12
Traumatic injuries to the teeth
R. Welbury, J.M. Whitworth, and M.S. Duggal
Chapter contents
12.4.5 Radiographic examination
12.5 Injuries to the primary dentition
12.5.1 Uncomplicated crown fracture
12.5.2 Complicated crown fracture
12.5.5 Concussion, subluxation, and luxation injuries
12.6 Sequelae of injuries to the primary dentition
12.6.4 Injuries to developing permanent teeth
12.6.5 Treatment of injuries to the permanent dentition
12.7 Injuries to the permanent dentition
12.7.1 Injuries to the hard dental tissues and the pulp
12.7.3 Injuries to the periodontal tissues
12.7.5 Pulp canal obliteration
12.7.6 Injuries to the supporting bone
12.1 Epidemiology
Dental trauma in childhood and adolescence is common (Fig. 12.1). At 5 years of age 31-40% of boys and 16-30% of girls, and at 12 years of age 12-33% of boys and 4-19% of girls, will have suffered some dental trauma. Boys are affected almost twice as often as girls in both the primary and the permanent dentitions.
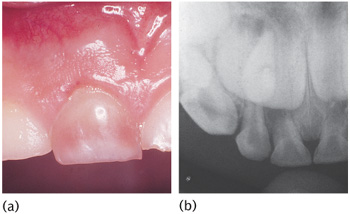
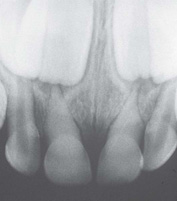
The majority of dental injuries in the primary and permanent dentitions involve the anterior teeth, especially the maxillary central incisors. Concussion, subluxation, and luxation are the most common injuries in the primary dentition (Fig. 12.2), while uncomplicated crown fractures are most common in the permanent dentition (Fig. 12.3).
Figure 12.1 A 7-year-old girl who fell off her bicycle and sustained orofacial injuries.
Figure 12.2 A 3-year-old child with a combination of injuries to her upper anterior teeth.
Figure 12.3 A fracture of the upper left central incisor involving enamel and dentine.
Figure 12.4 A 3-year-old boy with bruises and abrasions resulting from non-accidental injury.
Prognosis of traumatic injuries has improved significantly in the last 20 years. This has been largely due to a greater understanding and knowledge of pulpal procedures.
12.2 Aetiology
Children are most accident prone between 2 and 4 years for the primary dentition and between 7 and 10 years for the permanent dentition. Coordination and judgement are incompletely developed in children with primary dentition, and the majority of injuries are due to falls in and around the home as the child becomes more adventurous and explores his/her surroundings. In the permanent dentition most injuries are caused by falls and collisions while playing and running, although bicycles are a common accessory. The place of injury varies in different countries according to local customs, but accidents in the school playground remain common. Sports injuries usually occur in the teenage years and are commonly associated with contact sports. Injuries due to road traffic accidents and assaults are most commonly associated with the late teenage years and adulthood, and are often closely related to alcohol abuse.
One form of injury in childhood that must never be forgotten is child physical abuse or non-accidental injury (NAI). More than 50% of these children will have orofacial injuries (Fig. 12.4). See also Chapter 18.
Accidental injuries can be the result of either direct or indirect trauma. Direct trauma occurs when the tooth itself is struck. Indirect trauma is seen when the lower dental arch is forcefully closed against the upper, for example by a blow to the chin. Direct trauma implies injuries to the anterior region, while indirect trauma favours crown or crown-root fractures in the premolar and molar regions as well as the possibility of jaw fractures in the condylar regions and symphysis. The factors that influence the outcome or type of injury are a combination of energy impact, the resilience of the impacting object, the shape of the impacting object, and the angle of direction of the impacting force.
12.3 Classification
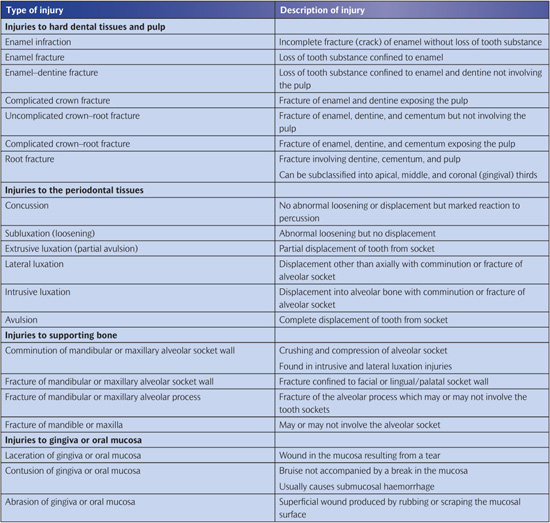
The classification of dento-alveolar injuries based on the World Health Organization (WHO) system is summarized in Table 12.1.
12.4 History and examination
A history of the injury followed by a thorough examination should be completed in any situation.
12.4.1 Dental history
1. When did injury occur? The time interval between injury and treatment significantly influences the prognosis of avulsions, luxations, crown fractures with or without pulpal exposures, and dento-alveolar fractures.
2. Where did injury occur? This may indicate the need for tetanus prophylaxis.
3. How did injury occur? The nature of the accident can yield information on the type of injury expected. Discrepancy between history and clinical findings raises suspicion of physical abuse.
4. Lost teeth/fragments? If a tooth or fractured piece cannot be accounted for when there has been a history of loss of consciousness, a chest radiograph should be obtained to exclude inhalation.
5. Concussion, headache, vomiting, or amnesia? Brain damage must be excluded and referral to a hospital for further investigation organized.
6. Previous dental history? Previous trauma can affect pulpal sensibility tests and the recuperative capacity of the pulp and/or periodon-tium. Alternatively, are there suspicions of physical abuse? Previous treatment experience, age, and parental/child attitude will affect the choice of treatment.
12.4.2 Medical history
1. Congenital heart disease, a history of rheumatic fever, or severe immunosuppression? These may be contraindications to any procedure that is likely to require prolonged endodontic treatment with a persistent necrotic/infected focus. Not all congenital heart defects carry the same risks of bacterial endocarditis, and the child’s paediatrician/cardiologist should be consulted before a decision regarding endodontic treatment is made.
2. Bleeding disorders? Very important if soft tissues are lacerated or teeth are to be extracted.
3. Allergies? Penicillin allergy requires alternative antibiotics.
4. Tetanus immunization status? Referral for tetanus toxoid injection is necessary if there is soil contamination of the wound and the child has not had a ‘booster’ injection within the last 5 years.
12.4.3 Extra-oral examination
When there are associated severe injuries a general examination is made with respect to signs of shock (pallor, cold skin, irregular pulse, hypotension), symptoms of head injury suggesting brain concussion, or maxillofacial fractures.
Facial swelling, bruises, or lacerations may indicate underlying bony and tooth injury. Lacerations will require careful debridement to remove all foreign material and suturing. Antibiotics and/or tetanus toxoid may be required if wounds are contaminated. Limitation of man-dibular movement or mandibular deviation on opening or closing the mouth indicate either jaw fracture or dislocation.
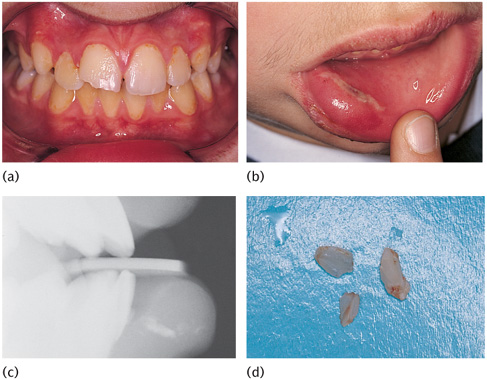
Crown fracture with associated swollen lip and evidence of a penetrating wound suggests retention of tooth fragments within the lip. Clinical and radiographic examinations should be undertaken (Fig. 12.5).
12.4.4 Intra–oral examination
This must be systematic and the following should be recorded:
1. Laceration, haemorrhage, and swelling of the oral mucosa and gingiva (Fig. 12.6). Any lacerations should be examined for tooth fragments or other foreign material. Lacerations of lips or tongue require suturing, but those of the oral mucosa heal very quickly and may not need suturing.
2. Abnormalities of occlusion, tooth displacement, fractured crowns, or cracks in the enamel.
The following signs and reactions to tests are particularly helpful:
1. Mobility. Degree of mobility is estimated in a horizontal and a vertical direction. When several teeth move together en bloc, a fracture of the alveolar process is suspected. Excessive mobility may also suggest root fracture or tooth displacement.
2. Reaction to percussion in a horizontal and vertical direction compared with a contralateral uninjured tooth. A duller note may indicate root fracture.
3. Colour of tooth. Early colour change associated with pulp breakdown is visible on the palatal surface of the gingival third of the crown.
4. Reaction to sensitivity tests. Thermal tests with warm gutta percha (GP) or ethyl chloride (EC) are widely used. However, an electric pulp tester (EPT) in the hands of an experienced operator is more reliable. Nevertheless, sensitivity testing is notoriously unreliable, especially in children, and should never be assessed in isolation from the other clinical and radiographic information. Neither negative nor positive responses immediately after trauma should be trusted. A positive response does not rule out later pulpal necrosis, and a negative response, while indicating pulpal damage, does not necessarily indicate a necrotic pulp. The negative reaction is often due to a ‘shock-wave’ effect which damages the apical nerve supply. In such cases the pulp may have a normal blood supply. In all sensitivity testing always include and document the reaction of uninjured contralateral teeth for comparison. In addition, all teeth neighbouring the obviously injured teeth should be regularly assessed as they have probably suffered concussion injuries.
Figure 12.5 (a) A 12-year-old child presented with an enamel and dentine fracture of the upper right permanent central incisor. (b) The lower lip was swollen with a mucosal laceration. (c) A lateral radiograph confirmed the presence of tooth fragments in the lip. (d) Fragments were retrieved from the lip under local anaesthesia.
Figure 12.6 Degloving injury to the lower labial sulcus that required exploration to remove grit.
12.4.5 Radiographic examination
Periapical
Reproducible ‘long-cone technique’ periapicals are the best for accurate diagnosis and clinical audit. Two radiographs at different angles may be essential to detect a root fracture. However, if access and cooperation are difficult, a single anterior occlusal radiograph rarely misses a root fracture. Periapical films positioned behind the lips can be used to detect foreign bodies.
Occlusal
This view detects root fractures when used inta-orally and foreign bodies within the soft tissues when held by the patient/helper at the side of the mouth in a lateral view (Fig. 12.5(c)).
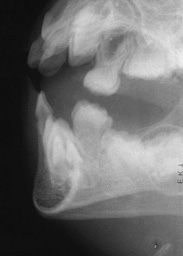
Orthopantomogram
This is essential in all trauma cases where underlying bony injury is suspected.
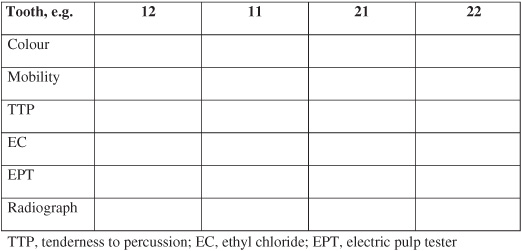
Trauma stamp
In the patient’s clinical notes the clinical and radiographic examinations at each visit can be combined into a simple aide-memoire in the form of a ‘trauma stamp’ (Fig. 12.7). Information that is collected in this standardized way is easily accessible when making clinical decisions and comparing responses at review appointments.
Figure 12.7 The trauma stamp.
12.4.6 Photographic records
Good clinical photographs are useful for assessing the outcome of treatment and for medico-legal purposes. Written consent must be obtained, and in the case of digital images uncropped originals must be held in an appropriately secure format and location. (See Key Point 12.1.)
12.5 Injuries to the primary dentition
During its early development the permanent incisor is located palatally to and in close proximity with the apex of the primary incisor. With any injury to a primary tooth, there is risk of damage to the underlying permanent successor.
Most accidents in the primary dentition occur between 2 and 4 years of age. Realistically, this means that few restorative procedures will be possible and in the majority of cases the decision is between extraction or maintenance without performing extensive treatment. A primary incisor should always be removed if its maintenance will jeopardize the developing tooth bud.
A traumatized primary tooth that is retained should be assessed regularly for clinical and radiographic signs of pulpal or periodontal complications. Radiographs may even detect damage to the permanent successor. Soft tissue injuries in children should be assessed weekly until healed. Tooth injuries should be reviewed every 3–4 months for the first year and then annually until the primary tooth exfoliates and the permanent successor is in place.
Traumatic injuries that occur prior to eruption of primary teeth can also interfere with their development.
12.5.1 Uncomplicated crown fracture
Either smooth sharp edges or restore with an acid etch restoration if cooperation is satisfactory.
12.5.2 Complicated crown fracture
Extraction is normally the treatment of choice. However, pulp extirpation and canal obturation with zinc oxide cement, followed by an acid etch restoration, is possible with reasonable cooperation.
12.5.3 Crown–root fracture
The pulp is usually exposed and any restorative treatment is very difficult. It is best to extract the tooth.
12.5.4 Root fracture
If there is no displacement and only a small amount of mobility, the tooth should be kept under observation. If the coronal fragment becomes non-vital and symptomatic, it should be removed. The apical portion usually remains vital and undergoes normal resorption. Similarly, with marked displacement and mobility only the coronal portion should be removed.
12.5.5 Concussion, subluxation, and luxation injuries
Associated soft tissue damage should be cleaned by the parent twice daily with 0.2% chlorhexidine solution using cotton buds or gauze swabs until it heals.
Concussion
This is often not brought to a dentist’s attention until the tooth discolours.
Subluxation
If there is slight mobility, the parents are advised to keep the child on a soft diet for 1–2 weeks and to keep the traumatized area as clean as possible. Marked mobility requires extraction.
Extrusive luxation
Marked mobility requires extraction.
Lateral luxation
If the crown is displaced palatally the apex moves buccally and hence away from the permanent tooth-germ. If the occlusion is not gagged, conservative treatment to await some spontaneous realignment is possible. If the crown is displaced buccally, the apex will be displaced towards the permanent tooth bud and extraction is indicated in order to minimize further damage to the permanent successor.
Figure 12.8 (a) A 4-year-old boy with complete intrusion of the upper right incisor. (b) Six months post-trauma, the tooth has spontaneously re-erupted.
Intrusive luxation
This is the most common type of injury. The aim of investigation is to establish the direction of displacement by thorough radiological examination. If the root is displaced palatally towards the permanent successor, the primary tooth should be extracted to minimize the possible damage to the developing permanent successor. If the root is displaced buccally, there should be periodic review to monitor spontaneous re-eruption (Fig. 12.8). Review should be weekly for a month and then monthly for a maximum of 6 months. Most re-eruption occurs between 1 and 6 months. If this does not occur, ankylosis is likely and extraction is necessary to prevent ectopic eruption of the permanent successor (Fig. 12.9).
Figure 12.9 Severe intrusion of an upper primary central incisor necessitating extraction.
Exarticulation (avulsion)
Replantation of avulsed primary incisors is not recommended because of the risk of damage to the permanent tooth-germs. Space maintenance is not necessary following the loss of a primary incisor as only minor drifting of adjacent teeth occurs. The eruption of the permanent successor may be delayed for about a year as a result of abnormal thickening of connective tissue overlying the tooth-germ.
12.6 Sequelae of injuries to the primary dentition
12.6.1 Pulpal necrosis
Necrosis is the most common complication of primary trauma. Evaluation is based on colour and radiography. Teeth of a normal colour rarely develop periapical inflammation but, conversely, mildly discoloured teeth may be vital. A mild grey colour occurring soon after trauma may represent intrapulpal bleeding with a pulp that is still vital. This colour may recede, but if it persists necrosis should be suspected. Radiographic examination should be every 3 months to check for periapical inflammation (Fig. 12.10). Failure of the pulp cavity to reduce in size is an indicator of pulpal death. Teeth should be extracted whenever there is evidence of periapical inflammation to prevent possible damage to the permanent successor.
12.6.2 Pulpal obliteration
Obliteration of the pulp chamber and canal is a common reaction to trauma (Fig. 12.11). Clinically, the tooth becomes yellow/opaque. Normal exfoliation is usual, but occasionally periapical inflammation may intervene and therefore annual radiography is advisable.
12.6.3 Root resorption
Extraction is advised for all types of root resorption where there is evidence of infection (Fig. 12.12).
Figure 12.10 (a) Severe discolouration of the upper right primary central incisor. (b) Radiographic evidence of periapical pathology. Extraction was necessary.
Figure 12.11 Pulp canal obliteration and external surface resorption of upper primary central incisors after a luxation injury.
Figure 12.12 External inflammatory resorption of previously injured primary incisors.
12.6.4 Injuries to developing permanent teeth
Injuries to the permanent successor tooth can be expected in 12-69% of primary tooth trauma and 19-68% of jaw fractures. Intrusive luxation causes most disturbances, but avulsion of a primary incisor will also cause damage if the apex moved towards the permanent tooth bud before the avulsion. Most damage to the permanent tooth bud occurs under 3 years of age during its developmental stage. However, the type and severity of disturbance are closely related to the age at the time of injury. Changes in the mineralization and morphology of the crown of the permanent incisor are most common, but later injuries can cause radicular anomalies. Injuries to developing teeth can be classified as follows:
1. White or yellow-brown hypomineralization of enamel. Injury at 2–7 years (Fig. 12.13).
2. White or yellow-brown hypomineralization of enamel with circular enamel hypoplasia. Injury at 2–7 years (Fig. 12.14).
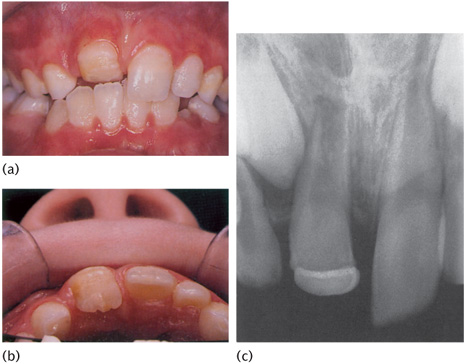
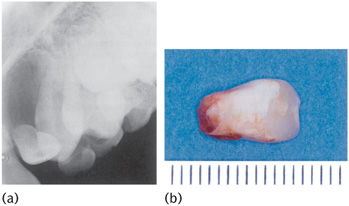
3. Crown dilaceration. Injury at about 2 years (Fig. 12.15).
4. Odontoma-like malformation. Injury at 1–3 years.
5. Root duplication. Injury at 2–5 years.
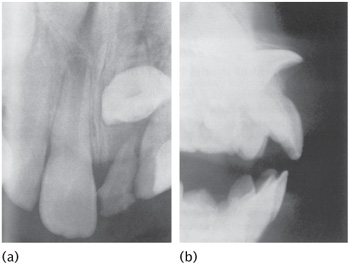
6. Vestibular or lateral root angulation and dilaceration. Injury at 2–5 years (Fig. 12.16).
7. Partial or complete arrest of root formation. Injury at 5–7 years (Fig. 12.17).
8. Sequestration of permanent tooth-germs.
9. Disturbance in eruption.
The term dilaceration describes an abrupt deviation of the long axis of the crown or root portion of the tooth. This deviation results from the traumatic displacement of hard tissue, which has already been formed, relative to developing soft tissue.
The term angulation describes a curvature of the root resulting from a gradual change in the direction of root development, without evidence of abrupt displacement of the tooth-germ during odon-togenesis. This may be vestibular (i.e. labiopalatal) or lateral (i.e. mesiodistal).
Evaluation of the full extent of complications following injuries must await complete eruption of all permanent teeth involved. However, most serious sequelae (disturbances in tooth morphology) can usually be diagnosed radiographically within the first year post-trauma.
Eruption disturbances may involve delay because of thickening of connective tissue over a permanent tooth-germ, ectopic eruption due to lack of eruptive guidance, and impaction in teeth with malformations of crown or root. (See Key Points 12.2.)
Figure 12.13 (a) Investigation of delayed eruption of the permanent upper central incisors revealed (b) an intruded upper left primary central incisor on radiograph. (c) Following removal of the retained primary incisor, the permanent successor erupted spontaneously with a white hypoplastic spot on the labial surface.
Figure 12.14 Brown hypoplastic area on the lower left permanent central incisor resulting from trauma to the primary predecessor.
12.6.5 Treatment of injuries to the permanent dentition
Yellow-brown hypomineralization of enamel with or without hypoplasia
1. Acid–pumice micro–abrasion.
2. Composite resin restoration: localized, veneer, or crown.
3. Porcelain restoration: veneer or crown (anterior); fused to metal crown (posterior). Conservative approaches are preferred whenever possible.
Crown dilaceration
1. Surgical exposure + orthodontic realignment.
2. Removal of dilacerated part of crown.
3. Temporary crown until root formation complete.
4. Semi-permanent or permanent restoration.
Vestibular root angulation
Combined surgical and orthodontic realignment.
Other malformation
Extraction is usually the treatment of choice.
Disturbance in eruption
Surgical exposure + orthodontic realignment.
Injuries to supporting bone
Most fractures of the alveolar socket in primary dentition do not require splinting because bony healing is rapid in small children. Jaw fractures are treated in the conventional manner, although stabilization after reduction may be difficult because of lack of sufficient adjacent teeth.
12.7 Injuries to the permanent dentition
Most traumatized teeth can be treated successfully. Prompt and appropriate treatment improves prognosis. The aims and principles of treatment can be broadly categorized as follows:
1. Emergency:
(a) retain vitality of fractured or displaced tooth;
(b) treat exposed pulp tissue;
(c) reduction and immobilization of displaced teeth;
(d) antiseptic mouthwash ± antibiotics and tetanus prophylaxis.
2. Intermediate:
(a) + pulp therapy;
(b) minimally invasive crown restoration.
3. Permanent:
(a) apexogenesis/apexification;
(b) root filling + root extrusion;
(c) + gingival and alveolar collar modification;
(d) semi-permanent or permanent coronal restoration.
Figure 12.15 (a) Labial, (b) palatal, and (c) radiographic appearance of a severe crown dilaceration of the upper right permanent central incisor which erupted spontaneously.
Figure 12.16 Unerupted dilacerated upper left permanent central incisor resulting from an accident sustained by a 3-year-old child.
Figure 12.17 Failure of root formation of the upper left permanent lateral incisor (against a centimetre scale) in a 5-year-old child with a history of intrusive trauma to the primary predecessor.
Trauma cases require painstaking follow-up to identify any complications and institute the correct treatment. The trauma stamp is invaluable in this. In the review period the following schedule is a guide: 1 week; 1, 3, 6, and 12 months; then annually for 4–5 years.
12.7.1 Injuries to the hard dental tissues and the pulp
Enamel infraction
These incomplete fractures without loss of tooth substance and without proper illumination are easily overlooked. Review is necessary, as above, as the energy of the blow may have been transmitted to the periodontal tissues or the pulp.
Enamel fracture
No restoration is needed and treatment is limited to smoothing of any rough edges and splinting if there is associated mobility. Periodic review as above.
Enamel–dentine (uncomplicated) fracture
Immediate treatment is necessary and the pulp requires protection against thermal osmotic irritation and from bacteria via the dentinal tubules. Restoration of crown morphology also stabilizes the position of the tooth in the arch.
Emergency protection of the exposed dentine can be achieved by the following:
1. A composite resin (acid etched) or compomer bandage.
2. Glass ionomer cement within an orthodontic band or incisal end of a stainless steel crown if there is insufficient enamel available for acid-etch technique.
Intermediate restoration of most enamel-dentine fractures can be achieved by the following:
1. Acid-etched composite applied either freehand or utilizing a celluloid crown-former. The majority of these restorations can be regarded as semi-permanent/permanent. Larger fractures can utilize more available enamel surface area for bonding by employing a complete celluloid crown-former to construct a ‘direct’ composite crown. As the child becomes older, this could be reduced to form the core of a full- or partial-coverage porcelain crown preparation.
2. Reattachment of crown fragment. Few long-term studies have been reported and the longevity of this type of restoration is uncertain. In addition, there is a tendency for the distal fragment to become opaque or require further restorative intervention in the form of a veneer or full-coverage crown (Fig. 12.18). If the fracture line through dentine is not very close to the pulp, the fragment can be reattached immediately. However, if it runs close to the pulp, it is advisable to place a suitably protected calcium hydroxide dressing over the exposed dentine for at least a month while storing the fragment in saline, which should be renewed weekly.
Technique
1. Check the fit of the fragment and the vitality ofthe tooth.
2. Clean fragment and tooth with pumice-water slurry.
3. Isolate the tooth with rubber dam.
4. Attach fragment to a piece of sticky wax to facilitate handling.
5. Etch enamel for 30 seconds on both fracture surfaces and extend for 2mm from fracture line on tooth and fragment. Wash for 15 seconds and dry for 15 seconds.
6. Apply bonding agent ± dentine primer according to the manufacturer’s instructions and light cure for 10 seconds.
7. Place appropriate shade of composite resin over both surfaces and position fragment. Remove gross excess and cure for 60 seconds labially and palatally.
8. Remove any excess composite resin with sandpaper discs.
9. Remove a 1mm gutter of enamel on each side of the fracture line both labially and palatally to a depth of 0.5mm using a small round or pear-shaped bur. The finishing line should be irregular in outline.
10. Etch the newly prepared enamel, wash, dry, apply composite, cure, and finish.
Enamel-dentine–pulp (complicated) crown fracture
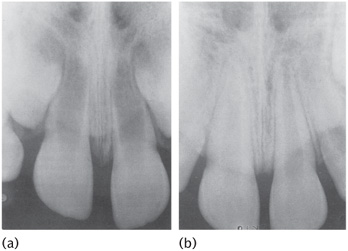
The most important function of the pulp is to lay down dentine which forms the basic structure of teeth, defines their general morphology, and provides them with mechanical strength and toughness. Dentine deposition commences many years before permanent tooth eruption, and when a tooth erupts the pulp within still has work to do in completing root development. Newly erupted teeth have short roots, their apices are wide and often diverging, and the dentine walls of the entire tooth are thin and relatively weak (Fig. 12.19(a)). Provided that the pulp remains healthy, dentine deposition and normal root development will continue for 2–3 years after eruption in permanent teeth (Fig. 12.19(b)). Loss of pulp vitality before a tooth has reached maturity may leave the tooth vulnerable to fracture, and with an unfavourable crown-root ratio. In addition, endodontic treatment of non-vital immature teeth can present technical difficulties which may compromise the long-term prognosis of the tooth.
The major concern after pulpal exposures in immature teeth is the prevention of physical, chemical, and microbial invasion and the preservation of pulpal vitality in order to allow continued root growth. The radicular pulp has enormous capacity to remain healthy and undergo repair if all infected and inflamed coronal tissue is removed and an appropriate wound dressing and sealing coronal restoration is applied. Pulp amputation by partial pulpotomy or complete coronal pulpotomy is often the treatment of choice, but pulp capping can be considered in certain circumstances.
Figure 12.18 An upper left permanent central incisor 3 years after reattachment of a fractured incisal fragment.
Figure 12.19 Maturation of permanent incisors. (a) Immature incisors showing short roots with incomplete wide open apices. The lateral walls of the roots are thin and structurally weak. (b) The same teeth 2 years later: the roots are now almost complete following continued dentine deposition by healthy pulp.
• Vital pulp therapy:
• Non-vital pulp therapy:
– pulpectomy
Vital pulp therapy: pulp capping
The procedure must be done within 24 hours of the incident. The tooth should be isolated with rubber dam and no instruments should be inserted into the exposure site. Any bleeding should be controlled with sterile cotton wool which may be moistened with saline or sodium hypochlorite, and not with a blast of air from a three-in-one syringe which may drive debris and micro-organisms into the pulp. A layer of setting calcium hydroxide cement is gently flowed onto the exposed pulp and surrounding dentine and quickly overlaid with a ‘bandage’ of adhesive material (e.g. compomer) pending definitive aesthetic restoration at a later date. A successful direct pulp cap will preserve the remaining pulp in health and should promote the deposition of a bridge of reparative dentine to seal off the exposure site.
Review after a month, then 3 months, and eventually at 6-monthly intervals for up to 4 years in order to assess pulp vitality. Periodic radiographic review should also be arranged to monitor dentine bridge formation and root growth, and to exclude the development of necrosis and resorption. On the radiograph check the following:
• root is growing in length
• root canal is maturing (narrowing).
Compare with antimere. If growth is not occurring, the pulp should be assumed to be non-vital.
Vital pulp therapy: pulpotomy
In pulpotomy a portion of exposed vital pulp is removed to preserve the radicular vitality and allow completion of apical root development (apexogenesis) and further deposition of dentine on the walls of the root. This procedure is the treatment of choice following trauma where the pulp has been exposed to the mouth for more than 24 hours. The amount of pulp that is removed depends on the time since exposure, which will also determine the depth of contamination of the pulp. Attempts must be made to remove only the pulp that is deemed to be contaminated. If the patient presents within 24–48 hours of the incident, it is safe to assume that the contaminated zone is no more than 2-4mm around the exposure site and only the pulp in the immediate vicinity of the exposure is removed, in a procedure also termed partial pulpotomy (Cvek’s technique). For more extensive exposures all coronal pulp can be removed down to the cervical constriction of the tooth (See Key Points 12.3). The operative procedure (Fig. 12.20) is as follows:
• Under local anaesthesia and rubber dam, pulp tissue is excised with a diamond bur running at high speed under constant water cooling. This causes least injury to the underlying pulp and is preferred to hand excavation or the use of slow-speed steel burs.
• Microbial invasion of an exposed vital pulp is usually superficial and generally only 2-4mm of pulp tissue should be removed (partial pul-potomy (Cvek)).
• Excessive bleeding from the residual pulp which cannot be controlled with moist cotton wool, or indeed no bleeding at all, indicates that further excision is required to reach healthy tissue (coronal pulpotomy).
• Removal of tissue may occasionally extend more deeply into the tooth (full coronal pulpotomy) in an e/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses







 Key Point 12.1
Key Point 12.1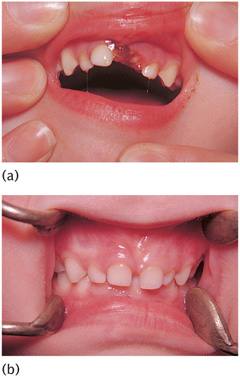

 Key Points 12.2
Key Points 12.2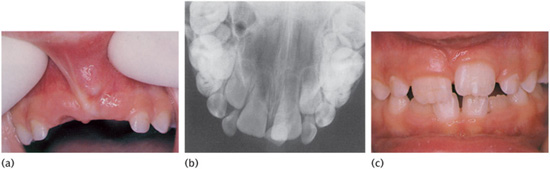


 Key Points 12.3
Key Points 12.3