Chapter 9 Anterior Direct Composites
Section A Direct Anterior Bonding: Minimally Invasive Dentistry at Its Best
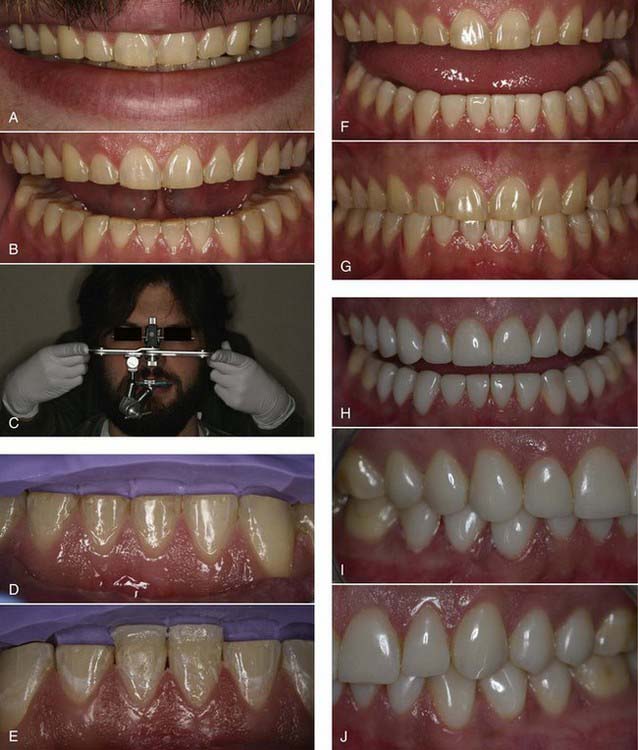
Modern resin materials have opened a huge door of opportunity for both dentists and patients by offering an esthetic and minimally invasive alternative for restoring the dentition that can be accomplished in just one office visit. Direct composite restorations make it possible to restore defects, repair tooth structure invisibly (Figures 9-1 to 9-3), and change tooth shape and alignment (Figures 9-4 and 9-5) without the use of a dental laboratory. This chapter section explores the influence of composites on modern dentistry and guides dentists through the art and science of restoring the anterior dentition with composites.
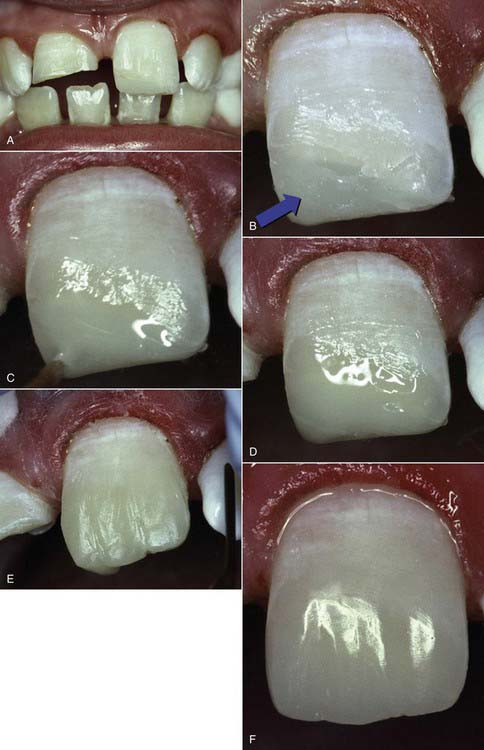
The best example for the value of a reliable opaquing system is when repairing a fractured incisor. Often clinicians try to replicate the dentin color and then overlay this layer with a compensating shade of enamel to achieve the right surface color. This involves considerable guesswork and offers inconsistent results. An alternate approach is to consider only the surface color. For example, if a fractured tooth is A1, then an A1 hybrid or nanofill can be added to recreate the incisal dentin portion of the tooth to help achieve opacity and strength. To eliminate translucent shine-through, an A1 opaquer can be placed over the top of the nanofill or microhybrid (Figure 9-6) to block and blend. Once the shine-through has been eliminated, there should be no difference between the tooth surface and the restoration. The addition of A1 microfill will create a perfect match of material to tooth structure and completely simulate the entire enamel surface once finished and polished. In this type of system, the colors of the opaquers, microhybrids, nanofills, and microfills should match one another and the corresponding shade guide exactly; only their values are different. (The Renamel Restorative System by Cosmedent [Chicago, Illinois] is the best example of this.)
Tints are yet another underutilized material that if used properly can greatly enhance the esthetics of anterior composite restorations. As with opaquers, lack of knowledge and lack of training in the application of tints is common. Tints are used to enhance incisal translucency as well as gingival hue and chroma. A good tint must be transparent to allow the light to shine through and carry the color into the overlying composite layer. Because of its translucency, microfill is the only composite material that truly allows this phenomenon of color shine-through to take place, creating the color realism from within (Figure 9-7). This is yet another reason for using microfill as the prime enamel layer.
Clinical Considerations
Composite Indications
Composite materials are indicated for almost all types of anterior restorations, from surface and incisal defects to routine restorations such as class III (Figure 9-8), class IV (Figure 9-9), and class V (Figure 9-10). They are ideally suited for other situations such as diastema closures, anterior veneering for color change, tooth reshaping, and tooth realignment to obtain a desired smile design (Figure 9-11). In addition, composites can be used for any type of treatment; such as full-bonded crowns (Figure 9-12), short-span anterior bridges, and porcelain repairs (Figure 9-13) which can all be constructed with direct composite resin. The indications for the use of anterior composite materials depend on how skilled the operator is, how comfortable the procedure feels, and how well the operator can develop the desired restoration. Although these restorations have the undeserved reputation of not holding up, when done properly they generally last at least 20 years (Figure 9-14).
Treatment Planning
Treatment planning is driven by the characteristics of each individual case. For patients who have no problems with their centric occlusion, centric relation or vertical dimension, treatment planning can be done in segments. Anterior restorations can be accomplished without restoring the posterior, but the practitioner should always remember to look at tooth size, inclination, rotation, or position and then visualize what needs to be done to create the illusion of perfection. For patients whose teeth are over-closed and those with decreased vertical dimension, it is necessary to treat the posterior occlusion first before addressing the anterior problems. Once the correct vertical dimension and centric occlusion have been established, then the proper anterior length and incisal guidance can be achieved with ease (Figure 9-15).
Sequence of Treatment
When planning a case, dentists must first look at the patient’s occlusion and all of the excursive and protrusive movements. If a person has either lateral or protrusive interferences, these must be addressed before tooth lengthening. For example, establishing proper canine rise with the use of composite is an excellent way to allow dentists the space necessary for tooth lengthening and proper disclusion (Figure 9-16). In wear cases, the patient’s mouth is treated according to the lip line. Often it is necessary to restore the cusp tips of the bicuspids and at least the first molar to achieve the ideal look and the uniform curve of Spee.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses






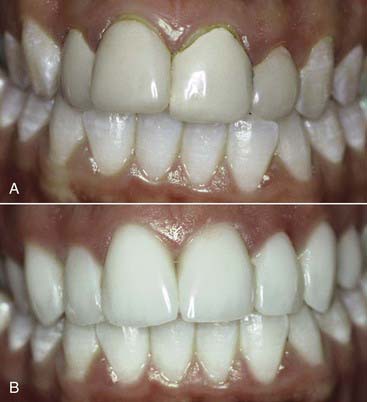


 years postperatively. They are virtually invisible when a Renamel Microhybrid with a Renamel Microfill overlay is used.
years postperatively. They are virtually invisible when a Renamel Microhybrid with a Renamel Microfill overlay is used.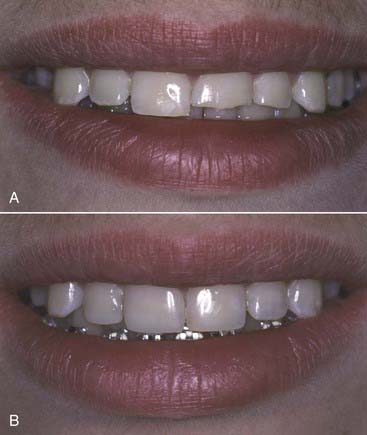



 years postoperatively. Note the diastema closure between the two centrals, the papillae completely intact after
years postoperatively. Note the diastema closure between the two centrals, the papillae completely intact after  years. No wear and no color change is seen due to the use of the microfill material.
years. No wear and no color change is seen due to the use of the microfill material.