedging a cortical cancellous strut, sculptured to the correct shape, between the alveolar margins of the cleft, slightly superior to the contralateral nasal floor, which was previously exposed. Autogenous cancellous bone is the ideal material to fill the bony cleft. Also, it is best to compact this graft before placement. This can be achieved by placing the graft in a 10-cc syringe and compressing it with the plunger. Following this, it can be delivered by cutting of the most distal end of the syringe with a blade.