9
Operative treatment of dental caries in the young permanent dentition
J.A. Smallridge
Chapter contents
9.3.1 Important points in relation to treatment
9.3.2 Important points in relation to remineralization
9.9.1 Preventive resin restoration
9.9.2 Class I restorations in young permanent teeth
9.11.1 Extensive/deep caries in young teeth
9.11.2 Extraction considerations
9.11.3 Conservative treatment options
9.12 Treatment for hypomineralized, hypomature, or hypoplastic first permanent molars
9.12.1 Preformed metal crowns (stainless steel crowns)
9.13 Alternatives to conventional cavity preparation
9.13.3 Chemomechanical caries removal
9.1 Introduction
Caries is a chronic disease. If it starts to affect the permanent teeth the child patient is drawn into a cycle requiring ongoing care for the rest of his/her life. Therefore when treating the young permanent dentition we have to adopt an approach that considers and addresses the whole disease process and not just treat the outcome of the disease.
Caries is still a considerable problem in children and adolescents. The 2002–2003 British Association for the Study of Community Dentistry (BASCD) surveys which looked at dental disease levels in 77 693 14-year-old children in England and Wales (Pitts et al. 2004) found that, on average, half of the children examined had dentinal decay, with a mean of three permanent teeth decayed into dentine. Other studies have shown a low care index in UK children. The average care index for 11-year-old children is 41%, i.e. 59% of caries is left untreated, and in some parts of the country 80% is untreated. These children are at high risk of pain and discomfort relating to their teeth. Interviews with 8-year-old children showed that 47.5% had experienced toothache, 7.6% of whom had had pain in the previous 4 weeks!
Caries prevalence declined in the later decades of the twentieth century. As it dropped, a concentration of the disease occurred, with a small percentage of the population experiencing most of the disease. Caries prevalence is greatest in the occlusal surfaces of the first permanent molars and buccal grooves of the lower first molars, and the prevalence in these sites has dropped by the smallest proportion. The least susceptible sites are the approximal surfaces of the incisors, so if caries is seen in these permanent teeth you are dealing with rampant caries (Sheiham and Sabbah 2010).
The first permanent teeth erupt into the mouth at approximately 6 years of age, but may appear as early as the age of 4 years. The eruption of the anterior teeth usually causes great excitement, as it is associated with ‘the fluttering of tooth fairy wings’. However, the eruption of the first permanent molars goes largely unnoticed until there is a problem. The mean eruption time for first permanent molars has been determined as 6.1 years in girls and 6.3 years in boys, but there is a tremendous variation in both the time of eruption and the time it takes for the tooth to emerge into the mouth. It takes 12–18 months for a first or second molar to erupt fully.
The first permanent molars are teeth that commonly exhibit disrupted enamel; the reported incidences of defects range from 3.6% to 25%. The occlusal surfaces of these molar teeth account for about 90% of caries in children. The most rapid rise in DMFT rates occurs during late childhood and adolescence, a time when the enamel is still immature but when responsibility for oral hygiene and dietary choices is changing from parent to child. The rate of increase slows as young adulthood is reached.
Restoration of the young permanent dentition is part of a continuum and cannot be regarded in isolation. Restoration is only one small part of the child’s treatment. Essentially it is ‘surgery’ to remove the carious infected area of the tooth and insertion of a suitable substitute to restore the missing structure. It does nothing to cure the disease and must form part of a much wider treatment modality, which includes identification of the risk factors contributing to the disease followed by introduction of specific prevention counter-measures.
Effort must be applied in all of these areas to attempt to provide the optimum conditions for future tooth survival. The risk factors and preventive measures are addressed in detail in other chapters; this chapter will confine itself to appraisal of methods of treatment of caries in the young permanent dentition. It cannot hope to completely cover every aspect of operative treatment and there are other texts that the dentist should read to give a fuller account of the available techniques. However, the authors intend to give an outline of some of the options available.
9.2 Assessment of caries risk
Caries risk assessment is essential for producing a holistic dental management plan specific for the individual child. There are many questions to consider when planning treatment of caries:
• Is there caries?
• Is it into dentine?
• When to monitor?
• When to treat?
• What is the family attitude to teeth?
• What cooperation can you expect?
• Are they at low risk of further caries?
• Are they at high risk of more caries developing?
The idea of a caries risk assessment for each child patient is to ensure that the chosen diagnostic tests, preventive treatment, and any restorations are geared specifically to the needs for that individual patient. Factors requiring consideration are:
1. present caries activity
2. past caries activity
3. parent/sibling caries activity
4. sugar consumption (food and drink)
5. oral hygiene
6. fluoride exposure
7. tooth morphology
8. Streptococcus mutans levels
9. saliva characteristics, flow rate, and consistency.
Factors (1)–(7) will become clear when a full history and examination are carried out (Fig. 9.1). Factors (8) and (9) will only come into play if there is rampant caries that cannot be explained by the history.
Figure 9.1 An example of caries in a 12-year-old girl, who sucked Polo mints non-stop—‘six packets per day’.
9.3 Treatment decisions
The clinician must always give consideration to whether it is better to treat a carious lesion or to remineralize it.
9.3.1 Important points in relation to treatment
1. Gaining access to the caries inevitably means destruction of sound tooth tissue. The operator must keep this to a minimum consistent with complete caries eradication.
2. Once the operator places an initial restoration, he/she cannot ‘undo’ it and that tooth will inevitably require further restoration in its lifetime.
3. Every time an operator places a restoration, he/she destroys more of the original tooth structure, thereby weakening the tooth.
4. Even though the occlusion in a young person changes as growth occurs and teeth erupt, it is important to realize that when the operator places restorations, he/she must replicate the original occlusal contacts in the tooth. Although it may be tempting to keep the restoration totally out of the occlusion, teeth will move back into the occlusion, which will thereafter be slightly different and the cumulative effect of a lot of little changes can severely disrupt the occlusion in the long term.
5. When treating an approximal lesion on one tooth with an adjacent neighbour, the operator will almost certainly damage the latter. The important surface layer of the neighbouring tooth, which contains the highest level of fluoride, is the most resistant, so damage inflicted increases the chances of the adjacent surface of the neighbouring tooth becoming carious. It also creates an area of roughness on that surface, which in turn will accumulate more plaque, thereby increasing the risk of further decalcification.
6. When placing a class 2 restoration it is inevitable that there is some damage to the periodontal tissues. There is the transient damage caused by placement of the matrix band and wedge, and there is also an enduring effect, caused by the presence of the restoration margin. The very presence of the new restoration margin results in a contour change of the interstitial space. However smooth the operator attempts to make it, the altered state will increase plaque accumulation.
7. Repair and refurbishment of restorations instead of replacement saves tooth structure.
(See Key Points 9.1.)
9.3.2 Important points in relation to remineralization
1. Early smooth surface lesions are reversible in the right conditions.
2. There is little evidence to suggest that remineralization occurs in lesions already into dentine.
3. It is very difficult to predict the rate of progression of a caries lesion. The rate of caries progression is usually slow, but can be rapid in some individuals, particularly younger children. In general, the older the child is when a carious lesion is diagnosed, the slower the progress of the lesion, assuming constancy of other risk factors.
4. The remineralized tissue of early caries is less susceptible to further caries.
5. Small restorations are generally more successful than large restorations, so a balance has to be struck between allowing preventive procedures adequate time to function and the risk of lesion enlargement.
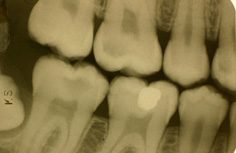
The progression rate of approximal caries can vary from tooth to tooth within the same mouth (Figs 9.2 and 9.3). It is thought that if the circumstances for remineralization are favourable, clinicians should use this modality as opposed to a restoration that has a finite but limited lifespan.
The operator can achieve remineralization with the aid of:
• fluoride rinse
• fluoride varnish
• chlorhexidine varnish
• CPP-ACP
Figure 9.2 A bitewing radiograph of a 13-year-old boy showing early caries in the upper right first permanent premolar and molar and in both lower molars.
Figure 9.3 Radiograph of the same boy 18 months later showing rapid progress of caries in the upper first premolar, molar, and lower second molar, with little or no change in the lower second premolar and molar.
• oral hygiene measures
• adjacent glass ionomer restorations.
Determination of the most effective method of retarding the progression of approximal caries requires identification of not only the most effective remineralizing agent but also the frequency with which to employ it.
Current studies indicate that fluoride varnishes, solutions, and toothpastes all have a significant effect on the progression of approximal caries in permanent molars when assessed radiographically. Chlorhexidine varnish does not appear to add any additional benefit to this. CPP-ACP shows some early promise as a remineralization tool, but further random controlled trials are needed. (See Key Point 9.2.)
Some questions still remain:
• Would the lesions have developed to the restorative stage if remineralizing techniques had not been employed?
• For how long should remineralization techniques be used?
• What is an acceptable frequency of monitoring the lesions radio-graphically if this is the only acceptable way of determining progress?
• Is the cost of remineralization therapy less than that of restorative treatment, particularly if it entails multiple attendances by the patient?
The progress of caries through the enamel seems to be fairly slow, but once the dentine is reached it accelerates. Therefore, as a rule of thumb, restore approximal surfaces once the lesion reaches the enamel–dentine interface.
9.4 Diagnosis
Whilst most dentists would agree that approximal caries is best diagnosed from bitewing radiographs, detection of occlusal caries is much more difficult. Where there is no overt or open cavity, diagnosing the status of a discoloured or stained fissure can be extremely difficult, if not impossible on occasions. Many methods have been proposed, both alone and in combination. These include:
• visual methods (dry tooth)
• probe/explorer (used only to remove debris)
• bitewing radiographs (see Box 9.1)
• electronic
• fibreoptic trans-illumination
• laser diagnosis.
When two or three methods are used in combination, there is greater accuracy and higher rates of detection of caries. The most widely used combination is visual inspection to examine a dry tooth (for stains, opacities, etc.) with a good light, along with a good-quality bitewing radiograph. Drying the tooth to be examined is essential, as early lesions, where the demineralization is minimal, will only become visible when there is a dry surface. (See Key Point 9.3.)
Additionally, flossing to clear any interstitial plaque and temporary separation of the teeth with either wedges or orthodontic separators may aid diagnosis by providing some direct vision to approximal areas (Figs 9.4 and 9.5). Different recommendations are made for the timing of bitewing radiographs in published guidelines, as discussed in Chapter 6. Conformity to these guidelines may not be good; a recent study found that only 72% of a group of Scottish dentists used radiography as a caries diagnostic tool in children. When planning which radiographs to take, the orthodontic implications that treatment of the caries may raise must also be taken into consideration. Young et al. (2009) reported that only 46.2% of children referred for removal of permanent teeth under general anaesthetic had undergone a previous radiographic assessment!
Figure 9.4 Decalcification on the mesial surface of the upper first molar. Radiographs show lesion confined to enamel.
Figure 9.5 Insertion of a separator may allow examination of the suspicious surface.
Bitewing radiographs (see Box 9.1) will show dentinal caries in teeth that are designated as clinically sound. The prevalence of ‘hidden caries’, i.e. radiographically visible dentine caries under a seemingly sound surface on visual inspection, in teenagers is reported to be between 10% and 15%. There will also be teeth visually designated as carious in which there are no radiological signs of caries, hence the need for more than one method of diagnosis.
In making a diagnosis of caries, the operator has to decide not only that there is a lesion present but also:
• whether demineralization is present
• the depth of the lesion
• the rate of progression of the lesion
• whether it is an arrested or active lesion.
It would be useful to have a method of quantifying these factors. Measurements of electrical conductance and laser fluorescence have the potential to chart lesion progression/retardation as they provide a quantitative record which, if repeated over several appointments, will demonstrate whether the lesion is active or arresting. They can be repeated safely more frequently than radiographs. However, it should be remembered that the electrical conductance and laser fluorescence methods will incorrectly interpret hypomineralization as caries and that the laser-based instrument will routinely interpret staining as caries. (See Key Points 9.4.)
9.5 Recurrent caries
Visual examination and radiographs are the most common ways of detecting recurrent caries.
Recurrent caries is most commonly found at the gingival margins of class II restorations, but often restorations will look a little ‘tatty’ at recall so careful examination in good light is essential.
Visually it is important to differentiate recurrent lesions from stained margins on resin-based composite restorations. Alternatives such as polishing or exploratory preparations adjacent to the lesion and repair may be appropriate rather than replacing the whole restoration. (See Key Point 9.5.)
9.6 Fissure sealants
A fissure sealant is a material that is placed in the pits and fissures of teeth in order to prevent the development of dental caries.
Fissure sealants cannot be discussed in isolation from caries diagnosis or treatment of pit and fissure caries. Fissure sealants can be used both preventively and therapeutically.
Toothbrush bristles cannot access the pit and fissure system because the dimensions of the fissures are too small. As a result micro-organisms remain within the fissure system undisturbed. The tooth is most susceptible to plaque stagnation during eruption, i.e. a period of 12–18 months. During this time, children need extra parental help in maintaining their oral hygiene. (See Key Point 9.6.)
Lesion formation takes place in the plaque stagnation area at the entrance to the fissure and commences with subsurface demineralization. Demineralized enamel is more porous than sound enamel. The more demineralized and porous the affected enamel, the more it shows up both clinically and on radiographs. (See Key Point 9.7.)
Once the initial lesion has developed, caries may spread laterally so that a small surface lesion may hide a much greater area of destruction below the surface (Figs 9.6 and 9.7).
Remineralization of occlusal lesions is much more difficult to achieve. Fissure sealing, application of 2.26% fluoride varnish every 6 months with oral hygiene instruction, and a weekly 0.2% sodium fluoride rinse have all been found to help stabilize the disease and retard the progress of occlusal caries, but fissure sealing the teeth is most effective. Many studies have shown that as caries rates decline, the proportion of pit and fissure caries of molar teeth has generally increased, and that the caries appears to be concentrated in a smaller cohort of children, with most of the decay occurring in 25% of the child population. This predilection has meant that correct application of fissure sealants should have a maximal effect.
There is no dispute that when correctly applied and monitored fissure sealants are highly effective at preventing dental caries in pit and fissures, but interpretation of the correct application and monitoring require scrutiny. (See Key Points 9.8.)
9.6.1 Who will benefit?
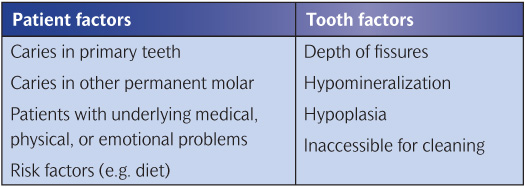
Not every fissure will become carious if it is not sealed. Therefore each tooth for each child must be assessed on its own merits. The clinician must assess the risk factors for that tooth developing pit or fissure caries (Table 9.1). As a general guide to who will benefit, review the British Society of Paediatric Dentistry (BSPD) guidelines (Smallridge 2010). (See Key Point 9.9.)
Figure 9.6 Hidden caries. Although the occlusal surface looks mostly intact it hides extensive caries.
Figure 9.7 Caries has been removed. The size of the cavity emphasizes the extent of the lesion.
Table 9.1 Factors to consider for sealant recommendation
The main beneficiaries are the following:
1. Children and young people with impairments such that their general health would be jeopardized by either the development of oral disease or the need for dental treatment. In such children all susceptible sites in both the primary and permanent dentitions should receive consideration.
2. The operator should seal all susceptible sites on permanent teeth in children and young people with caries in their primary teeth (decayed, filled, and missing tooth surfaces (DMFS) ≥2).
3. Where occlusal caries affects one permanent molar, the operator should seal the occlusal surfaces of the other molars.
4. If the anatomy of the tooth is such that surfaces are deeply fissured, the operator should seal that surface.
5. Where potential risk factors such as dietary factors or oral hygiene factors indicate a high risk of caries, seal all at-risk sites.
6. Where there is doubt about the caries status of a fissure or it is known to have caries confined to the enamel, fissure sealants may be used therapeutically but it is essential to monitor the surface both clinically and radiologically after application.
(See Key Point 9.10.)
Sealant use must be based on personal, tooth, and surface risk, and the clinician must assess these risks at intervals since they might change at any time in the life of the patient. Therefore, whereas it was traditionally stated that dentists should complete sealant application up to a year or two after eruption, he/she should assess the potential risk factors regularly, and place sealant when indicated (Figs 9.8 and 9.9).
Failure rates are higher when sealants are placed on newly erupted teeth and in mouths with high previous caries experience. Monitoring the integrity of the sealant is vital in these circumstances, and any deficiencies should be corrected. It is important that parents are made aware of this, and the fact that a sealant does not protect all surfaces of a tooth, so that their expectations are realistic and they bring their child for regular checks.
Figure 9.8 It is too early to seal this tooth with resin. Therefore it should be painted with fluoride varnish, or if the caries risk is very high it should be sealed with glass ionomer until further eruption has taken place.
Figure 9.9 This molar is just at the correct stage to apply fissure sealant. The very small operculum of gingival tissue can gently be held away from the tooth with a flat plastic spatula.
9.6.2 Clinical technique
Pre-treatment prior to sealant application
Tooth preparation with pumice and a rotary brush results in good clinical retention rates. Dry brushing achieves similar results. Air polishing using a Prophy-Jet, an early air abrasion system that uses sodium bicarbonate particles as the abrasive medium, provides good bond strength and sealant penetration, but has not received general acceptance probably because most dental surgeries do not possess this item of equipment.
Some researchers have advocated the use of ‘enameloplasty’, a more aggressive intervention into the tooth, i.e. mechanical enlargement of the fissures with a bur or with air abrasion, to improve sealant penetration and reduce micro-leakage. Although some studies have confirmed these claims, the authors feel that this submits the child to an unnecessary extra procedure and do not recommend it.
Etching
Etching for just 20 seconds with a range of concentrations of acid, but usually 35–37.5% phosphoric acid, is the tried and tested method. Its one drawback is the susceptibility of the etched surface to saliva/moisture contamination, which reduces the bond strength. Salivary contamination results in significantly reduced bond strengths unless the salia is removed by thorough washing. Re-etching of the surface is usually necessary.
Bonding agents
Use of a bonding agent under a resin fissure sealant aids bond strength. A bonding agent used as an additional layer under a resin sealant yields bond strengths significantly greater than the bond strength obtained when using sealant without a bonding agent. The initial results of clinical trials also show increased retention of the sealant when an intermediate bond is used. New bonding techniques are proving to be less technique sensitive with respect to moisture control than previous procedures.
The use of a bonding agent under sealant on wet contaminated surfaces yields bond strengths equivalent to the bond strength obtained when sealant is bonded directly to clean etched enamel without contamination. Most of the data on the use of a bonding agent as part of the sealant procedure support its use.
Use of a bonding agent tends to increase the time and cost of the sealant application, but in cases where maintaining a dry surface is difficult or where there are areas of hypomineralization on the surface it has many advantages.
Logically, combination of these technologies to achieve better penetration with fewer steps in the application sequence would be beneficial. The big bonus of the self-etching primer–adhesive system is the speed with which the operator can apply it. The operator brushes the self-etching adhesive onto the surface, where air thins it, and follows this by immediate placement of the sealant and polymerization. In the study, the average time operators took for the procedure was 1.8 minutes compared with 3.1 minutes with the conventional technique. Such time-saving is very useful in young fidgety children. However, there are conflicting results with these systems at present, and conventional separate etch and bond systems still appear to give superior retention of the sealant.
A Cochrane review (Ahovuo-Saloranto et al. 2004) recommends sealing with a resin-based sealant to prevent caries of the occlusal surface of permanent molars. Resin-based sealants have a good track record. Many clinical trials have demonstrated their effectiveness, and several long-term studies have show their benefits. A 28% complete retention and 35% partial retention of sealants on first permanent molars after a single application have been shown. Where researchers re-applied sealant to deficient surfaces, as determined by annual examinations, 65% complete retention was obtained and only 13% of the surfaces had caries or restorations after 20 years.
Re-treatment
Sealants placed in the first permanent molars of 6-, 7-, and 8-year-old children and in second permanent molars in 11- and 12-year-old children required more re-application than those placed in the teeth of older children. If the clinician places fissure sealant in newly erupted teeth, it is more likely to fail, but it should still be placed as early as possible because the teeth are so vulnerable to caries at this time. Parents must be aware of the possible loss and the importance of regular monitoring.
Modifying the resin to incorporate fluoride is a logical rationale. However, fluoride release occurs for only a very short time and at a very low level. Many studies over 2- to 3-year periods have reported good retention but similar caries incidence to conventional sealant. Since the addition of fluoride to sealant resin does not have any detrimental effect it could certainly be used, but until the chemistry can be adapted to unlock the fluoride readily, the anti-cariogenicity cannot be attributed to the fluoride.
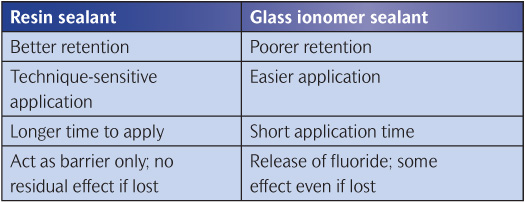
A greater release of fluoride can be achieved by using a glass ionomer (poly-alkenoate). Such cements have high levels of fluoride available for release but they suffer from the drawback of poor retention. Even with their very poor retention rates, sealing with glass ionomer does seem to impart some caries-protective effect. This may be due to both the fluoride released by the glass ionomer and residual material retained in the bottom of the fissure, which is invisible to the naked eye. Hence glass ionomers used as sealants can be classified as fissure sealants but more realistically as fluoride depot materials. Resin and glass ionomer sealants are compared in Table 9.2
Glass ionomer sealants can also be used in partially erupted teeth and where cooperation is too limited for a resin sealant. They can be usefully employed to seal partially erupted molars in high-risk children since eruption of the molars takes 12–18 months and during this time they are often very difficult to clean. Once the teeth are sufficiently erupted the operator can place a resin sealant. They are also useful in children in whom there are difficulties with the level of cooperation as the technique does not depend on absolute moisture control.
Table 9.2 Resin sealants versus glass ionomer sealants
Filled or unfilled resins?
Retention is better for unfilled resins probably because it penetrates into the fissures more completely. In addition, it does not need occlusal adjustment as it abrades very rapidly. If a filled resin is not adjusted there is a perceptible occlusal change, possible discomfort, and wear of the opposing antagonist tooth.
Coloured or clear material?
Opaque sealants have the advantage of high visibility at recall (Fig. 9.10). It has been found that the identification error for opaque resin was only 1% whilst for clear resin the corresponding figure was 23%, with the most common error being false identification of the presence of clear resin on an untreated tooth. The disadvantage of opaque sealant is that the dentist cannot visually examine the fissure at future recalls (Fig. 9.11). Both camps have a case, so it really comes down to personal choice.
Safety issues
There has only been one report of an allergy to the resin used for pit and fissure sealing.
Concern has been raised about the oestrogenicity of resin-based composites. The proposed culprit, bis-phenol A (BPA), is not a direct ingredient of dental sealants but is a chemical that appears in the final product if the raw materials fail to react fully. The amount released orally is undetectable in the systemic circulation and concerns about potential oestrogenicity are probably unfounded.
Figure 9.10 White fissure sealants can easily be seen to check at recall. They are also visible to show the patient and parent to help them understand the procedure.
Figure 9.11 Clear fissure sealant is less easy to see but its presence can be checked by etching if an area is giving cause for concern.
Sealant bulk in relation to application
With respect to the method of application, it is important to remember that the sealant must be kept to a minimum consistent with coverage of the complete fissure system including buccal and lingual pits. Over-filling can lead to reduction in retention and increased micro-leakage.
Sealant monitoring
Once the sealant has been placed the operator must monitor it at recall appointments and repair or replenish as necessary. Teeth lose 5–10% of sealant bulk each year. Partial loss of resin sealant allows ingress of bacteria into the fissure system, which leaves that surface equally at risk from caries as one that has not been sealed at all (Figs 9.12 and 9.13
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



 Key Points 9.1
Key Points 9.1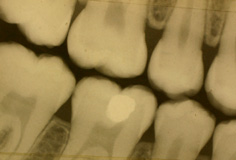
 Key Point 9.2
Key Point 9.2 Key Point 9.3
Key Point 9.3

 Key Points 9.4
Key Points 9.4 Key Point 9.5
Key Point 9.5 Key Point 9.6
Key Point 9.6 Key Point 9.7
Key Point 9.7 Key Points 9.8
Key Points 9.8

 Key Point 9.9
Key Point 9.9 Key Point 9.10
Key Point 9.10



