Direct Composite Restorations
Overview
Over the last 15 years socioeconomic changes, decreased caries prevalence, the greater esthetic demands of patients, and finally the controversy about the potential toxicity of amalgam have contributed to the introduction of new materials and the development of new techniques for esthetic restorations in the posterior, which are being used alongside traditional restorative materials and are progressively replacing them (Nathanson, 1991).
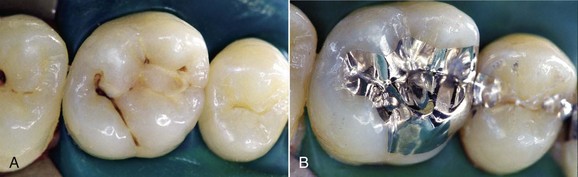
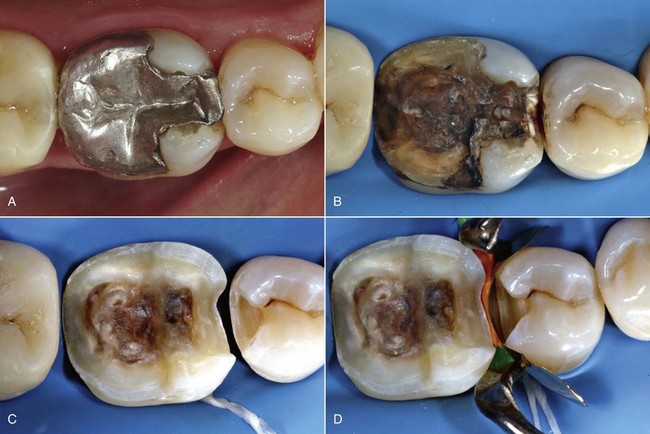
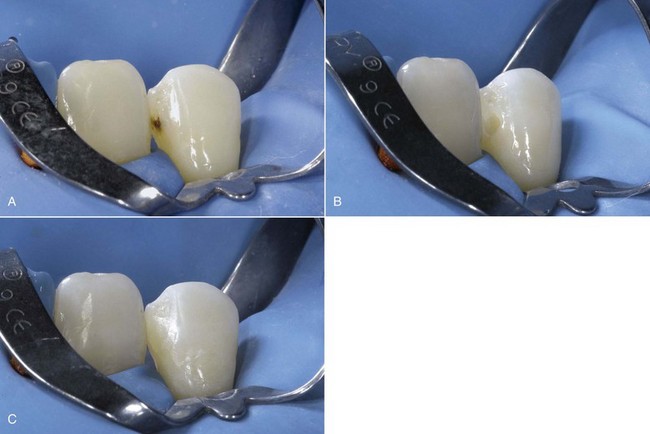
In the early 1990s the Geneva School still recommended the use of silver amalgam even for small Class II restorations up to the distal surface of the canine (Figure 9-1).

Figure 9-1 Small Class II restoration performed in 1993 according to the principles of the Geneva School.
Today tooth restoration techniques are radically different from those employed 15 years ago. Conservative dentistry has undergone a radical change, and today rehabilitation with adhesive techniques—following a strict operative protocol—of posterior teeth with medium and large carious lesions, and even with cuspal coverage, is considered correct and beneficial (Figure 9-2).
Reasons for Employing Adhesive Dentistry in the Posterior
The indications for use of amalgam are limited to few cases (see Chapter 5), essentially because esthetic adhesive composites have evolved considerably and offer significant advantages (Dietschi and Spreafico, 1997). They are tissue sparing, they strengthen the residual dental tissues, they ensure good esthetics, and they permit reintervention.
Tissue-Sparing Principle
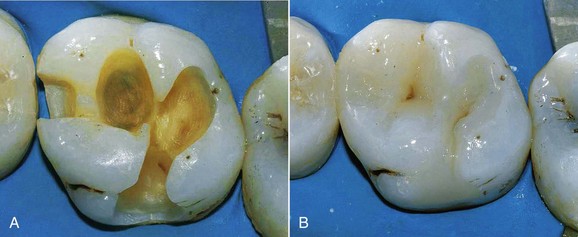
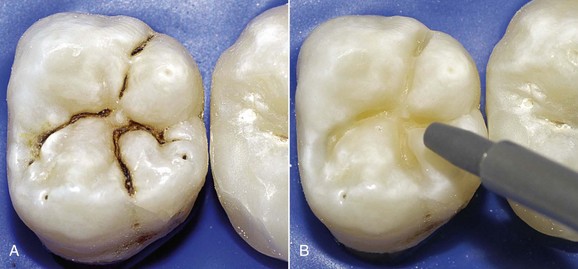
The need to perform composite restorations in the posterior is largely connected with the tissue-sparing principle—that is, the minimal sacrifice of sound hard tissues that results in an adhesive cavity rather than a conventional preparation (Figures 9-3 and 9-4).
Reinforcement of the Residual Tooth Structure
The current trend is to restore the elastic properties of lost dentin by using composite materials with microhardness (a parameter related to the modulus of elasticity) very similar to that of dentin (Lutz, 1986) (Figure 9-5). This technique is used particularly for the restoration of endodontically treated teeth.
Esthetics
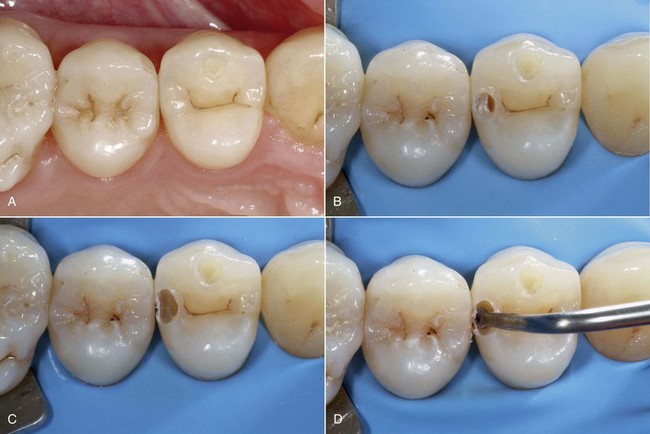
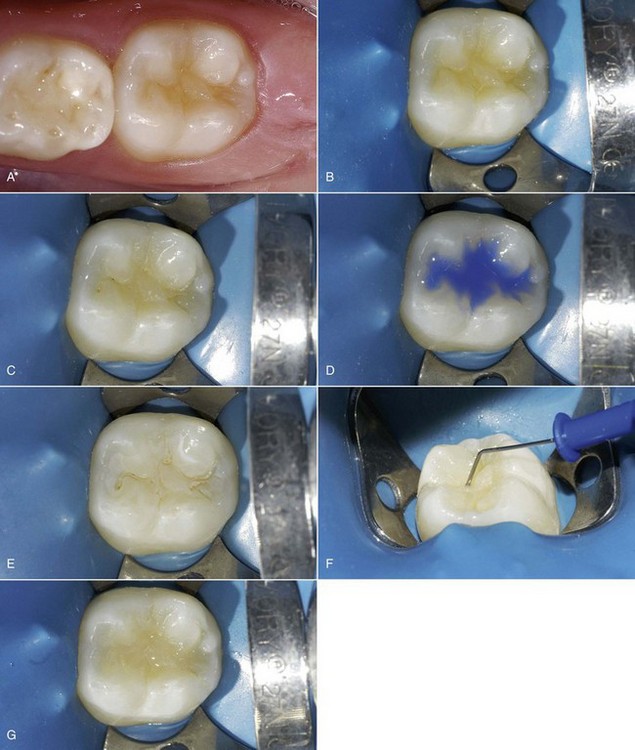
Today there is an increasing and decisive demand among patients for “invisible” restorations (Figures 9-6 and 9-7).
Longevity
These materials also have a satisfactory life (Figure 9-8). According to Skeeters and colleagues (1998), 95% of restorations retain their function after 15 years; for Kohler and colleagues (1998) the 5-year duration depends on proper selection of cases and caries susceptibility.
Hoby and colleagues (1998) argue that after 5 years of function, marginal adaptation in premolars with Class II cavities seems more comparable to that of similar cavities with amalgam fillings. According to van Dijken (2000) the survival rate of composite inlays applied with intraoral technique is 83% at 11 years. A major review of the literature on the clinical survival of direct and indirect restorations since 1990 (Manhart and colleagues, 2004) reports an average annual failure of 2.2% for direct composite restorations and 2.9% for composite inlays.
Suitable for All Types of Cavities
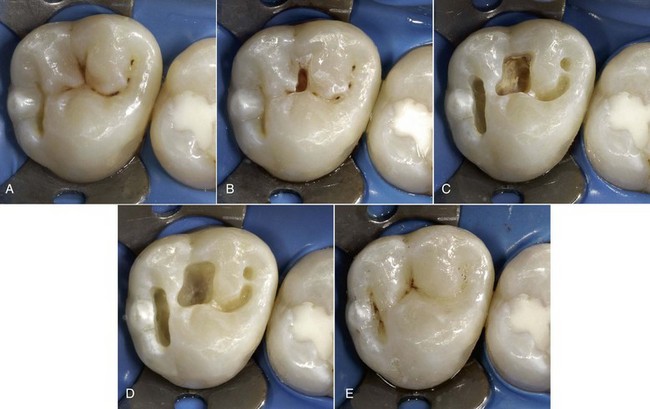
Composites can be used for preventive restorations, for small, medium, and large Class I and II restorations, and those that are gradually more complex, culminating with full cuspal coverage—all of which are performed with the same material applied with different techniques (direct, semidirect, indirect). Figure 9-9 exemplifies some of the benefits listed previously.
Direct Class I Restorations in the Posterior
Adhesive Cosmetic Restorations in the Posterior
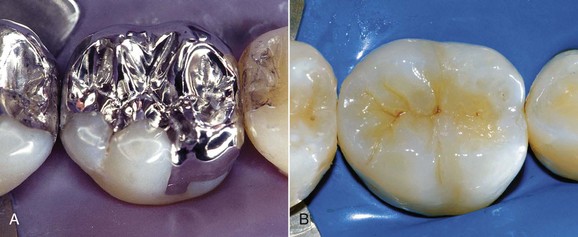
For many years metals used for both direct and indirect techniques were considered the only viable treatment option for restorations in the lateral sectors. Amalgam was the first choice for conservative dentistry for a long time, and today—despite the various alarmist campaigns regarding its potential toxicity—it continues to have important indications (Ferrari and Patroni, 2000).
Initially resins were used only in the anterior for both small and large restorations, with excellent results in terms of restoring shape, color, function, and esthetics (Figure 9-10).
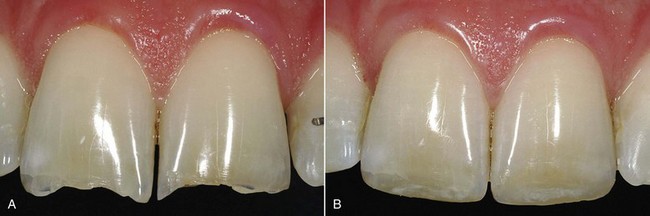
Figure 9-10 Example of a direct anterior adhesive composite restoration before (A) and after (B) treatment.
Today the latest evolution of enamel-dentin adhesive systems and composite materials has completely changed the therapeutic approach to carious lesions in the posterior, allowing greater preservation of sound dental tissues during preparation of the cavities (adhesive techniques do not require any drilling for mechanical retention) and also offering better reliability and esthetics (Figure 9-11).
Moreover, preventive extension gives way to the “prevention of extension” principle (Toffenetti, 2001).
Classification
Among the most reliable classifications, that of the Geneva School (Dietschi and Holz, 1990) divides posterior cosmetic restorations into three categories corresponding to three basic techniques: direct, semidirect (intraoral and extraoral), and indirect techniques.
Regarding the selection criteria of the three methods, the main decision parameters (Dietschi and Spreafico, 1997) rely especially on the following:
With greater thicknesses and heights (>1 mm) all three techniques can be used, and in such cases the choice is based mainly on the size of the cavity (see Figure 9-12).
Indications
Class II cavities instead involve the proximal surfaces of molars and premolars (Marmasse, 1980).
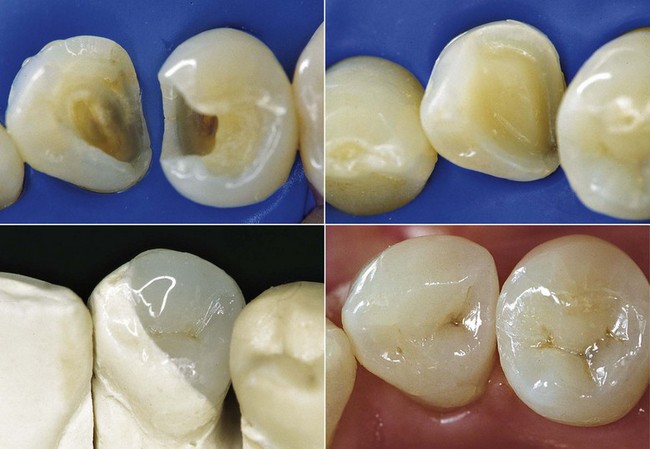
Composite is considered the material of choice for small-to-medium Class I cavities.
The approach is extremely conservative and strengthens the remaining tooth structure, which is not possible with metals (Eakle, 1986).
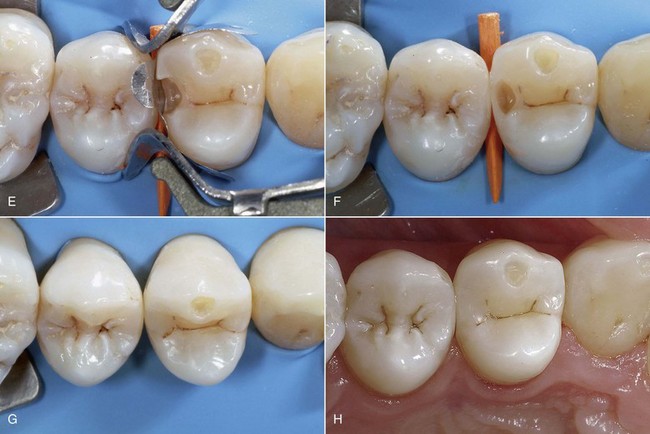
The method is relatively simple to perform and the esthetic outcome is predictable (Figure 9-13).
Cavity Preparation Techniques
Minimally Invasive Preparations
The main goal of modern restorative dentistry based on the minimally invasive approach thus lies in the ability to avoid or defer the performance of restoration (Peters and McLean, 2001a).
The application of these principles within clinical restorative techniques, considered secondary to disease control and caries prevention, has led to the development of increasingly sophisticated techniques and tools, including the following (Peters and McLean, 2001a):
Atraumatic Restorative Technique
ART (World Health Organization [WHO], 1994) is used only in special circumstances, particularly in countries with inadequate healthcare, when limited dental equipment is available (emergency home treatment), and in certain circumstances (e.g., the elderly, uncooperative patients). It can also be performed by nurses and auxiliary personnel. It involves control and stabilization of existing active carious lesions by partial removal of carious tissue with hand instruments. Self-hardening glass-ionomer cement is applied to create a sort of indirect pulp capping and promote remineralization of pathologic residual dentin.
The limits of the procedure are mainly related to the operational difficulties determined by the use of hand instruments (Van Amerongen, 1996).
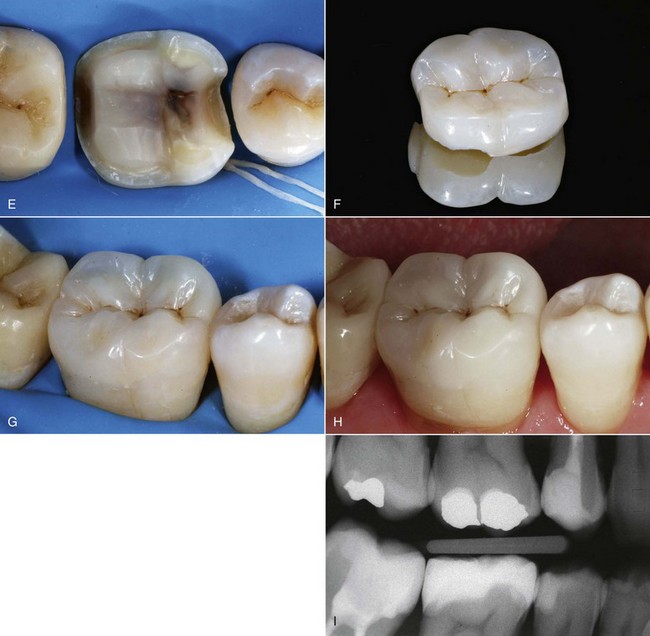
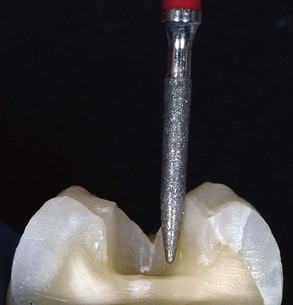
Traditional Rotary Instruments
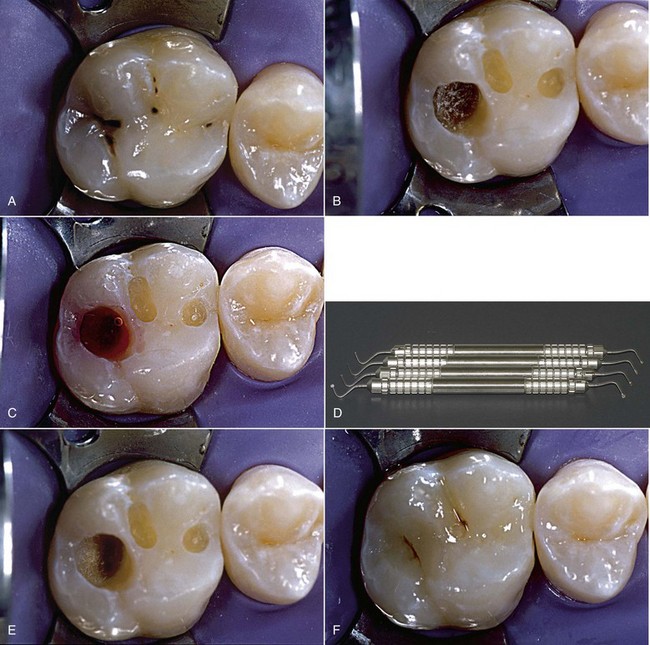
Traditional rotary instruments are unquestionably the most widely used tools in restorative dentistry, and today they can be combined with more up-to-date sonic systems and caries removal instruments based on chemical and mechanical systems (Figure 9-14).
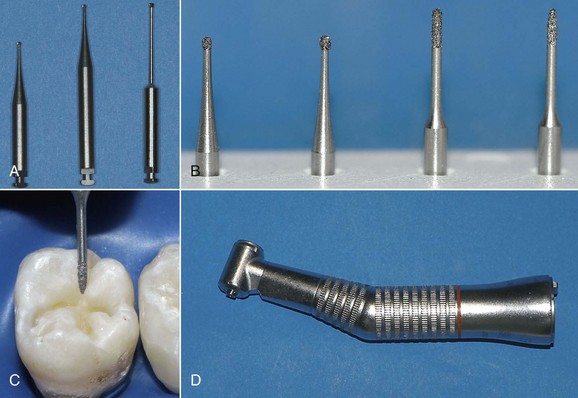
Sonic Instruments
Sonic instruments, on the other hand, are characterized by greater ease of use and safety for the adjacent teeth owing to their special shape with a smooth nonworking flat portion, which is set toward the marginal surface of the adjacent tooth, and a diamond convex working portion for cavity shaping (Figure 9-15).
According to some authors, a combination of rotary and ultrasound instruments ensures a more conservative approach (Krejci, Dietschi, and Lutz, 1998; Galimberti and colleagues, 2001; Sheets and Paquette, 2002).
Tunnel cavities are preparations that, starting from the marginal fossa, reach the interproximal carious area without completely removing the marginal ridge below which the carious process started. This is a more conservative approach. Closed tunnel cavities are preparations in which only the carious dentin is removed and the interproximal enamel wall is maintained. The preparation is referred to as an open tunnel when there is involvement and removal of the demineralized enamel (Pope and colleagues, 1993; Peters and McLean, 2001a).
Slot (or box) preparations can further be divided into vertical (occlusal) preparations (Figure 9-16) and horizontal (bucco-palatal) preparations (Figure 9-17).

Figure 9-16 Example of vertical slot preparation.
According to many authors, the tunnel has no advantages over the slot. Moreover, tunnel preparations are harder to perform, involve more difficulties in the removal of carious dentin because of the limited access, and have an increased risk of pulp involvement and fracture of the marginal ridge (Papa and colleagues, 1993; Peters and McLean, 2001a; Ericson and colleagues, 2003) (Figures 9-18 and 9-19).
Chemical-Mechanical Systems
This system is quite effective for removing carious dentin, has no adverse effects on pulp vitality or the composition of pulp and dentin, and does not interfere with adhesive processes. Moreover, there is less need for anesthesia (Ericson and colleagues, 1999; Bongenhielm and Young, 2001; Hossain and colleagues, 2003) (Figure 9-20).
Air Abrasion
The main advantages are the lack of vibration and noise and a reduced need for anesthesia.
In addition, the problems of dust and contamination of the environment should be taken into account (Rinaudo, Cochran, and Moore, 1997; White and Eakle, 2000; Malmstrom, Chaves, and Moss, 2003) (Figures 9-21 and 9-22).

Figure 9-21 Tips for air abrasion.
Laser Systems
Its mechanism of action is based on high-energy absorption and rapid evaporation of water molecules, generating microexplosions resulting in mechanical removal of the substrate (Hibst and Keller, 1989).
According to some authors, the effects determined by the use of the Er:YAG laser on the pulp are equivalent to those of a turbine handpiece (Cozean and colleagues, 1997).
The laser action increases the resistance of enamel and dentin to acid exposure, with adhesion values that are lower for irradiated dentin compared with untreated tissue (Kameyama and colleagues, 2000).
Cavity preparation is also slower compared with conventional rotary instruments.
In any case, laser surface conditioning cannot replace etching with orthophosphoric acid (Poggio and colleagues, 2000).
Ozone Therapy
Exposing carious dentin to ozone supposedly leads to a significant reduction of cariogenic bacteria in primary root caries (Baysan, Whiley, and Lynch, 2000).
Some authors are cautiously hopeful about these promising initial results, encouraging further investigation and confirmation by researchers (Ericson and colleagues, 2003).
Materials for Minimally Invasive Restorations
The selection criteria for these materials are based on the parameters listed in the box.
Instead, composites always require complete removal of demineralized dentin to obtain an optimal adhesive bond (Mount and Ngo, 2000; Mount, 2003).
Small cavities are often more difficult to layer owing to the absence of voids and porosity. It may be useful to apply flowable composites on the cavity floor, and they can be combined with the application of microhybrid composites with superior physical and mechanical properties on the surface of the cavity (Chuang and colleagues, 2001; Opdam, Roeters, and de Boer, 2003) (Figure 9-23).
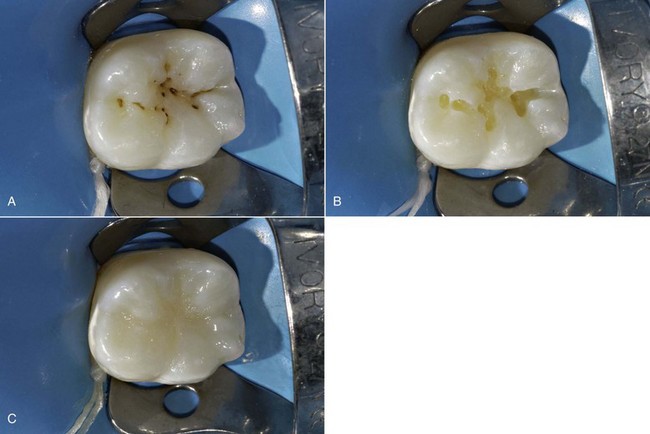
Operative Sequence for Preventive Resin Restorations
1. Careful isolation of the field with a rubber dam.
2. Cleaning with a brush and water jet and pumice or bicarbonate jet.
3. Thorough inspection and examination of the pit.
4. Possible selective opening of the pit if enamel lesion is suspected, using rose-head microburs at low speed or diamond needle burs at medium speed.
5. Etching and enamel-dentin bonding.
6. Execution of small restorations with bulk layering of a light-curing composite. PRRs are often combined with traditional sealings of the adjacent pits and fissures (Figure 9-26). According to some authors, traditional sealants (not filled) obtain better results in vivo in terms of microleakage than flowable composite and compomer. However, the ability of sealants to penetrate seems to be closely related to the shape of the groove (Duangthip and Lussi, 2003).
7. Application of a specific sealant or flowable composite on the intact pits and fissures.
8. Possible simultaneous curing of adhesive and sealant agents (Peters and McLean, 2001b).
Adhesive Preparation
Adhesive preparation (Lutz and colleagues, 1976; Porte and colleagues, 1984) applies to primary deep carious lesions whose extent is the sole determinant of cavity size. It entails rounding of the angles and definition of cavity margins through careful finishing (chamfering) of the enamel (Figure 9-27). In reality, chamfering of the occlusal portion simply means rounding the enamel to adjust the edges and improve the definition of cavity margins (Figure 9-28). A proper chamfer is not required, because, by virtue of their orientation at this level, the enamel prisms are already cut crosswise by the finishing bur (cylindric or a needle type) placed perpendicular to the occlusal surface (Schwartz, Summit, and Robbins, 1996).
Conventional Chamfer Preparation
Conventional chamfer preparation is used for cavities created by the replacement of metals. The general shape of the cavity is dictated by the preexisting restoration. After removal of any residual infected tissue, preparation requires adjustment of the internal angles by rounding and finishing of the margins, which will transform the cavity into an adhesive cavity (Figure 9-29).
Materials
These materials are highly filled (70% to 80% by weight, 60% by volume) and have excellent physical and mechanical properties, optimal surface characteristics (polishing), a modulus of elasticity similar to that of dentin, and wear behavior comparable to that of enamel and amalgam (10 to 50 microns/year) (Willems and colleagues, 1993).
Flowable composites are used in a thin layer to improve the fit between the adhesive and the composite and reduce the risk of postoperative sensitivity, especially in the most unfavorable cavity configuration. In this regard, it is certainly important to consider the cavity C-factor, described by Feilzer, De Gee, and Davidson (1987), which considers the relationship between cavity configuration and shrinkage stress based on the relationship between bonded and unbonded surfaces—in other words, the inversely proportional relationship between the number of cavity walls and preservation of adhesion (Davidson, De Gee, and Feilzer, 1984).
The application of more flexible materials in the deepest areas of these cavities, such as flowable composites, is desirable to compensate for stress and improve the fit between adhesive and composite (Dietschi and colleagues, 1995; Dietschi and Spreafico, 1998; Scheibenbogen-Fuchsbrunner and colleagues, 1999).
Layering
Bulk Technique
The bulk technique approach is used for small cavities (preventive cavities), where the thickness of the material is irrelevant in terms of polymerization shrinkage (see Figures 9-24 and 9-25).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses