Chapter 9 The Orthodontist’s Role in MDI Therapeutics
ORTHO Transitional Anchorage Devices (TADs) and Related Applications
Introductory Background by Dr. Victor Sendax
As a prime center for orthodontic research, University of Oklahoma has contributed the following section as a review of its research and clinical perspectives on temporary anchorage devices (TADs) for the orthodontic domain:
Introduction to Anchorage and Biomechanics
The use of anchorage is important in orthodontic biomechanics. Root lengths, shapes, and surface areas help differentiate teeth that resist tooth movement.67 Reciprocal effects influence the teeth that do not have direct forces applied, and collateral effects are secondary involving the teeth to which the force is applied.
Extraoral anchorage is the oldest anchorage system in contemporary orthodontics and includes both facebow and J-hook headgears in Class II correction or anterior retraction compared with the facemask, which is used in maxillary protraction for cases of Class III maxillary deficiency problems. The application of headgears is usually labeled as occipital anchorage whether it involves high, straight, or low pull. The neck strap is related to the low pull headgear, which can be identified as the Kloehn type that was introduced in the 1940s.36
There is no doubt that temporary anchorage devices (TADs) can revolutionize the treatment mechanics in orthodontics. Complicated movements such as molar intrusion, arch intrusion, and retraction of anterior teeth or protraction of posterior teeth without reciprocal movement of the reactive units have previously been managed through various types of modified force systems, such as the manipulation of moment arms, pitting anchorage units with greater resistance against the tooth or teeth to be moved.31 An important biomechanical aspect in the use of TADs is related to the direct application. Forces are different than moments. A moment is the tendency of a force to rotate an object about a point. Therefore, in orthodontics, forces are linear but moments circular. Couples are force systems separated by a distance and have equal and opposite vectors (i.e., edgewise brackets). Both couples and moments created in conventional retraction and protraction mechanics are not present when direct anchorage methods are used with the TADs. The TADs will not create any counteracting moments to cancel those in the active unit, which the anchorage teeth (reactive units) would create with conventional biomechanics. Because of this, when planning anchorage with TADs, clinicians should evaluate the mechanical setup carefully to understand the lack of reciprocal effects on the teeth. Basic biomechanical considerations still apply. Application of a force vector that does not pass through the center of resistance (biologic entity at furcation of multirooted teeth or one third the distance from the cementoenamel junction to the root apex in single-rooted teeth) still results in rotational movements. Centers of rotations, however, are defined by the moments about them and their resistance. Again, for every action there is an equal and opposite reaction. What changed with TADs was where the equal and opposite reactive forces occurred.31 The reactive forces with TADs are dissipated in the skeleton. Knowing this not only changes the mechanics but, in fact, directs the clinician to greater attention in the biomechanical planning of the particular case.
Using various lever arms, one can control the point of force application and achieve desired intrusive or extrusive effects during retraction according to the patients’ needs.52,55
In a series of articles by Cornelis et al.8 and De Clerck et al.,12,13 the biomechanical considerations in extraction versus nonextraction cases and intrusion mechanics were discussed. Although these authors focused on using mini plates, the same principles can apply to the mini screw TADs. They noted that regardless of the appliance used, the undesirable frictional forces may actually help correct the overjet in the early stages of treatment, thus reducing overall treatment time. In conventional sliding mechanics without TADs, permanent canines are distalized with elastics between the permanent canines and molars. The compensating moments are generated and cancel each other out, thus resulting in canine distalization with minimal overjet correction. However, if the TADs are used as the direct form of anchorage and if there is no contact between the maxillary and mandibular permanent incisors, the resulting force from the archwire will retract the four maxillary permanent incisors distally, thus reducing the overjet and the total treatment time. The authors also discuss the faciolingual aspect of the posterior teeth. The rotational moment of the reactive unit is again not present with TADs. The only moment is on the permanent canine, and it is not being neutralized. Therefore the arch wire will keep tilting, causing a crossbite on the distalization side of the canine. To prevent this, a transpalatal bar is recommended. These devices may also be used when intruding the posterior teeth in the maxillary arch, similar to a fixed lingual arch in providing control for intrusion of the mandibular posterior teeth. Some clinicians suggest the use of palatal TADs for better control on the maxillary permanent molars during intrusion.
Immediate loading of the TADs has been under investigation for more than a decade. Current literature is inconclusive whether the clinicians should immediately load the TADs. However, immediate loading seems to be acceptable with reduced forces.45,46,9 These light loads are between 25 and 50 grams.
Owens et al.48 evaluated the stability of TADs in relation to the timing, amount, and location of force application. They tested 56 TADs on skeletally mature male beagle dogs. The maxillary TADs were divided into two groups of immediate loading and delayed loading. In the mandible all the TADs were immediately loaded. The experimental TADs had a corresponding unloaded control. They presented an overall success rate of 93% with no significant effects of timing, amount, or location of force applied. No correlations were reported between the timing of force application and the success rate.
Temporary Anchorage Devices
The application of skeletal anchorage devices in orthodontics currently has come from the extensive use of skeletal implants used in restorative dentistry. These osseointegrated devices have directed dentistry in new directions from surgical management through the restoration of the implants. These changes include input from general dentistry, oral surgery, and periodontics. The application in orthodontics has included osseointegrated bars and screws as well as onplants.60–633 The trend is toward screws that are not osseointegrated for bony anchorage that make tooth anchorage more strong, either in an indirect or direct manner.
Many articles have been published describing this novel method of attaining seemingly absolute anchorage, especially after Kanomi’s 1997 article,30 which gave rise to the modern TADs that are being used today.
The traditional implants as skeletal anchorage have not reached wide-spread use in orthodontics for several reasons. The traditional implants used in dentistry, such as the Brånemark system, have limitations that make their use in orthodontics problematic. These implants are often too large to be placed in convenient places, remain costly, and require a fairly invasive surgical procedure, followed by extended healing time.6 These limitations have spurred a number of innovative implant designs and sizes in recent years.
Much has improved since the introduction of TADs in 1945 by Gainsforth and Higley15 from the University of Iowa. They were the first investigators who thought it was time to investigate alternative anchorage resources in orthodontics and tried using the basal bone with an animal model. They were inspired by a series of surgical techniques described in Shaar and Kreuz’s 194363 text Manual of Fractures. Vitallium, being the most biocompatible and inert alloy at the time, was the choice of material for the screw hooks. Their screws were 13 mm in length with a diameter of 3.4 mm. They were placed in the ramus immediately distal to the last molar. Maxillary canines were banded in each of the six dogs, and four of the dogs had an orthodontic appliance using an elastic that stretched from the implant to a jig in the maxillary arch and then to the maxillary canine for orthodontic traction. The remaining two dogs served as controls with no traction forces applied on their teeth. Placement of the implants occurred under general anesthesia using sterile techniques. The implants were immediately loaded after placement with an elastic force of 140 to 200 g. Although the hope for basal bone anchorage existed, their results were not supportive of the idea. None of the screws stayed more than 31 days, but the teeth moved a few millimeters with minimal anchorage loss, which was not enough to inspire the profession.
After Gainsforth and Highley’s unsuccessful attempt, further research into skeletal anchorage in orthodontics was limited for some time. More than 20 years later, Linkow of New York published the next article on the subject of implants and their usage as skeletal anchorage units in orthodontics in 1969.41 His article described the use of an endosseous blade implant in orthodontics. These implants had been successfully used in dentistry for several years before his report, but the orthodontic community was relatively skeptical of the ideas brought forth by Linkow. One year later, Linkow40 published a follow-up article in 1970 that established his position in the development of implants in orthodontics. He noted that most of the emphasis in implantology to that time was placed on perfecting implant design and techniques. He added that several years of proven success made it possible to broaden the range of implant applications, and he advocated implant use as an adjunct to conventional orthodontic therapy. In this article he listed problems that could benefit from the use of endosseous implants. The six cases that Linkow selected were patients with missing teeth or with teeth that were lost in the course of orthodontic treatment. The implant functioned to replace these missing teeth, either to maintain space or as anchorage on which the force systems were applied directly to the restored implant. He argued that implants could be used to prevent drifting of teeth and act as an anchorage point. Linkow asserted that implants could eliminate the need for extraoral anchorage devices.
The transition into a more contemporary look for the implants took another 13 years. Creekmore and Eklund10 presented a case report of a 25-year-old woman. This was the first temporary anchorage device placed specifically to aid orthodontic mechanics and had a screw type design. The investigators placed a Vitallium bone screw just below the anterior nasal spine and used a light elastic thread to it, on which they attempted to intrude the maxillary incisors to correct her deep bite. They were able to intrude and torque the maxillary central incisors with the help of the screw. The Vitallium screw remained stationary for a year until the mechanics were completed. They posed the question “Might skeletal anchorage be applied to orthodontic tooth movement and orthopedic jaw movement?” In the same year, the stability of the Vitallium screws was confirmed on a histologic animal model by Gray et al.19
The advances in biomaterials introduced titanium to dentistry. After the report1 of the American Dental Association (ADA) Council on Scientific Affairs in 1996, the use of endosseous implants increased. The ADA accepted the use of both pure titanium and titanium alloy implants. Although the clinical data for long-term success of the endosseous implants is still lacking, titanium has been used for more than 25 years and used for both endosseous and subperiosteal implants in many different forms such as rods, posts, blades, and finally mini screws. The process of living tissues becoming structurally and functionally connected with the oxide surface of the body of the implant is called osseointegration. This process is necessary for the prosthodontic use of implants. However, it is not a requirement for a successful application of an orthodontic mini screw. Although a recent report34 promotes the need for partial osseointegration for orthodontic mini screws, it may complicate their removal as temporary anchorage devices and may not be widely accepted under the presence of numerous successful clinical studies.
In the late 1990s, the contemporary designs made with pure titanium and titanium alloys were introduced, and clinical trials were initiated. In 1995 Block and Hoffman3 introduced the “onplant” and evaluated possible palatal applications. They used a design that measured 10 mm in diameter and 2 mm in height. The implant itself was a disk with one side textured in addition to a hydroxyapatite coating. On the opposite side, it had an internal thread for attachments. The onplant resided on the surface of the palatal bone, and after osseointegration, it could withstand enough force to be used for orthodontic anchorage. The onplant was tested in both animal and human models and proved safe and effective for intraoral anchorage. However, its use resulted in limited acceptance due to a large surgical flap on the palate for both placement and removal.
The palatal trend has been similar to facial applications whereby the initial versions were endosseous and later were being replaced by mini screw type, nonosseointegration TADs. Wehrbein et al.69 introduced an anchorage setup through a transpalatal bar for en masse retraction of maxillary anterior teeth. It was done without the use of compliance-dependent appliances such as headgear or elastics. They reported a mean anchorage loss of 0.7 mm on the right side and 1.1 mm on the left side.
Numerous studies have been published investigating the possibilities of using palatal TADs either by assisting holding arches or by assisting intraoral distalization appliances in an indirect manner. In 1997, Kanomi30 reported using miniscrew for anchorage in an intrusion case. His work initiated the concept of modern TADs. In 1998, zygoma ligatures were proposed as an option for maxillary anchorage.47 In 1999 Umemori et al.68 discussed skeletal anchorage systems and titanium miniplates for correction of open bites.
Biological Considerations
A number of studies in the dental literature look at osseointegration and bone remodeling around the endosseous implants. Huja et al.23–25 studied bone adaptation and response to TADs.
In their studies, they looked at the effect of micro cracks in the bone caused by the insertion of the TADs. Their results indicated that regional bone turnover was elevated. The increased rates noted were 100% to 200% recorded during the healing period of 6 to 12 months. This was in contrast to normal cortical bone turnover rate, which was 2% to 20% per year.24 The authors called this phenomenon a localized bone adaptation response.
Indications and Applications
The first study20,21,22 investigated the retraction of maxillary permanent canines.
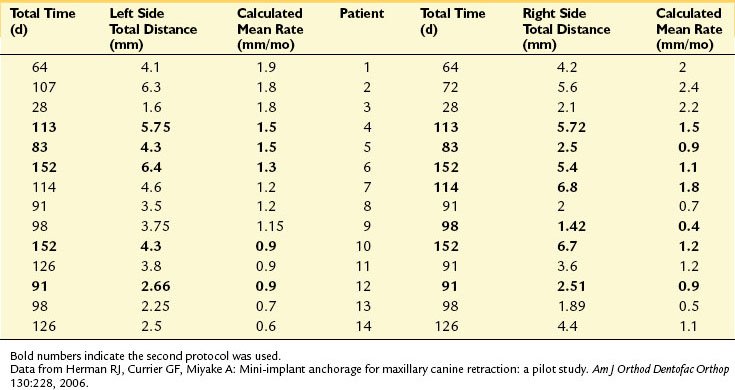
The study22 comprised 16 subjects who had maxillary first premolars extracted. TADs were placed between the roots of the maxillary permanent first molars and the second premolars by one oral surgeon. All retraction was accomplished on 0.017 × 0.025-in stainless steel archwires in 0.022-in slots by using nickel-titanium springs stretched from the implant head to the brackets on the permanent canines. Because this was the first study completed in the department, investigators tested different placement protocols. In the first protocol, the investigators used a noninvasive protocol. However, it resulted in the loss of 51% of the implants (19 of 39); the second protocol required a small flap surgery and resulted in 100% stability (10 of 10). The calculated monthly canine retraction rates varied widely from 1.5 to 6.1 mm per month (Table 9-1). The researchers also noted excessive crown tipping into the extraction spaces in four of the 28 retracted canines, and this was related to the method of ligation of the canine to the archwire. They were able to preserve anchorage and concluded successful results in canine retraction.
The second study60 evaluated en masse retraction of the mandibular incisors and retraction of mandibular permanent canines in selected cases. The sample contained 10 patients who had mandibular first premolars extracted for orthodontic treatment. TADs were placed laterally in the mandibular alveolar ridge between the roots of the permanent first and second molars by one oral surgeon. TADs were ligated to the bracket of the mandibular permanent first molars, providing indirect anchorage for retraction of the mandibular anterior teeth. All patients were treated with the 0.022-in slot Damon 2 appliance (Ormco, Glendora, CA). En masse retraction of the mandibular anterior teeth (n = 7) was accomplished on 0.019 × 0.025-in stainless steel archwires, and in certain cases canine retraction (n = 3) was accomplished on 0.018-in HiTi stainless steel archwires using nickel-titanium springs stretched from the mandibular permanent first molar brackets to anterior hooks soldered to the archwire or to the hooks on the canine bracket during en masse or canine retraction, respectively. Monthly rate of retraction was calculated for each mandibular canine. In the en masse retraction group of seven, total mean retraction for the canines was 0.61 mm per month with an arch length change of 0.56 mm per month. The canine retraction group of three demonstrated a total mean retraction rate of 1.75 mm per month for the canines. Overall, the reported retraction rates seemed appropriate compared with the findings of similar studies. Stability of the implants was reported to be very good, and results indicated minimal anchorage loss and good vertical control of the mandibular posterior dentition.
Similar findings from both studies were as follows: the soft tissue reactions were excellent; patient acceptance and tolerances were reported to be very high; and the Ortho Implant proved to be an effective TAD in the posterior maxilla or mandible to assist in retracting maxillary or mandibular anterior teeth (Table 9-2). After serving as anchorage devices, the implants were easily removed without any complications in both studies.
TABLE 9-2 Preliminary Summary of the Combined Data From Three Studies on Soft Tissue Health, Stability of TADs, and Patient Acceptance
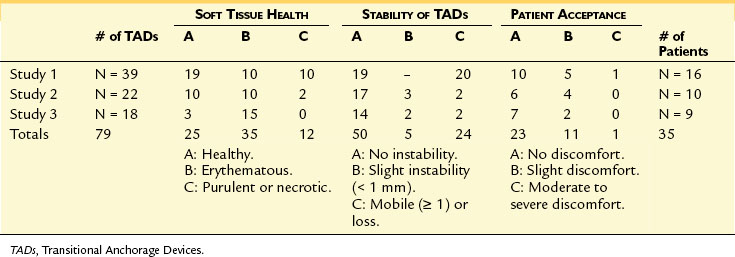
The third study investigated the skeletal, dental and soft tissue changes with Forsus fatigue resistance appliance with and without TADs.27 Forsus appliances are fixed functional appliances used to correct Class II malocclusions. As they assist in correcting the Class II malocclusion, they tend to move the mandibular teeth forward, particularly the anterior ones, resulting in anchorage loss. The TADs were used to prevent this side effect from these fixed functional appliances. The stability, soft tissue health, and patient acceptance of TADs were also evaluated similar to the previously completed studies. A total of 20 patients in the permanent dentition, between 11 to 17 years of age, with Class II or end-on-end molar relationships and with an indication for nonextraction orthodontic treatment were randomly selected to participate. MBT prescription low profile Victory/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses