History of and Examination for Temporomandibular Disorders
“NOTHING IS MORE CRITICAL TO SUCCESS THAN BEGINNING WITH ALL THE NECESSARY DATA.”
—JPO
THE SIGNS AND SYMPTOMS of temporomandibular disorders (TMDs) are extremely common. The epidemiologic studies described in Chapter 7 suggest that 50% to 60% of the general population have at least one sign of some functional disturbance of the masticatory system. Some of these appear as significant symptoms that motivate patients to seek treatment. Many, however, are subtle and not even at a level of the patient’s clinical awareness. As described earlier, signs of which the patient is unaware are said to be subclinical. Some subclinical signs can later become apparent and, if left unattended, may come to represent more significant functional disturbances. It is important, therefore, to identify any and all signs and symptoms of functional disturbances in every patient.
This is not to suggest that all signs indicate a need for treatment. The significance of the sign and the etiology as well as the prognosis of the disorder are factors that determine the need for treatment. The significance of a sign, however, cannot be evaluated until that sign has been identified. Since many of the signs are subclinical, many disturbances can progress and remain undiagnosed and therefore untreated by the clinician. The effectiveness and success of treatment lie in the ability of the clinician to establish the proper diagnosis. This can be established only after a thorough examination of the patient for the signs and symptoms of functional disturbances. Each sign represents a portion of information needed to establish a proper diagnosis. It is therefore extremely important that each sign and symptom be identified by means of a thorough history and examination procedure. This is the essential foundation of successful treatment.
The purpose of a history and examination is to identify any area or structure of the masticatory system that shows breakdown or pathologic change. If this is to be effective, the examiner must have a sound understanding of the clinical appearance and function of the healthy masticatory system (Part I of this text). Breakdown in the masticatory system is generally signified by pain and/or dysfunction. History and examination procedures should therefore be directed toward the identification of masticatory pain and dysfunction.
When the patient’s chief complaint is pain, it is important to identify the source of the problem. The dentist’s primary role in therapy is the treatment of masticatory pains. As already described, masticatory pains have their sources in and emanate from masticatory structures. Masticatory structures are the teeth, the periodontium, the supporting structures of the teeth, the temporomandibular joints (TMJs), and the muscles that move the mandible. By virtue of training, the dentist is best suited to treat these structures. Unfortunately, however, disorders of the head and neck can frequently lead to heterotopic pains that are felt in the masticatory structures but do not have their sources within masticatory structures (Chapter 2). These types of pains must be properly identified during an examination so that an accurate diagnosis can be established. To be effective, treatment must be directed toward the source of pain and not toward the site. For dental treatment to be effective, the pain must be of masticatory origin.
A general rule in the effort to identify masticatory pain is that jaw function usually aggravates or accentuates the problem. In other words, the functional activities of chewing and talking increase the pain. This rule does not always apply since some nonmasticatory pains can produce secondary hyperalgesia in masticatory structures, thus function will increase the pain. At the same time, one must be suspicious of the patient who reports the location of the pain to involve the TMJ or masticatory muscles yet whose history and examination reveal no alteration in range of jaw movement or increase in pain during function. When this circumstance exists, therapy directed toward the masticatory structures is likely to be useless. The examiner must find the true source of the pain before effective treatment can be provided.
Screening History and Examination
Since the prevalence of TMDs is very high, it is recommended that every patient who comes to the dental office be screened for these problems regardless of the apparent need or lack of need for treatment. The purpose of the screening history and examination is to identify patients with subclinical signs as well as symptoms that the patient may not relate but are commonly associated with functional disturbances of the masticatory system (e.g., headaches, ear symptoms). A screening history should consist of several short questions that will help alert the clinician to any TMDs. These can be asked personally by the clinician or may be included in a general health and dental questionnaire that the patient completes prior to first being seen by the dentist.
The following questions can be asked of the patient to identify functional disturbances1:
1. Do you have difficulty and/or pain opening your mouth, for instance, when yawning?
2. Does your jaw get “stuck,’’ “locked,’’ or “go out’’?
3. Do you have difficulty and/or pain when you are chewing, talking, or using your jaws?
4. Are you aware of noises in the jaw joints?
5. Do your jaws regularly feel stiff, tight, or tired?
6. Do you have pain in or about the ears, temples, or cheeks?
7. Do you have frequent headaches, neck aches, or toothaches?
8. Have you had a recent injury to your head, neck, or jaw?
9. Have you been aware of any recent changes in your bite?
10. Have you previously been treated for any unexplained facial pain or a jaw joint problem?
Accompanying the screening history is a short screening examination. This should be brief and is an attempt to identify any variation from normal anatomy and function. It begins with an inspection of the facial symmetry. Any variation from the general bilateral symmetry should raise suspicion and indicate the need for further examination. The screening examination also includes observations of jaw movement. Restriction or irregular mandibular movements are indications for a more thorough examination.
Several important structures of the masticatory system are palpated for pain or tenderness during the screening examination. The temporal and masseter muscles are palpated bilaterally along with the lateral aspects of the TMJs. Any pain or tenderness should be viewed as a potential indicator of a TM disorder.
If the screening history and examination reveal positive findings, a more thorough history and examination for TMDs is completed. Three basic structures should be examined for pain and/or dysfunction: the muscles, the TMJs, and the dentition. Prior to the examination, a complete history of the problem, both past and present, is obtained from the patient.
History Taking for Temporomandibular Disorders
The importance of taking a thorough history cannot be overemphasized. When the clinician is examining a patient for dental disease (e.g., caries), a relatively small percentage of the information needed for diagnosis will be gained through the history; most of it will come from the examination. Diagnosing pain, however, is quite different. With pain disorders, as much as 70% to 80% of the information needed to make the diagnosis will come from the history, with the examination contributing a smaller part.
Most often the patient will provide essential information that cannot be acquired from the examination procedures. The history is key in making an accurate diagnosis. In fact, the patient will often tell the examiner the precise diagnosis, only it will be in his or her own words.
The history can be obtained in one of two ways. Some clinicians prefer to converse directly with the patient concerning the past history of the problem. This allows them to direct questions that appropriately follow the patient’s previous response. Although this method of seeking vital facts is very effective, it relies heavily on the clinician’s ability to pursue all areas of concern. A more thorough and consistent history can be taken by using a written questionnaire that includes all areas of concern. This method ensures that every bit of necessary information is obtained. Although a questionnaire is usually more complete, some patients have difficulty expressing their problems using a standard form. Therefore in most cases the best history taking consists of having the patient complete a predeveloped questionnaire and then reviewing this with the patient, giving both clinician and patient an opportunity to discuss and elaborate on important areas.
It is helpful to have the patient complete the questionnaire in a quiet area and with no particular time constraints. As the clinician reviews the questionnaire with the patient, any discrepancies or major concerns can be discussed in order to gain additional information. At this time the patient is freely allowed to expound on concerns that were not expressed in the questionnaire.
The history should include a complete medical questionnaire identifying all the patient’s major medical problems. Such problems can play an important role in functional disturbances. For example, a patient’s generalized arthritic condition can also affect the TMJ. Even when symptoms are not closely related to a major medical problem, the existence of such a problem may play an important role in selecting a treatment method.
An effective history centers on the patient’s chief complaint. This is a good starting point in obtaining needed information. The patient is allowed to describe, in his or her own words, the chief complaint. If the patient has more than one complaint, each of the complaints is initially recorded and detailed information on each is collected separately. A complete history obtains information in the following specific areas.
Pain
When pain is present, it is evaluated according the patient’s description of the chief complaint: its location, onset, and characteristics; any aggravating and alleviating factors; past treatments; and any relationship to other complaints as to location, behavior, quality, duration, and degree. Each of these factors is discussed in this section and highlighted in Box 9-1.
The chief complaint
A good starting point in history taking is to obtain an accurate description of the patient’s chief complaint. This should first be taken in the patient’s own words and then restated in technical language as indicated. If the patient has more than one pain complaint, each complaint should be noted and, when possible, placed in a list according to its significance to the patient. Each complaint must be evaluated according to each factor listed in the history outline. Once this has been accomplished, each pain complaint should be assessed as to its relationship to any of the other complaints. Some complaints may be secondary to others while others may be independent. Determining these relationships is basic to management.
Location of the pain
The patient’s ability to locate the pain with accuracy has diagnostic value. The examiner, however, should always guard against assuming that the site of pain necessarily identifies the true source of pain, the structure from which the pain actually emanates. The patient’s description of the location of his or her complaint identifies only the site of pain. It is the examiner’s responsibility to determine whether it is also the true source of the pain. Sometimes what appears to be adequate cause at the site of pain may mislead both patient and doctor, such as visible superficial herpetic lesions in an area that also happens to be the site of pain referral from the cervical area. The clinician must perform the needed diagnostic tests to determine the true source of the pain (Chapter 10).
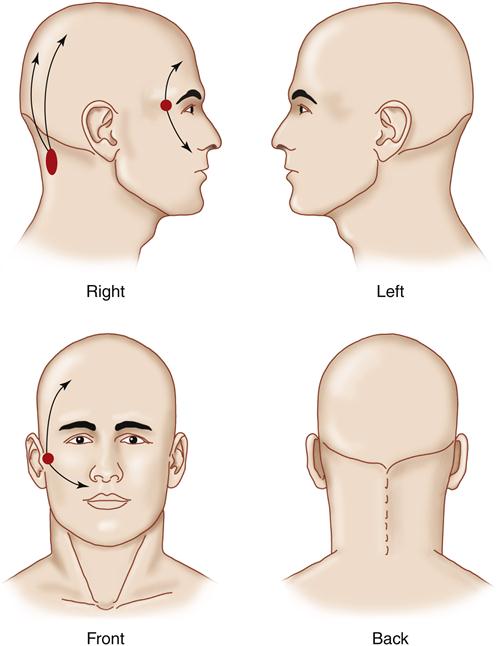
It can be very helpful to provide patients with a drawing of the head and neck and ask them to outline the location of their pain (Figure 9-1). This allows them to reflect in their own way on any and all of the pain sites. They can also draw arrows revealing any patterns of pain referral. These drawing can give the clinician significant insight regarding the location and even the type of pain the patient is experiencing.
In the office where chronic pain is being evaluated it is helpful to have a drawing of the entire body so that the clinician can appreciate other locations of pain. A full-body drawing can be quite revealing for patients with fibromyalgia or generalized arthritic conditions. It is very important to take into account the patient’s entire pain condition.
Onset of the pain
It is important to assess any circumstances associated with the initial onset of the pain complaint. These circumstances can give great insight as to etiology. For example, in some instances the pain complaint will have begun immediately following a motor vehicle accident. Trauma is a frequent cause of a pain condition and not only gives insight as to etiology but also enlightens the examiner to other considerations such as other injuries, related emotional trauma, and possible litigation. The onset of some pain conditions is associated with systemic illnesses or jaw function, or it may even be wholly spontaneous. It is important that the patient present the circumstances associated with the initial onset in chronologic order so that proper relationships can be evaluated.
It is equally important to ask the patient what he or she feels caused the pain condition. This may provide great insight into the patient’s view of the pain. In many instances the patient knows precisely what caused the condition. Even if the patient is confused as to cause, the examiner may gain valuable information that is useful in management. For example, this question may reveal anger associated with blame for the pain condition. It is important to know if the patient believes mistreatment or another practitioner has caused the pain. This type of anger may greatly affect future treatment outcome.
Characteristics of the pain
The characteristics of the pain must be precisely described by the patient as to their quality, behavior, intensity, concomitant symptoms, and manner of flow.
Quality of the pain
The quality of pain should be classified according to how it makes the patient feel. The terms bright and dull are commonly used. When pain has a stimulating or exciting effect on the patient, it is classified as bright. When the pain has a depressing effect that causes the patient to withdraw to some extent, it is classified as dull. It is important that such judgment be wholly independent of pain intensity, variability, temporal characteristics, or any accompanying lancinating exacerbations that may punctuate the basic underlying painful sensation.
Further evaluation of the quality of pain should be made to classify it as pricking, itching, stinging, burning, aching, or pulsating. Many pains, of course, require more than a single designation. Bright, tingling pain is classified as a pricking sensation, especially when it is mild and stimulating. Superficial discomfort that does not reach pain threshold intensity may be described as itching. As intensity increases, it may take on a pricking, stinging, aching, or burning quality. Deep discomfort that does not reach pain threshold intensity may be described as a vague, diffuse sensation of pressure, warmth, or tenderness. As intensity increases, the pain may take on a sore, aching, throbbing, or burning quality. When the discomfort has an irritating, hot, raw, caustic quality, it is usually described as burning. Most pains have an aching quality. Some noticeably increase with each heartbeat and are described as pulsating or throbbing.
Behavior of the pain
The behavior of the pain should be evaluated according to its frequency or temporal behavior as well as its duration and localizability.
Temporal behavior
Temporal behavior reflects the frequency of the pain as well as the periods between episodes of pain. If the suffering distinctly comes and goes, leaving pain-free intervals of noticeable duration, it is classified as intermittent. If such pain-free intervals do not occur, it is classified as continuous. Intermittency should not be confused with variability, in which there may be alternating periods of high- and low-level discomfort. Intermittent pain implies the occurrence of true intermissions or pain-free periods during which comfort is complete. This temporal behavior should not be confused with the effect of medications that induce periods of comfort by analgesic action. When episodes of pain, whether continuous or intermittent, are separated by an extended period of freedom from discomfort only to be followed by another similar episode of pain, the syndrome is said to be recurrent.
Duration of the pain
The duration of individual pains in an episode is an important descriptive feature that aids in pain identification. A pain is said to be momentary if its duration can be expressed in seconds. Longer-lasting pains are classified in minutes, hours, or days. A pain that continues from one day to the next is said to be protracted.
Localization of the pain
The localization behavior of the pain should be included in its description. If the patient is able to define the pain to an exact anatomic location, it is classified as localized pain. If such description is less well defined and somewhat vague and variable anatomically, it is termed diffuse pain. Rapidly changing pain is classified as radiating. A momentary cutting exacerbation is usually described as lancinating. More gradually changing pain is described as spreading; if it progressively involves adjacent anatomic areas, the pain is called enlarging. If it changes from one location to another, the complaint is described as migrating. Referred pain and secondary hyperalgesia are clinical expressions of secondary or heterotopic pain.
Intensity of the pain
The intensity of pain should be established by distinguishing between mild and severe pain. This can be based on how the patient appears to react to the pain. Pain that the patient describes as mild is generally not associated with any display of visible physical reactions. Severe pain is associated with significant reactions of the patient to provocation of the painful area. One of the best methods of assessing the intensity of the pain is with a visual analog scale. The patient is presented with a line that has “no pain” written at one end and “the most severe pain possible” at the other. The patient is then asked to place a mark on the location of the line that best describes the pain today. A scale of 0 to 5 or 0 to 10 can be used to assess the intensity of the pain, with 0 being no pain and 10 being the most pain possible. This scale, however, is not appropriate for comparing different patients, since pain is a very personal experience and varies greatly from patient to patient, but it can be helpful in comparing initial pain with pain at follow-up appointments to evaluate the success or failure of therapies.
Concomitant symptoms
All concomitant symptoms such as sensory, motor, or autonomic effects that accompany the pain should be included. Sensations such as hyperesthesia, hypoesthesia, anesthesia, paresthesia, or dysesthesia should be mentioned. Any concomitant change in the special senses affecting vision, hearing, smell, or taste should be noted. Motor changes expressed as muscular weakness, muscular contractions, or actual spasm should be recognized. Various localized autonomic symptoms should be observed and described. Ocular symptoms may include lacrimation, injection of the conjunctivae, pupillary changes, and edema of the lids. Nasal symptoms include nasal secretion and congestion. Cutaneous symptoms have to do with skin temperature, color, sweating, and piloerection. Gastric symptoms include nausea and indigestion.
Flow of the pain
The manner of flow yields important information by determining whether the individual pains are steady or paroxysmal. A flowing type of pain, even though variable in intensity or distinctly intermittent, is described as steady. Such pain is to be distinguished from paroxysmal pain, which characteristically consists of sudden volleys or jabs. The volleys may vary considerably in both intensity and duration. When they occur frequently, the pain may become nearly continuous.
Aggravating and alleviating factors
Effect of functional activities
The effect of functional activities should be observed and described. Common biomechanical functions include such activities as movement of the face, jaw, or tongue and the effects of swallowing, head position, and body position. The effect of activities such as talking, chewing, yawning, brushing the teeth, shaving, washing the face, turning the head, stooping over, or lying down should be noted. The effect of emotional stress, fatigue, and time of day also should be recorded.
The pain may be triggered by minor superficial stimulation such as touch or movement of the skin, lips, face, tongue, or throat. When pain is triggered by such activities, it is well to distinguish between stimulation of overlying tissues that are only incidentally stimulated and the result of functioning of the joints and muscles themselves. The former is triggered whereas the latter is induced pain. This distinction can usually be made by stabilizing the joints and muscles with a bite block to prevent their movement while the other structures are stimulated or moved. If uncertainty exists, the distinction can be made more positively by utilizing local anesthesia. Topical anesthesia of the throat effectively arrests triggering in the distribution of the glossopharyngeal nerve. Mandibular block anesthesia stops triggering from the lower lip and tongue. Infraorbital anesthesia arrests triggering from the upper lip and maxillary skin. None of these procedures prevents the induction of true masticatory pain.
Parafunctional activities should also be assessed. The patient should be questioned regarding bruxism, clenching, or any other oral habit. One should remember that often these activities occur at subconscious levels and the patient may not be reporting accurately (i.e., with regard to clenching and bruxing). Other habits are more readily reported (e.g., holding objects between the teeth, such as a pipe, a pencil, or other occupational implement). Habits that introduce extraoral forces are also identified, such as holding a telephone between the chin and shoulder, resting the mandible in the hands while sitting at a table, or playing certain musical instruments.2,3 Any force applied to the jaw (either intraorally or extraorally) must be identified as a potential contributing factor to the functional disturbance.4
Effect of physical modalities
The patient should be questioned regarding the effect of hot or cold on the pain condition. The patient should be asked if other modalities such as massage or transcutaneous electrical nerve stimulation have been tried and if so what the results were. The results of such therapies may shed light on the type and therapeutic responsiveness of the pain condition.
Medications
The patient should review all past and present medications taken for the pain condition. Dosages should be reported along with how often the medications were taken and their effectiveness in relieving the chief complaint. It is also helpful to know who prescribed these medications, since input from other providers may also shed light on the pain condition. Some very commonly used medications, such as oral contraceptives and estrogen replacements, may play a role in some pain conditions,5,6 although this is still debated.7
Emotional stress
As previously mentioned, emotional stress can play a significant role in functional disturbances of the masticatory system. While taking the history, the clinician should attempt to assess the level of emotional stress being experienced by the patient. This is often difficult to do. There are no conclusive questionnaires that can be used to identify whether high levels of emotional stress relate to the patient’s problem, nor can any emotional stress test be used to help diagnose or determine an effective treatment. Sometimes the course of the symptoms can be helpful. When symptoms are periodic, the patient should be questioned for any correlation between symptoms and high levels of emotional stress. A positive correlation is an important finding and will affect diagnosis and treatment. This represents another factor that can be identified only by taking a thorough history. The effect of emotional stress on the patient is also ascertained by questioning for the presence of other psychophysiologic disorders (e.g., irritable bowel syndrome, hypertension, colitis). Knowledge of the presence of these types of disorders helps document the effect of stress on the patient.
Sleep quality
There are relationships between some pain conditions and the quality of the patient’s sleep.8–11 It is important, therefore, that the quality of the patient’s sleep be reviewed. Patients should be asked how long it takes for them to fall asleep; how often they wake during the night; whether, if they wake up during the night, they can then get back to sleep easily; and whether they feel rested in the morning. Patients who report poor a quality of sleep should be questioned regarding the relationship of their sleep to the pain condition. Particular notice should be taken when the patient reports waking during the night in pain or when the pain actually wakes the patient.
Litigation and disability
During the interview it is important to inquire if the patient is involved in any form of litigation related to the pain complaint. This information may help the clinician better appreciate all the conditions surrounding the pain complaint. The presence of litigation does not directly imply a wish to achieve secondary gains, but this may be present.
A similar condition may exist with disability. If the patient is either receiving or applying for disability that will allow him or her not to work yet receive compensation, it may have a powerful effect on the individual’s desire to get well and return to work. Secondary gains may have a direct effect on the success or failure of treatment.
Past consultations and treatments
During the interview all previous consultations and treatments should be thoroughly discussed and reviewed. This information is extremely important so that the repetition of tests and therapies can be avoided. If information is incomplete or unclear, the previous treating clinician should be contacted and appropriate information requested. Clinical notes from previous treating clinicians can be extremely helpful in deciding future treatments.
When a patient reports previous treatments such as an occlusal appliance, the patient should be asked to bring the appliance to the evaluation appointment. The previous success of this treatment should be reported and the appliance evaluated. This evaluation may shed light on future treatment considerations.
Relationship to other pain complaints
As previously discussed, some patients may have more than one pain complaint. When more than one complaint is reported, the clinician must evaluate each aspect of each complaint separately. Once each complaint is evaluated according to all the criteria mentioned above, the relationship of the primary complaint to the others should be ascertained. Sometimes a pain complaint may actually be secondary to another complaint. In these instances effective management of the primary pain complaint will likely also resolve the secondary pain complaint. In other instances one complaint may be totally independent of another complaint. When this exists, individual therapy may have to be directed to each complaint. Identifying the relationship between these complaints is essential and best determined by the history.
Past medical history
Since pain can be a symptom related to many physical illnesses and disorders, it is essential that the past and present medical condition be carefully evaluated. Any past serious illnesses, hospitalizations, operations, medications, or other significant treatments should be discussed in light of the present pain complaint. The patient should be asked about any systemic conditions such as osteoarthritis, rheumatoid arthritis, or autoimmune/connective tissue disorders that may be related to the chief complaint. When indicated, treating physicians should be contacted for additional information. It may also be appropriate for the clinician to discuss any planned suggested treatment with the patient’s primary care physician when significant health problems are present.
Review of systems
A complete history should also include appropriate questions concerning the present status of the patient’s body systems. Questions should investigate the present health status of the cardiovascular (including lungs), digestive, renal, and liver systems, as well as the peripheral and central nervous systems. Any abnormalities should be noted and any relationship with the pain complaint should be determined.
Psychological assessment
As pain becomes more chronic, psychological factors relating to the pain complaint become more predominant. Routine psychological evaluation may not be necessary with acute pain; however, with chronic pain, it becomes essential. It may be difficult for the general practitioner to confidently evaluate psychological factors. For this reason, chronic pain patients are best evaluated and managed by a multidisciplinary approach.
A variety of measuring tools can be used to assess a patient’s psychological status. One of these is the Multidimensional Pain Inventory (MPI), developed by Turk and Rudy.12 This scale evaluates how the pain experience is affecting the patient. It classifies the patient into one of three pain profiles: adaptive coping, interpersonal distress, and dysfunctional chronic pain. Dysfunctional chronic pain is a profile of severe pain, functional disability, psychological impairment, and low perceived life control.
Another useful tool is the Symptom Check List 90 (SCL-90).13 This evaluation provides an assessment of the following nine psychological states: somatization, obsessive-compulsive behavior, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism. Assessing these factors is essential in evaluating the chronic pain patient.
Often the general practitioner may not have immediate access to psychological evaluation support. In this instance the practitioner may elect to use the TMJ scale.14,15 This scale was developed for use in the private dental practice to assist in evaluating clinical and certain psychological factors associated with orofacial pain. This scale can assist the dentist in identifying whether psychological issues are an important aspect of the patient’s pain condition. Although this scale is helpful, it is not as complete as the other psychological tests mentioned above and certainly does not replace the personal evaluation of a clinical psychologist.
Clinical Examination
Once the history has been obtained and thoroughly discussed with the patient, a clinical examination is performed. It should identify any variations from the normal health and function of the masticatory system.
Because of the complexity of head and neck pain disorders, it is important that certain nonmasticatory structures be at least grossly examined for the purpose of ruling out other possible disorders.16 Even before one examines the masticatory structures, it is important to evaluate gross function of the cranial nerves and the eyes, ears, and neck. If abnormal findings are identified, an immediate referral to the appropriate specialty is indicated.
Cranial nerve examination
The 12 cranial nerves supply sensory information to and receive motor impulses from the brain. Any gross problem relating to their function must be identified that so abnormal conditions can be immediately and appropriately addressed. Treating a neurologic problem with dental techniques will not only fail to solve the problem but also is likely to be hazardous because appropriate treatment may then be delayed. The dentist need not be trained as a neurologist. In fact, the cranial nerve examination does not have to be complex. Any therapist who regularly evaluates pain problems can test the gross function of the cranial nerves, which can help rule out neurologic disorders. The following simple evaluation procedures can be used in assessing each nerve.
The olfactory nerve
The first cranial nerve has sensory fibers originating in the mucous membrane of the nasal cavity and provides the sensation of smell. It is tested by asking the patient to detect differences between the odors of peppermint, vanilla, and chocolate. (It is helpful to have these available in the office for testing.) It must also be determined whether the patient’s nose is obstructed. This can be done by asking the patient to exhale nasally onto a mirror. Fogging of the mirror from both nostrils denotes adequate airflow.
The optic nerve
The second cranial nerve, also sensory, with fibers originating in the retina, serves for sight. It is tested by having the patient cover one eye and read a few sentences. The other eye is checked in the same manner. The examiner assesses the visual field by standing behind the patient and slowly bringing his or her fingers from behind around into view (Figure 9-2). The patient should report when the fingers are first seen. Normally there is no variation between the right and left eyes when this test is done.
The oculomotor, trochlear, and abducens nerves
The third, fourth, and sixth cranial nerves, supplying motor fibers to the extraocular muscles, are tested by having the patient follow the examiner’s finger as it makes an X (Figure 9-3). Both eyes should move smoothly and similarly as they follow the finger. The pupils should be of equal size and rounded and should react to light by constricting. The accommodation reflex is tested by having the patient change focus from a distant to a near object. The pupils should constrict as the object (the finger) approaches the patient’s face. Not only should they both constrict to direct light, but each should also constrict to light directed in the other eye (consensual light reflex) (Figure 9-4).
The trigeminal nerve
The fifth cranial nerve is both sensory (from the face, scalp, nose, and mouth) and motor (to the muscles of mastication). Sensory input is tested by lightly stroking the face with a cotton-tipped applicator bilaterally in three regions: forehead, cheek, and lower jaw (Figure 9-5). This will give a rough idea of the function of the ophthalmic, maxillary, and mandibular branches of the trigeminal nerve. The patient should describe similar sensations on each side. The trigeminal nerve also contains sensory fibers from the cornea. The corneal reflexes can be tested by observing the patient’s blink in response (nerve VII) to a light touch on the cornea (nerve V) with a sterile cotton pledget or tissue. Gross motor input is tested by having the patient clench the teeth while the examiner feels both the masseter and temporal muscles (Figure 9-6). The muscles should contract equally bilaterally.
The facial nerve
The seventh cranial nerve is also sensory and motor. The sensory component, supplying taste sensations from the anterior portion of the tongue, is tested by asking the patient to distinguish between sugar and salt using just the tip of the tongue. The motor component, which innervates the muscles of facial expression, is tested by asking the patient to raise both eyebrows, smile, and show the lower teeth. During these movements, any differences between the two sides are recorded.
The acoustic nerve
Also called the vestibulocochlear nerve, the eighth cranial nerve supplies the senses of balance and hearing. The patient should be questioned regarding any recent changes in upright posture or in hearing, especially if they were associated with the problem that initiated the office visit. If there is a question regarding balance, ask the patient to walk heel to toe along a straight line. Gross hearing can be evaluated by rubbing a strand of hair between your first finger and thumb near the patient’s ear and noting any difference between right and left sensitivities (Figure 9-7).
The glossopharyngeal and vagus nerves
The ninth and tenth cranial nerves are tested together because they both supply fibers to the back of the throat. The patient is asked to say “ah” and the soft palate is observed for symmetrical elevations. The gag reflex is tested by touching each side of the pharynx.
The accessory nerve
The spinal accessory nerve supplies fibers to the trapezius and sternocleidomastoid muscles. The motor input to the trapezius is tested by asking the patient to shrug the shoulders against resistance. The sternocleidomastoid is tested by having the patient move the head first to the right and then to the left against resistance (Figure 9-8). Any differences in muscle strength are then noted.
The hypoglossal nerve
The twelfth cranial nerve supplies motor fibers to the tongue. To test it, the patient is asked to protrude the tongue; any uncontrolled or consistent lateral deviation is then noted. The strength of the tongue can also be evaluated by having the patient push laterally against a tongue blade.
As previously stated, any abnormalities found during the cranial nerve examination should be viewed as important and an appropriate medical referral should be made.
Eye examination
The patient is questioned regarding his or her vision and any recent changes, especially any associated with the reason for seeking treatment. As in the cranial nerve examination, simple techniques will be sufficient in testing gross vision. The patient’s left eye is covered and he or she is asked to read a few sentences from a paper. The other eye is then similarly examined. Any diplopia or blurriness of vision is noted as well as whether this relates to the pain problem. Pain felt in or around the eyes is noted and whether or not reading affects it. Reddening of the conjunctivae should be recorded, along with any tearing or swelling of the eyelids.
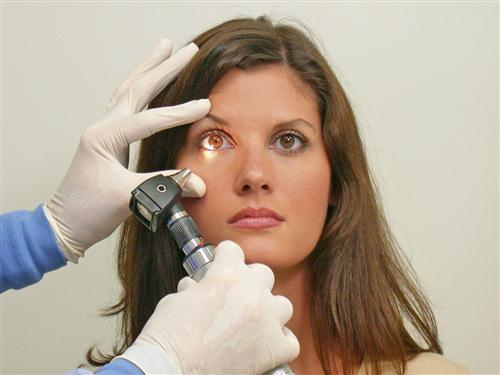
Ear examination
Approximately 70% of patients reporting with TMJ pain also complain of ear discomfort. The proximity of the ear to the TMJ and muscles of mastication as well as their common trigeminal innervation creates a frequent condition for referral of pain. Although few of these patients have actual ear disease, when they do it is important to identify it and refer them for proper treatment. Any dentist who treats TMDs should become proficient at examining the ear for gross pathology. Hearing should be checked, as in the examination of the eighth cranial nerve. Infection of the external auditory meatus (otitis externa) can be identified by simply pushing inward on the tragus. If this causes pain, there could be an external ear infection and the patient should be referred to an otolaryngologist. An otoscope will be necessary to visualize the tympanic membrane for inflammation, perforations, or fluid (Figure 9-9).
The dentist’s role should be merely to attempt to rule out gross ear disease with an otologic examination. Any questionable findings should be referred to an otolaryngologist for a more thorough evaluation. On the other hand, normal findings from an otologic examination may be taken as encouragement to continue to search for the true source of pain or dysfunction.
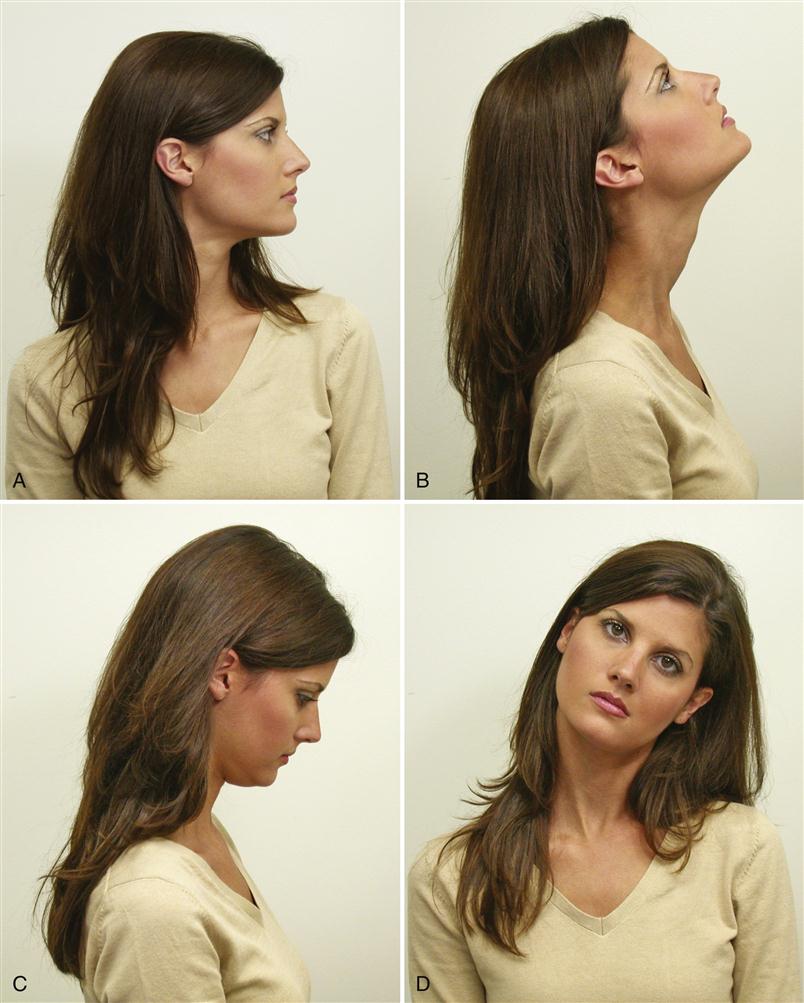
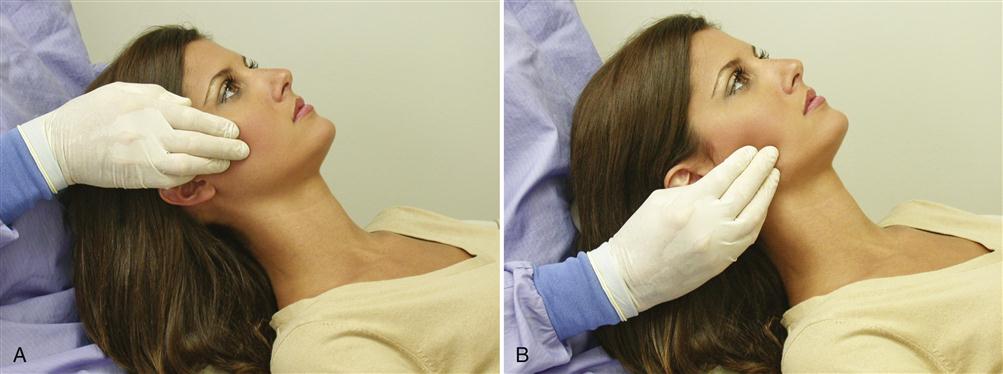
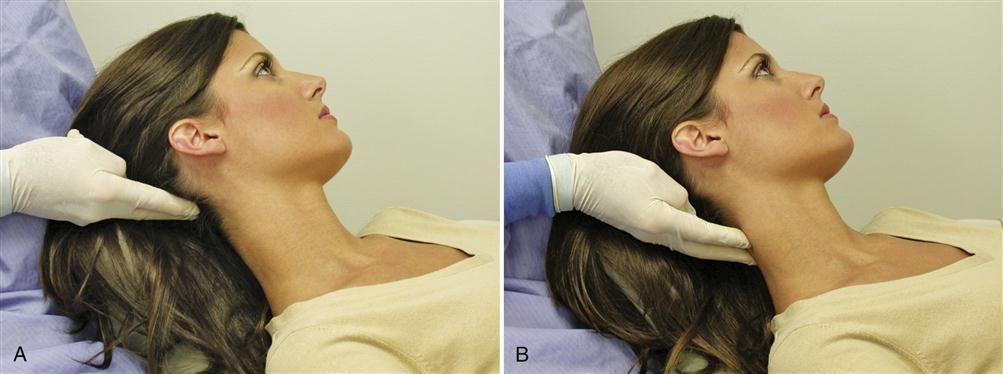
Cervical examination
As described in Chapter 2, cervicospinal pain and dysfunction can refer pain to the masticatory apparatus. Since this is a frequent occurrence, it is important to evaluate the neck for pain or movement difficulties. A simple screening examination for craniocervical disorders is easily accomplished. The mobility of the neck is examined for range and symptoms. The patient is asked to look first to the right and then to the left (Figure 9-10, A). There should be at least 70 degrees of rotation in each direction.17 Next the patient is asked to look upward as far as possible (extension) (Figure 9-10, B) and then downward as far as possible (flexion) (Figure 9-10, C). The head should normally extend backward some 60 degrees and flex downward 45 degrees.17 Finally, the patient is asked to bend the neck to the right and then to the left (Figure 9-10, D). This should be possible to approximately 40 degrees each way.17 Any pain is recorded and any limitation of movement carefully investigated to determine whether its source is a muscular or a vertebral problem. When patients with limited range of movement can be passively stretched to a greater range, the source is usually muscular. Patients with vertebral problems cannot normally be stretched to a greater range. If the clinician suspects that the patient has a craniocervical disorder, proper referral for a more complete (cervicospinal) evaluation is indicated. This is very important, since craniocervical disorders can be closely associated with TMD symptoms.18–20
Once the cranial nerves, eyes, ears, and cervicospinal area have been evaluated, the masticatory apparatus is examined. The masticatory examination consists of evaluating three major structures: the muscles, joints, and teeth. A muscle examination is used to evaluate the health and function of the muscles. A TMJ examination is used to evaluate the health and function of the joints. An occlusal examination is used to evaluate the health and function of the teeth and their supportive structures.
Muscle Examination
Pain is not associated with the normal function or palpation of a healthy muscle. In contrast, a frequent clinical sign of compromised muscle tissue is pain. The condition that brings about compromise or unhealthy muscle tissue may be muscle overuse or physical trauma such as overstretching or receiving a blow to the muscle tissue itself. Most often the muscles of mastication become compromised through increased activity. As the number and duration of contractions increase, so also do the physiologic needs of the muscle tissues. Increased muscle tonicity or hyperactivity, however, can lead to a decrease in blood flow to the muscle tissues, lowering the inflow of nutrient substances needed for normal cell function while also accumulating metabolic waste products. This accumulation of metabolic waste products and of other algogenic substances is thought to cause the muscle pain.21,22 It is now appreciated that the central nervous system can contribute to the myalgia associated with neurogenic inflammation.21,23
In its early stages myalgia is noticed only during function of the muscle. If sustained hyperactivity continues, it can be long lasting and result in a dull, aching pain that often radiates over the entire muscle. The pain can eventually become severe enough to limit mandibular function. The degree and location of muscle pain and tenderness are identified during a muscle examination. The muscle can be examined by direct palpation or by functional manipulation.
Muscle palpation
A widely accepted method of determining muscle tenderness and pain is by digital palpation.24–26 A healthy muscle does not elicit sensations of tenderness or pain when palpated. Deformation of compromised muscle tissue by palpation can elicit pain.27 Therefore if a patient reports discomfort during palpation of a specific muscle, it can be deduced that the muscle tissue has been compromised by either trauma or fatigue.
Palpation of the muscle is accomplished mainly by the palmar surface of the middle finger, with the index finger and forefinger testing the adjacent areas. Soft but firm pressure is applied to the designated muscles, with the fingers compressing the adjacent tissues in a small circular motion. A single firm thrust of 1 or 2 s duration is usually better than several light thrusts. During palpation the patient is asked whether it hurts or is just uncomfortable.
For the muscle examination to be most helpful, the degree of discomfort is ascertained and recorded. This is often a difficult task. Pain is subjective and is perceived and expressed quite differently from patient to patient. Yet the degree of discomfort in the structure can be important in recognizing the patient’s pain problem as well as an excellent method of evaluating treatment effects. An attempt is made, therefore, not only to identify the affected muscles but also to classify the degree of pain in each. When a muscle is palpated, the patient’s response is placed in one of four categories.28,29 A zero (0) is recorded when the muscle is palpated and no pain or tenderness is reported by the patient. A number 1 is recorded if the patient responds that the palpation is uncomfortable (tenderness or soreness). A number 2 is recorded if the patient experiences definite discomfort or pain. A number 3 is recorded if the patient shows evasive action or eye tearing or verbalizes a desire not to have the area palpated again. The pain or tenderness of each muscle is recorded on an examination form, which will assist diagnosis and later be used in the evaluation and assessment of progress.
A thorough muscle examination should identify not only generalized muscle tenderness and pain but also the localized, firm, hypersensitive bands of muscle tissue (trigger points) indicative of myofascial pain. As stated in Chapters 2 and 8, trigger points act as sources of deep pain input that can produce central excitatory effects. It is important that these areas be identified and recorded. To locate trigger points, the examiner palpates the entire body of each muscle. Generalized muscle pain may not exist in a muscle with trigger points. In recording examination findings, it is important to differentiate between generalized muscle pain and trigger-point pain, since the diagnosis and treatment are often different.
When trigger points are located, an attempt should be made to determine if there is any pattern of pain referral. Pressure should be applied to the trigger point for 4 to 5 s, and the patient is then asked if the pain is felt to radiate in any direction. If a pattern of referred pain is reported, it should be noted on a drawing of the face for future reference. Patterns of referred pain are often helpful in identifying and diagnosing certain pain conditions.
A routine muscle examination includes palpation of the following muscles or muscle groups: temporalis, masseter, sternocleidomastoid, and posterior cervical (e.g., the splenius capitis and trapezius). For increased efficiency of the examination, both the right and left muscles are palpated simultaneously. The technique of palpating each muscle is described below. An understanding of the anatomy and function of the muscles is essential for proper palpation (Chapter 1).
The muscle examination also includes evaluation of the medial and lateral pterygoids by functional manipulation. This technique is used for muscles that are impossible or nearly impossible to palpate manually.
The temporalis
The temporalis is divided into three functional areas, each of which is independently palpated. The anterior region is palpated above the zygomatic arch and anterior to the TMJ (Figure 9-11, A). Fibers of this region run essentially in a vertical direction. The middle region is palpated directly above the TMJ and superior to the zygomatic arch (Figure 9-11, B). Fibers in this region run in an oblique direction across the lateral aspect of the skull. The posterior region is palpated above and behind the ear (Figure 9-11, C). These fibers run in an essentially horizontal direction.
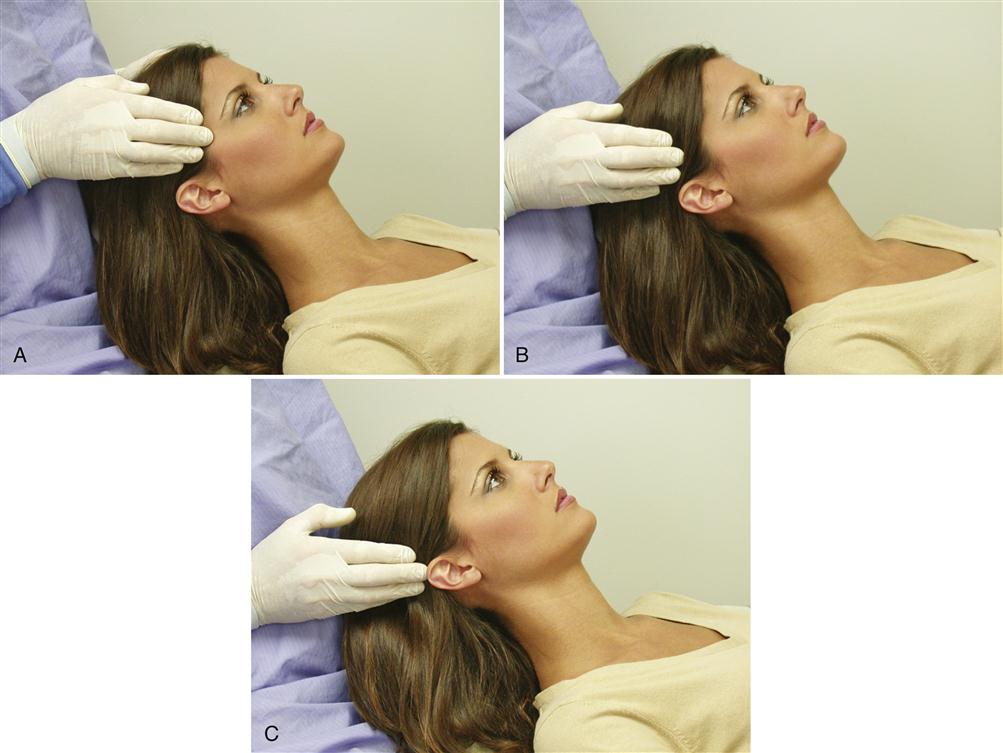
If uncertainty arises regarding the proper finger placement, the patient is asked to clench the teeth. The temporalis will then contract and the fibers should be felt beneath the examiner’s fingertips. It is helpful to be positioned behind the patient and to use the right and left hands to palpate respective muscle areas simultaneously. During palpation of each area, the patient is asked whether it hurts or is just uncomfortable and the response is classified as 0, 1, 2, or 3, according to the previously described criteria. If a trigger point is located, it should be identified on the exam form along with any pattern of referral.
In evaluating the temporalis muscle, it is important also to palpate its tendon. The fibers of the temporalis muscle extend inferiorly to converge into a distinct tendon that attaches to the coronoid process of the mandible. It is common for some TMDs to produce a temporalis tendinitis, which can create pain in the body of the muscle as well as referred pain behind the adjacent eye (retro-orbital pain). The tendon of the temporalis is palpated by placing the finger of one hand intraorally on the anterior border of the ramus and the finger of the other hand extraorally on the same area. The intraoral finger is moved up the anterior border of the ramus until the coronoid process and tendon are palpated (Figure 9-12). The patient is asked to report any discomfort or pain.
The masseter
The masseter is palpated bilaterally at its superior and inferior attachments. First, the fingers are placed on each zygomatic arch (just anterior to the TMJ). They are then dropped down slightly to the portion of the masseter attached to the zygomatic arch, just anterior to the joint (Figure 9-13, A). Once this portion (the deep masseter) has been palpated, the fingers drop to the inferior attachment on the inferior border of the ramus. The area of palpation is directly above the attachment of the body of the masseter (i.e., the superficial masseter) (Figure 9-13, B). The patient’s response is recorded.
The sternocleidomastoid
Although the sternocleidomastoid (SCM) does not function directly in moving the mandible, it is specifically mentioned because it often becomes symptomatic with TMDs and is easily palpated. The palpation is done bilaterally near its insertion on the outer surface of the mastoid fossa, behind the ear (Figure 9-14, A). The entire length of the muscle is palpated, down to its origin near the clavicle (Figure 9-14, B). The patient is asked to report any discomfort during the procedure. Also, any trigger points found in this muscle are noted, since they are frequent sources of referred pain to the temporal, joint, and ear area.
The posterior cervical muscles
The posterior cervical muscles (trapezius, longissimus [capitis and cervicis], splenius [capitis and cervicis], and levator scapulae) do not directly affect mandibular movement; however, they do become symptomatic during certain TMDs and therefore are routinely palpated. They originate at the posterior occipital area and extend inferiorly along the cervicospinal region. Because they are layered over each other, they are sometimes difficult to identify individually.
In palpating these muscles, the examiner’s fingers slip behind the patient’s head. Those of the right hand palpate the right occipital area and those of the left hand palpate the left (Figure 9-15, A), at the origins of the muscles. The patient is questioned regarding any discomfort. The fingers move down the length of the neck muscles through the cervical area (Figure 9-15, B), and any patient discomfort is recorded. It is important to be aware of trigger points in these muscles, since they are a common source of frontal headache.
The splenius capitis is palpated for general pain or tenderness as well as for trigger points. Its attachment to the skull is a small depression just posterior to the attachment of the SCM (Figure 9-16). Palpation is begun at this point and moves inferiorly until the muscle blends into the other neck muscles. Any pain, tenderness, or trigger points are recorded.
The trapezius is an extremely large muscle of the back, shoulder, and neck; like the SCM and the splenius, it does not directly affect jaw function but is a common source of headache pain and is easily palpated. The major purpose of its palpation is not to evaluate shoulder function but to search for active trigger points that may be producing referred pain. The trapezius commonly has trigger points that refer pain to the face. In fact, when facial pain is the patient’s chief complaint, this muscle should be one of the first sources investigated. The upper part is palpated from behind the SCM inferolaterally to the shoulder (Figure 9-17) and any trigger points are recorded.
Clinical significance of trigger points
As discussed in Chapter 2, trigger points can be either active or latent. When active, they are clinically identified as specific hypersensitive areas within the muscle tissue. Often a small firm tight band of muscle tissue can be felt. When latent, they are not detectable. Active trigger points are frequently a source of constant deep pain and produce central excitatory effects.30,31 When referred (heterotopic) pain is detected, the clinician should remember that this pain is wholly dependent on the conditions of the trigger points (the source of the pain). This means that when active referring trigger points are provoked, the referred pain will be increased. This finding becomes a significant diagnostic observation in relating the pain complaint to its source. For example, when a patient’s chief complaint is headache, careful palpation of the aforementioned neck muscles for trigger points will demonstrate its source. When a trigger point is located, applying pressure to it will usually increase the headache (referred) pain.
The specific pattern of referred pain from various trigger-point locations has been outlined by Travell and Simons31 (see Chapter 8). An understanding of these common referral sites may help the clinician who is attempting to diagnose a facial pain problem. As discussed in Chapter 10, anesthetic blocking of the trigger point often eliminates the referred headache pain and thus becomes a helpful diagnostic tool.
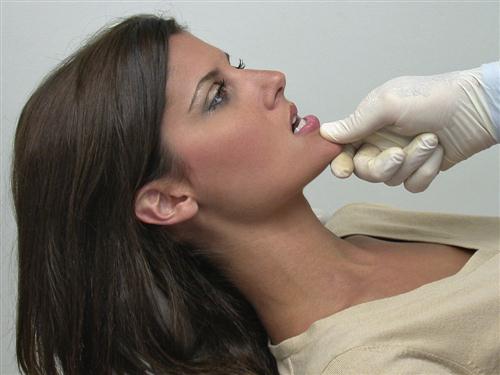
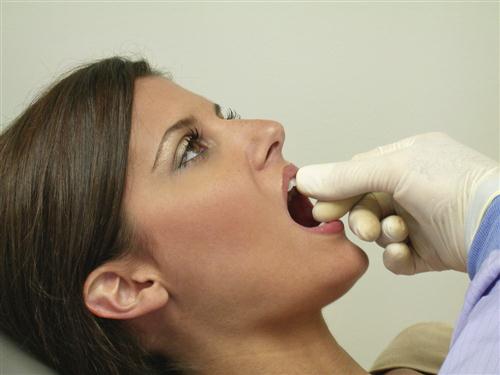
Functional manipulation
Three muscles that are basic to jaw movement but impossible or nearly impossible to palpate are the inferior lateral pterygoid, superior lateral pterygoid, and medial pterygoid. The inferior and superior lateral pterygoids reside deep within the skull, originating on the lateral wing of the sphenoid bone and the maxillary tuberosity and inserting on the neck of the mandibular condyle and the TMJ capsule. The medial pterygoid has a similar origin, but it extends downward and laterally to insert on the medial surface of the angle of the mandible. Although the medial pterygoid can be palpated by placing the finger in the lateral aspect of the pharyngeal wall of the throat, this palpation is difficult and sometimes uncomfortable for the patient (owing to the gag reflex). All three muscles receive their innervation from the mandibular branch of the trigeminal nerve (cranial nerve V).
For years an intraoral technique was suggested for palpating the lateral pterygoid muscle, but this has not proven effective.32,33 Since the location of this muscle makes palpation impossible, a second method for evaluating muscle symptoms, called functional manipulation, was developed based on the principle that as a muscle becomes fatigued and symptomatic, further function will elicit more pain.21,27,34,35 Thus a muscle that is compromised by excessive activity is painful both during contraction and when being stretched; in these cases functional manipulation is the only technique for evaluating whether it is indeed a source of deep pain.
In some instances palpation in the region of the lateral and medial pterygoids may elicit pain; however, functional manipulation does not. A study36 comparing the results of palpation and functional manipulation of the inferior lateral pterygoid muscle showed that 27% of a control group had tenderness to intraoral palpation but none had symptoms following functional manipulation. This implied that 27% of the time a false-positive result was being reported with palpation. In the same study a group of orofacial pain patients was similarly examined and 69% were found to have inferior lateral pterygoid pain with a palpation technique, yet only 27% had pain with functional manipulation. In other words, when palpation was used, the inferior lateral pterygoid was blamed for pain 42% of the time although it was not actually the source. There is no question that when the area posterior to the maxillary tuberosity is palpated, there is a high incidence of pain; functional manipulation merely suggests that this pain is not from the lateral pterygoids but that other structures are likely responsible.
During functional manipulation, each muscle is contracted and then stretched. If the muscle is a true source of pain, both activities will increase the pain. The following section reviews the functional manipulation techniques for the evaluation of three muscles that are difficult to palpate reliably: the inferior lateral pterygoid, the superior lateral pterygoid, and the medial pterygoid.
Functional manipulation of the inferior lateral pterygoid muscle
Contraction
When the inferior lateral pterygoid contracts, the mandible is protruded and/or the mouth is opened. Functional manipulation is best accomplished by having the patient make a protrusive movement, since this muscle is the primary protruding muscle. It is also active during opening, but so are other muscles, which adds confusion to the findings. The most effective manipulation, therefore, is to have the patient protrude against resistance provided by the examiner (Figure 9-18). If the inferior lateral pterygoid is the source of pain, this activity will increase the pain.
Stretching
The inferior lateral pterygoid stretches when the teeth are in maximum intercuspation. Therefore if it is the source of pain when the teeth are clenched, the pain will increase. When a tongue blade is placed between the posterior teeth, the intercuspal position (ICP) cannot be reached; therefore the inferior lateral pterygoid does not fully stretch. Consequently biting on a separator does not increase the pain but may even decrease or eliminate it.
Functional manipulation of the superior lateral pterygoid muscle
Contraction
The superior lateral pterygoid contracts with the elevator muscles,∗ especially during a power stroke (clenching). Therefore if it is the source of pain, clenching will increase the pain. If a tongue blade is placed between the posterior teeth bilaterally (Figure 9-19) and the patient clenches on the separator, pain again increases with contraction of the superior lateral pterygoid. These observations are exactly the same as for the elevator muscles. Stretching is needed to enable superior lateral pterygoid pain to be distinguished from elevator pain.
Stretching
As with the inferior lateral pterygoid, stretching of the superior lateral pterygoid occurs at maximal intercuspation. Therefore stretching and contraction of this muscle occur during the same activity, clenching. If the superior lateral pterygoid is the source of pain, clenching will increase it. Superior lateral pterygoid pain can be differentiated from elevator pain by having the patient open wide. This will stretch the elevator muscles but not the superior lateral pterygoid. If opening elicits no pain, then the pain of clenching is from the superior lateral pterygoid. If the pain increases during opening, then both the superior lateral pterygoid and the elevators may be involved. It is often difficult to differentiate pain in the former from pain in the latter unless the patient can isolate the location of the painful muscle.
Functional manipulation of the medial pterygoid muscle
Contraction
The medial pterygoid is an elevator muscle and therefore contracts as the teeth are coming together. If it is the source of pain, clenching the teeth together will increase the pain. When a tongue blade is placed between the posterior teeth and the patient clenches against it, the pain is still increased since the elevators are still contracting.
Stretching
The medial pterygoid also stretches when the mouth is opened wide. Therefore if it is the source of pain, opening the mouth wide will increase the pain.
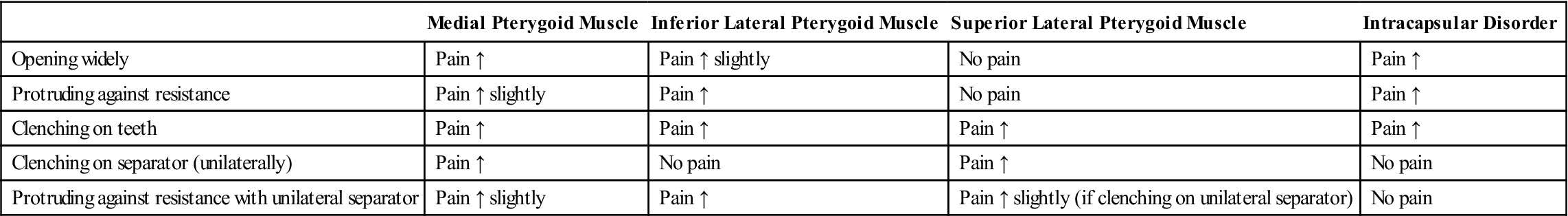
Functional manipulation of muscles that are impossible to palpate can provide accurate information regarding the source of masticatory pain. All the information needed is obtained by having the patient open wide, protrude the mandible against resistance, clench the teeth, and then bite on a separator. The response of each muscle to functional manipulation is summarized in Table 9-1.
TABLE 9-1
Functional Manipulation by Muscle
| Contracting | Stretching | |
| Inferior lateral pterygoid muscle | Protruding against resistance, ↑ pain | Clenching on teeth, ↑ pain |
| Clenching on separator, no pain | ||
| Superior lateral pterygoid muscle | Clenching on teeth, ↑ pain | Clenching on teeth, ↑ pain |
| Clenching on separator, ↑ pain | Clenching on separator, ↑ pain | |
| Opening mouth, no pain | ||
| Medial pterygoid muscle | Clenching on teeth, ↑ pain | Opening mouth, ↑ pain |
| Clenching on separator, ↑ pain |
If a muscle is a true source of pain, functional manipulation will be helpful in identifying this source. However, the fact that pain is produced during functional manipulation does not necessarily mean that a source of pain has been identified. Referred symptoms such as secondary hyperalgesia can create painful symptoms during muscle function. In this instance functional manipulation identifies only the site of pain and not the source.37 Anesthetic blocking may be necessary to differentiate the source of pain from the site (Chapter 10).
Intracapsular disorders
There is another source of pain that can confuse these functional manipulation findings. Intracapsular disorders of the TMJ (e.g., a functional dislocation of the disc, an inflammatory disorder) can elicit pain with increased interarticular pressure and movement. Functional manipulation both increases interarticular pressure and moves the condyle. Therefore this pain is easily confused with muscle pain. For example, if an inflammatory disorder exists and the patient opens wide, pain is increased as a result of movement and function of the inflamed structures. If the mandible is protruded against resistance, pain is also increased, since movement and interarticular pressure are causing force to be applied to the inflamed structures. If the teeth are clenched, pain is again increased with the increased interarticular pressure and force to the inflamed structures. If, however, the patient clenches unilaterally on a separator, the interarticular pressure is decreased on the ipsilateral side and pain in that joint is decreased (Figure 9-20).
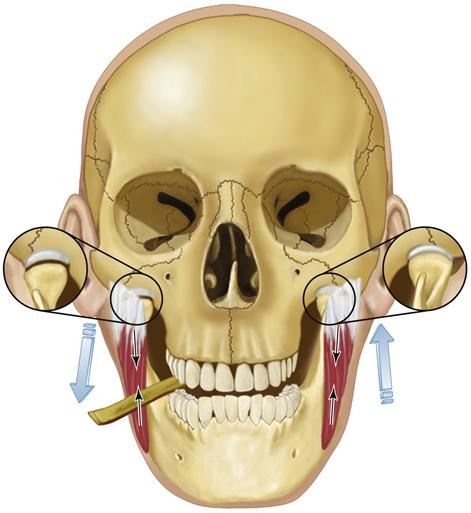
These results are logical but confusing since they are the same results found when the inferior lateral pterygoid is the site of pain. Therefore a fifth test must be administered to differentiate inferior lateral pterygoid pain from intracapsular pain. This can be done by placing a separator between the posterior teeth on the painful side. The patient is asked to close on the separator and then protrude the mandible against resistance. If an intracapsular disorder is the source of pain, the pain will not increase (or possibly even decrease), since closing on a separator decreases the interarticular pressure and thus reduces the forces to the inflamed structures. Contraction of the inferior lateral pterygoid, however, is increased during resistant protrusive movement and therefore pain will increase if this is its source of origin.
The four basic functional manipulation activities, along with the activity necessary to differentiate intracapsular pain, are listed in Tables 9-1 and 9-2. The potential sites or sources of pain are also listed as well as how each will react to functional manipulation.
TABLE 9-2
Functional Manipulation by Activity
| Medial Pterygoid Muscle | Inferior Lateral Pterygoid Muscle | Superior Lateral Pterygoid Muscle | Intracapsular Disorder | |
| Opening widely | Pain ↑ | Pain ↑ slightly | No pain | Pain ↑ |
| Protruding against resistance | Pain ↑ slightly | Pain ↑ | No pain | Pain ↑ |
| Clenching on teeth | Pain ↑ | Pain ↑ | Pain ↑ | Pain ↑ |
| Clenching on separator (unilaterally) | Pain ↑ | No pain | Pain ↑ | No pain |
| Protruding against resistance with unilateral separator | Pain ↑ slightly | Pain ↑ | Pain ↑ slightly (if clenching on unilateral separator) | No pain |
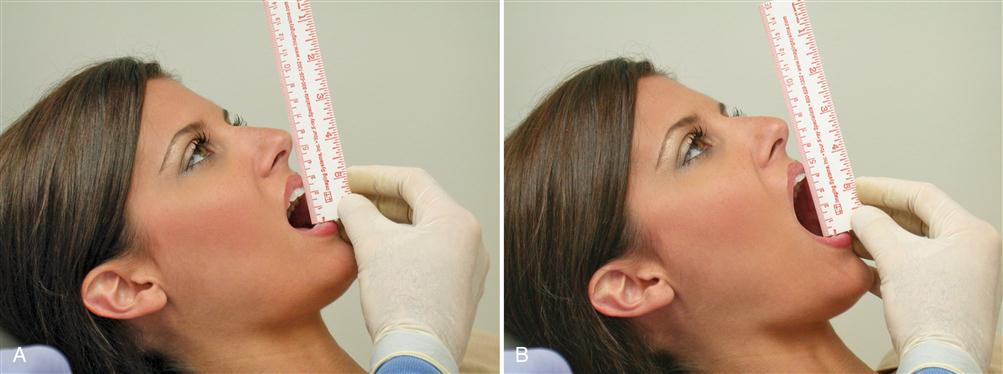
Maximal interincisal distance
A muscle examination is not complete until the effect of muscle function on mandibular movement has been evaluated. The normal range38 of mouth opening when measured interincisally is between 53 and 58 mm. Even a 6-year-old child can normally open to a maximum 40 mm or more.39,40 Since muscle symptoms are often accentuated during function, it is common for people to assume a restricted pattern of movement. The patient is asked to open slowly until pain is first felt (Figure 9-21, A). At that point the distance between the incisal edges of the maxillary and mandibular anterior teeth is measured. This is the maximal comfortable opening. The patient is next asked to open the mouth maximally even if it is painful (Figure 9-21, B). This is recorded as the maximal opening. In the absence of pain, the maximal comfortable opening and maximal opening are the same.
A restricted mouth opening is considered to be any distance less than 40 mm. Only 1.2% of young adults41 open less than 40 mm. One must remember, however, that 15% of the healthy elderly population41 open less than 40 mm. Less than 40 mm of mouth opening, therefore, seems to represent a reasonable point at which to designate restriction, but one should always consider the patient’s age and body size. This distance is measured by observing the incisal edge of the mandibular central incisor traveling away from its position at maximum intercuspation. If a person has a 5-mm vertical overlap of the anterior teeth and the maximum interincisal distance is 57 mm, the mandible has actually moved 62 mm in opening. In people who have extremely deep bites, these measurements must be considered in determining normal range of movement.
If mouth opening is restricted, it is helpful to test the end feel. This term describes the characteristics of the restriction that limits the full range of joint movement.42 The end feel can be evaluated by placing the fingers between the patient’s upper and lower teeth and applying gentle but steady force in an attempt to passively increase the interincisal distance (Figure 9-22). If the end feel is “soft,” increased opening can be achieved, but it must be done slowly. A soft end feel suggests muscle-induced restriction.43 If no increase in opening can be achieved, the end feel is said to be “hard.” Hard end feels are more likely associated with intracapsular sources (e.g., a disc dislocation).
The patient is next instructed to move the mandible laterally. Any lateral movement less than 8 mm is recorded as a restricted movement (Figure 9-23). Protrusive movement is also evaluated in a similar manner.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses