9
Restorative appointments
People with developmental disabilities/disorders (DDDs) generally present with increased oral health problems compared to the general population. For this reason, it is important to focus on each patient’s specific needs in order to achieve optimal oral health. No two persons are alike, not even twins! It is extremely important to keep this in mind, especially when treating individuals with DDDs. Improving the oral health of a person with DDDs may be slow at first, but determination and communication can bring positive results.
Unfortunately, most academic programs in dental schools worldwide advocate the use of general anesthesia for patients with DDDs and fail to consider behavior management/guidance as a viable option when treating these individuals. General and pediatric dentistry programs have shifted from a clinic-based operation to more of a hospital-based perspective, referring patients with DDDs directly to the hospital’s operating room without assessing the behavioral situation, therefore increasing barriers to a more appropriate treatment: behavior management/guidance.
SETTING UP FOR SUCCESS
Providing oral health care services to patients with DDDs requires an adjustment of our everyday skills, as some DDDs such as autism spectrum disorders (ASDs), cerebral palsy, Down syndrome, and intellectual disabilities (IDs) can affect the mind, the body, and the skills of thinking, talking, and self-care. Those inflicted need extra help to achieve and maintain good oral health. It has been established that those with chronic medical illnesses, developmental disabilities, and psychosocial issues experience more oral health care problems than others who do not suffer from these conditions (Havio 1995; Feldman et al. 1997; Waldman et al. 2000).
Knowing the background of your target population, in this case DDDs, will enhance your possibilities of success in presenting an adequate treatment plan and subsequent successful restorative appointments. The dental team may be inattentive to communication styles, but the patient and his or her parents are not (Hall et al. 1987). These relationship and communications problems have been shown to play a prominent role in initiating malpractice actions (Lester & Smith 1993).
STRATEGIES FOR CARE
The optimum development of correct attitudes will give us a correct approach to an effective dental restorative treatment for patients with DDDs.
Knowing your patient´s developmental disability/disorder
Before the restorative appointment, make sure you have reviewed DDDs and the different manifestations and possible complications. Consult the patient’s physician, family, or caregivers to achieve an accurate medical/dental history. Specific questions regarding the disability of the patient will provide valuable information about the patient’s level of function and will help us identify the patient’s support system. The disability may require adjustment of the patient’s position in the dental chair, as those individuals with congestive heart failure, asthma, high-level spinal cord injuries, cerebral palsy, and/or swallowing difficulties will require a more upright position.
To properly treat patients with DDDs and, if necessary, refer them for appropriate medical care, dental professionals must be able to recognize the signs and symptoms of each patient’s specific disability (Raposa 2009).
Medications used to treat cardiovascular, psychiatric, chronic respiration, and other disorders may interact with dental agents, including anesthetics, vasoconstrictors, and sedatives; therefore these agents may be avoided or used with extreme caution and medical supervision.
Most people with DDDs can be treated successfully in the general practice setting with few procedural alterations. It is important to introduce the patient to the staff and setting before placing him or her in a hospital operating room. If placed immediately, it will only indicate, in our opinion, a clear refusal of treatment. There is no need for a specialty degree to perform operative work on a patient who is sleeping and controlled; some knowledge of general anesthesia and the hospital setting protocols will suffice.
In the 30-year clinical and academic practice of one of the authors of this chapter (FGG), general anesthesia has been used for only very profound cases of patients with DDDs. Behavioral techniques have generally proved adequate in the dental office and university environment. Transferring these patients to the hospital environment risks the “labeling” of patients with DDDs. Complete knowledge of the condition and effective communication will enhance your approach toward patients with DDDs.
During assessment, the dentist should consider not only the physical/medical risk for the individual but also social issues, which could help enhance patient as well as parent/caregiver satisfaction (Girdler & Hill 1988). Patient satisfaction, both during treatment and after care, is an important goal, and patients by right should have their concerns about care taken into account (Baker 1990).
Treatment planning
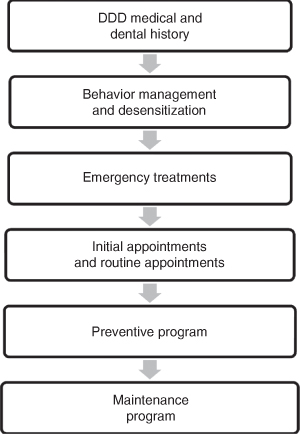
The ideal components of an accurate treatment plan in patients with DDDs have to include (Figure 9.1):
Figure 9.1 Ideal components of an accurate treatment plan for patients with developmental disabilities/disorders.
Potential dental or medical emergencies should be considered before any other dental treatment is considered.
Dental urgencies differ from dental emergencies in that they do not require immediate attention and are generally noted during routine patient examination (e.g., asymptomatic deep carious lesion).
The following can be considered as dental emergencies (Abbud et al. 2002; Mani et al. 1997):
Dentists who provide sedation service in their dental office should have the ADA documents and guidelines readily available (ADA 2000).
Determining medical conditions associated with aberrant behavior in patients with DDDs could be difficult. Effective communication will help ease this identification problem.
Pyles et al. (1997) described three very important ways to interpret some abnormal behavior:
RESTORATIVE TREATMENTS
Strategies for operatory procedures and biomaterials
Restorative treatments in patients with DDDs immediately uncover three issues that are the primary concerns of the clinician:
- Use of local anesthesia.
- Use of rubber dam.
- What is the best restorative material?
One of the issues that arises concerning the use of local anesthesia in patients with DDDs is lip biting. We have not seen any surprising adverse effects during regular dental treatments. When caries spots or infections are not deep or pulp-involving, we do not use local anesthesia in our patients with or without a DDD. When a patient is well oriented by behavior management/guidance, its use can be alleviated. When needed, a local anesthetic may be used with a shorter needl/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


