Implant site development through orthodontic extrusion can regenerate hard and soft tissue volumes lost to periodontal disease. This extrusive procedure is indicated especially when a maxillary incisor is severely compromised and the esthetic demands are high. This article describes a novel approach to alveolar bone development that enhanced the volume of the implant site. The technique involves tipping the maxillary incisor in the direction of the angular defect to increase alveolar bone volume in the implant site; simultaneous improvement of the interproximal papillary height can also be expected. With this procedure, immediate loading of the endosseous implant is possible due to the quality of the bone developed.
Alveolar bone development before the placement of an endosseous implant can be accomplished through the slow orthodontic eruption or “extraction” of a severely periodontally compromised tooth. This procedure is particularly useful when a maxillary incisor is compromised. Because the maxillary incisor is in an important esthetic zone, this method generates tissues that are sufficient to mimic the contralateral incisor and maximizes the development of hard and soft tissue contours. With a light, continuous orthodontic force applied, the tooth is slowly brought incisally along with its gingival attachment and alveolar bone, improving the surrounding bony architecture.
The success of an endosseous implant depends on adequate soft and hard tissue volumes in the recipient site. As the compromised tooth is erupted, the cross-sectional area of the root is reduced because of its conical shape. As a result, bone fill is deficient, since the root’s capacity of regenerating bone is limited in the mesiodistal and buccolingual directions. To circumvent this problem, Zuccati and Bocchieri described a procedure to increase the buccolingual width of the ridge development by purposely torquing the root labially as the orthodontic eruption is advanced. An alternative to this method is tipping the incisor to maintain adequate buccolingual and mesiodistal widths of the remnant root. In addition, the tipped root fragment might have the potential of developing the papilla lost to periodontal disease. This case report describes the forced eruption concurrent with tipping of the remaining root fragment of a maxillary left central incisor with a severe alveolar bone defect in the mesial aspect. The full treatment plan included replacement of this tooth with an endosseous implant.
Case report
A 30-year-old woman was referred by a periodontist for an orthodontic consultation, and a significant angular defect was found on the maxillary left central incisor. A significant deepbite was noted during the intraoral examination, as well as a Class II end-on molar occlusion on the right and a Class I occlusion on the left. From the frontal view, the patient displayed uneven gingival heights in the anterior region with mild recession on the maxillary left central incisor and open gingival embrasures in the anterior maxillary region ( Fig 1 ).

The periodontal examination with the periapical full-mouth series ( Fig 2 ) showed generalized moderate periodontal disease. Angular bone defects were limited to the mandibular first molars and the maxillary central incisors. The magnitude of the bony defects of the mandibular molars was mild; however, the angular defect in the mesial aspect of the maxillary left central incisor was severe, extending to the apex. The severity of the osseous angular defect in the maxillary left incisor was of concern but not directly related to the microbial plaque observed, suggesting that a genetic predisposition might have contributed to the progression of the disease.
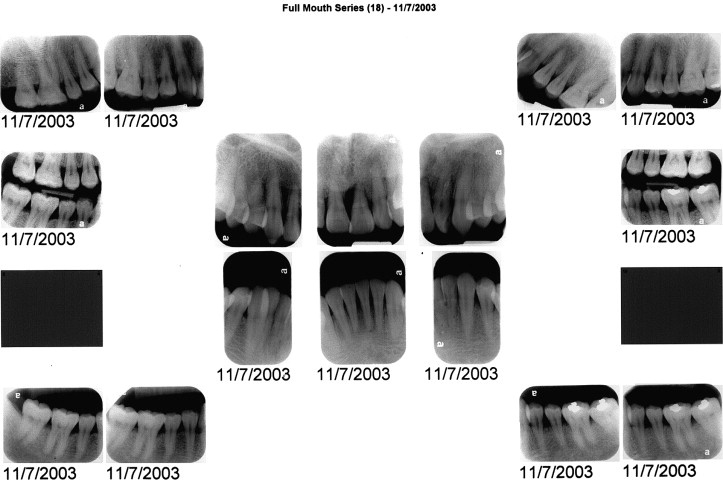
The distal aspect of the maxillary left central incisor and the mesial and distal aspects of the maxillary right incisor had lost approximately 60% of the angular bone. The clinical examination also showed mild to moderate crowding in both arches and increased mobility in the maxillary left incisor.
Cephalometric analysis confirmed a straight soft and hard tissue profile with short lower facial height and a reduced mandibular plane angle. Maxillary incisor display at smile was 100%, and the maxillary incisors were slightly retroclined.
The primary treatment objective for this patient was the regeneration of adequate height and width of the alveolar bone and gingival tissue lost to periodontal disease in the maxillary anterior region. The site would be used for an ideal 3-dimensional placement of an endosseous implant to support a prosthetic restoration for the maxillary left central incisor.
The specific orthodontic objectives were to maintain the maxillary incisal edges and relieve the crowding by distalizing the maxillary right canine, thereby finishing in a full-cusp Class II molar occlusion on the right and a Class I on the left. The mandibular arch was to be aligned through approximately 2 mm of incisor flaring. In the vertical dimension, the objective was to absolutely intrude the anterior teeth from canine to canine to correct the overbite. The incisal edges of the maxillary incisors were to be maintained as well as the patient’s skeletofacial and soft-tissue drape.
The treatment alternatives for the localized periodontal problem were the following.
- 1.
A thorough debridement with gingival tissue regeneration procedures. This would address the disease and result in possible bone deposition and attachment gain. Although some alveolar bone gain would be expected, the extent of regeneration would be limited and most likely result in approximately 50% of root coverage. Additionally, the gain in gingival tissue height, with the obvious esthetic benefits, would probably be negligible.
- 2.
Extraction of the maxillary left central incisor and extensive debridement and grafting to gain alveolar bone height and width. The advantage of this procedure would be that the site could be ready for implant placement in a shorter time, compared with an orthodontic forced-eruption approach. However, the occlusal relationship in the form of a deepbite was not favorable to receive an implant, and its placement would need to be delayed until intrusion of the mandibular incisors was accomplished. Two other disadvantages of this tripartite approach were the unpredictability of soft-tissue gain and the need for additional surgical procedures before the endosseous implant placement.
- 3.
Eruption of the maxillary left central incisor after debridement of the anterior region in conjunction with periodontal maintenance visits every 3 months. The advantages of this option were both esthetic and functional. Functionally, a greater amount of bone could be obtained in both height and width for an ideal implant site. Esthetically, the gingival tissue would follow coronally, thereby matching the contralateral tooth and achieving optimal soft-tissue contours. Furthermore, tipping the root apex of the maxillary left central incisor in a mesial direction toward the right central incisor would have the added benefit of potentially restoring the papilla lost to periodontal disease in the mesial aspect. A larger surface area of the periodontal ligament would remain with this method, and, as a result, increases in bone width and height would be achieved. In contrast, the direct vertical eruption of the incisor limited the beneficial influence of the periodontal ligament because of the reduced surface area.
The periodontist who referred the patient had performed a thorough scaling and root planing procedure by quadrants before the orthodontic consultation. The patient had also been placed on a 3-month recall schedule. The treatment was divided into 2 phases: the first phase involved eruption of the maxillary left central incisor and intrusion of the mandibular anterior segment. The second phase involved extraction of the maxillary right first premolar and space closure. An endosseous dental implant was to be immediately placed after orthodontic treatment.
The first phase started with two 0.022-in preadjusted double tubes bonded to the maxillary first molars and a bracket bonded to the maxillary left central incisor. An 0.018-in stainless steel archwire with an extrusive activation force of approximately 20 g was extended to the central incisor from the molar tubes. A 0.022-in slot preadjusted appliance was bonded to the mandibular first molars and premolars. A 0.020-in stainless steel wire segment was bonded directly, without brackets, from the right lateral incisor to the mandibular left canine ( Fig 3 ). Brackets were not placed in this region to prevent potential occlusal interference with the maxillary incisors, particularly in this patient, whose maxillary left incisor was being extruded as the mandibular incisors were being intruded.

Two 0.017 × 0.025-in stainless steel segments were placed in the mandibular buccal segments from the first molar to the first premolar. An intrusion arch made of .020-in titanium-molybdenum alloy was extended from the auxiliary tubes of the first molars to the mandibular anterior segment and tied mesially to the lateral incisors.
As extrusion in the maxillary left incisor was accomplished, the incisal edge was adjusted for esthetic reasons. After significant tooth eruption, elective endodontic treatment with calcium hydroxide was performed on this tooth to continue the eruptive process ( Fig 4 ). Incisal and lingual tooth structure reduction was needed as the tooth erupted.





