Alloplastic temporomandibular joint (TMJ) reconstruction is an entirely biomechanical rather than biologic solution to severe and debilitating anatomic joint disease. Modern reconstructive orthopedic surgery would be unthinkable without the availability of alloplastic total joint prostheses. In the 1960s, posed with the problem that resection arthroplasty was an uncertain procedure with common complications such as recurrent deformity and limited motion, Sir John Charnley developed a successful low-friction total joint replacement (TJR) device. Since that time, with the evolution of surgical techniques, implant materials, and designs, excellent long-term function and improvement in quality of life have been reported, along with device survival rates exceeding 90% after 10 years.
Based on evidence from the orthopedic, biomedical engineering, and oral and maxillofacial surgery literature, this chapter discusses the role that total alloplastic reconstruction can play as salvage in the management of patients with severe and debilitating anatomic TMJ disorders to improve mandibular function and overall quality of life.
Etiopathogenesis/Causative Factors
The following are the presently accepted indications for TMJ TJR :
- 1
Inflammatory arthritis involving the TMJ that is not responsive to other modalities of treatment
- 2
Recurrent fibrosis or ankylosis (or both) not responsive to other modalities of treatment
- 3
Failed tissue grafts (bone and soft tissue)
- 4
Failed alloplastic joint reconstruction
- 5
Loss of vertical mandibular height or occlusal relationships (or both) because of bone resorption, trauma, developmental abnormalities, or pathologic lesions
Pathologic Anatomy
Severe pathology associated with mandibular dysfunction and anatomic distortion of the TMJ complex dictates the need for TJR. Because of the multifaceted composition of the TMJ complex and its reliance on coordinated masticatory muscle function, it is an unreasonable expectation that a reconstructed TMJ can be returned to its “normal” premorbid function. Thus, there will always be some functional disability involved in any reconstructed joint, either autogenous or alloplastic.
In a multiply operated patient with an anatomically distorted joint reconstruction, chronic neuropathic pain will be a major component of that patient’s disability. Therefore, it is important for both the surgeon and the patient to understand that the primary goal of any type of TMJ reconstruction is restoration of objective mandibular function and form. Any subjective pain relief gained must be considered only of merely secondary benefit.
Pathologic Anatomy
Severe pathology associated with mandibular dysfunction and anatomic distortion of the TMJ complex dictates the need for TJR. Because of the multifaceted composition of the TMJ complex and its reliance on coordinated masticatory muscle function, it is an unreasonable expectation that a reconstructed TMJ can be returned to its “normal” premorbid function. Thus, there will always be some functional disability involved in any reconstructed joint, either autogenous or alloplastic.
In a multiply operated patient with an anatomically distorted joint reconstruction, chronic neuropathic pain will be a major component of that patient’s disability. Therefore, it is important for both the surgeon and the patient to understand that the primary goal of any type of TMJ reconstruction is restoration of objective mandibular function and form. Any subjective pain relief gained must be considered only of merely secondary benefit.
Diagnostic Studies
A detailed history and head, neck, and oral examination, including evaluation of the occlusion and any oral orthotic devices that the patient has been using, are important. This should be followed by a careful review of any previous imaging (plane films, magnetic resonance imaging, computed tomography) available to determine the need for further imaging to correlate any findings with the chief complaint, history, and clinical examination.
Appropriate laboratory studies may be required, such as in patients suspected of having high inflammatory arthritic disease.
Unmounted and mounted study models are helpful in determining compensatory changes in the occlusion that may necessitate orthodontic management before reconstruction. Severely compromised occlusal or skeletal relationships (or both) must be considered and planned for correction because they will affect mandibular stability after reconstruction and the longevity of alloplastic devices as a result of abnormal wear forces.
Past and recent clinical photographs are helpful in determining the onset of conditions such as unilateral condylar hyperplasia/hypoplasia and apertognathia associated with pathology or previous TMJ surgery.
Present and previous medical and dental records can provide useful information in preparing for future reconstructive surgery and anesthesia, especially in patients with a long history of narcotic use for controlling pain or management in a pain clinic.
If there is any concern regarding the patient’s preoperative psychological state, thorough evaluation by a psychologist or psychiatrist familiar with patients with TMJ disorders is essential before any reconstruction is undertaken. Unrealistic expectations of pain control and functional or esthetic results must also be considered and dealt with accordingly.
Presurgical Considerations
Presurgical diagnostic local anesthetic (without vasoconstrictor) blocks of the joint or masticatory muscles (or both) may be performed to try to determine the cause of the pain, as well as to demonstrate the concept of centrally mediated pain to the patient.
Presurgical use of botulinum toxin or muscle relaxants and physical therapy such as ultrasound can be considered, but to date no studies have provided any data that these treatments are helpful in decreasing postoperative masticatory muscle pain in such cases.
Treatment/Reconstructive Goals
Regardless of whether the TMJ is reconstructed with alloplastic, allogeneic, or autogenous material, the following should be the management goals :
- 1
Improve mandibular function and form
- 2
Reduce suffering and disability
- 3
Contain excessive treatment and cost
- 4
Prevent morbidity
Specific Treatment and Techniques
Inflammatory Arthritis Involving the Temporomandibular Joint that is not Responsive to Other Modalities of Treatment
Since inflammatory arthritis involves a local synovial-mediated destructive systemic disease process and complete synovectomy cannot be achieved, the orthopedic literature opts for TJR in these cases because the results are very predictable.
In the TMJ, alloplastic reconstruction has been discussed at length. All of these authors agree that when the mandibular condyle is extensively damaged, degenerated, or lost, as in arthritic conditions, replacement with either an autogenous graft or alloplastic implant is an acceptable approach to achieve optimal functional and symptomatic improvement.
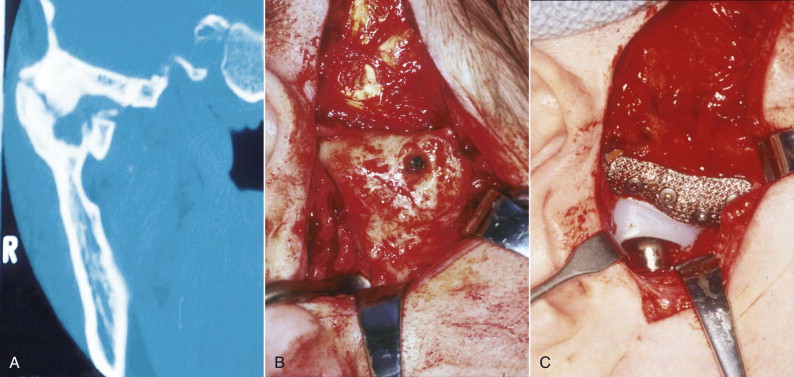
However, dissatisfaction with some of the facets of autogenous costochondral grafting, particularly in patients with high inflammatory arthritic disease (e.g., rheumatoid arthritis) ( Fig. 100-1 ) and resultant ankylosis, led to the development and use of TMJ TJR devices, and data can be evaluated to support good results with such treatment.

Recurrent Fibrosis or Bony Ankylosis not Responsive to Other Modalities of Treatment
The traditional management of complete bony TMJ ankylosis has been gap arthroplasty with an autogenous tissue graft or alloplastic hemiarthroplasty reconstruction ( Fig. 100-2 ). Although autogenous grafting techniques develop form, mandibular function is typically delayed. Since graft mobility during healing will compromise its incorporation into the host environment or compromise its blood supply, early mandibular mobility often leads to graft-host interface failure and a high incidence of recurrent ankylosis.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses