8
Minimally Invasive Surgical Technique and Modified-MIST in Periodontal Regeneration
Pierpaolo Sandro Cortellini
Introduction
Periodontal regenerative technologies are applied to improve short- and long-term clinical outcomes of periodontally compromised teeth, presenting with deep pockets and reduced periodontal support. The persistence of deep pockets following active periodontal therapy has been associated with an increased probability of tooth loss in patients attending supportive periodontal care programs [1]. Teeth with deep pockets associated with deep intrabony defects are considered a clinical challenge: periodontal regeneration has been shown to be effective in the treatment of one-, two-, and three-wall intrabony defects or combinations thereof, from very deep to very shallow, from very wide to very narrow [2–5]. Therefore, the application of regenerative procedures, including minimally invasive procedures, is suited in deep and shallow intrabony defects.
Regeneration is a healing outcome that can occur when the systemic and local conditions are favorable. The systemic conditions include the control of periodontitis, a low total bacterial load in the mouth and cessation of smoking habits: high percentages of bleeding on probing and high bacterial loads as well as cigarette smoking have been associated with reduced clinical outcomes [6–12]. The local conditions include the presence of space for the formation of the blood clot at the interface between the flap and the root surface [12–17], the stability of the blood clot to maintain a continuity with the root surface avoiding formation of a long junctional epithelium [13,18–20], and the soft tissue protection to avoid bacterial contamination [10,21–23].
Development of periodontal regenerative medicine in the past 25 years has followed two distinctive, though totally interlaced paths. The interest of researchers has thus far focused on regenerative materials and products on the one side and on novel surgical approaches on the other side.
In the area of materials and products, three different regenerative concepts have been explored: (i) barrier membranes, (ii) grafts, and (iii) wound healing modifiers, plus many combinations of the aforementioned concepts [5].
In general, the development of surgical procedures was aimed at complete preservation of the soft tissues to achieve and maintain primary closure on top of the applied regenerative material/substance during the critical early stages of healing. Specifically, flap designs attempted to achieve passive primary closure of the flap combined with optimal wound stability.
In the 1990s, the modified papilla preservation technique (MPPT)[15] and the simplified papilla preservation flap (SPPF)[24] have been tested and proposed. These clinical innovations in flap design and handling have radically changed surgery and have allowed a drastic limitation of interdental wound failure to less than 30% of the treated cases. Further enhancements of clinical outcomes were achieved when an operative microscope was adopted [25,26]. Authors reported an increased capacity to manipulate the soft tissues that resulted in an improved potential for primary closure of the wound to an excellent 92% obtained with microsurgery. Other authors reported improved outcomes using operative microscopes in different areas of periodontal surgery, from flap surgery to mucogingival surgery [27–32].
In the past decade, a growing interest for more friendly, patient-oriented surgery have urged clinical investigators to focus their interest in the development of less invasive approaches [33–35]. Following this path, Cortellini and Tonetti proposed a minimally invasive surgical technique (MIST) on isolated [36] and multiple [37]intrabony defects, and a Modified MIST (M-MIST)[38] on isolated intrabony defects.
Clinical studies and outcomes
Cohort studies and randomized controlled clinical trials reporting outcomes on the application of minimally invasive surgical approaches are reported in Tables 8.1 and 8.2.
Table 8.1 Minimally invasive surgical technique (MIST): clinical studies.
| MIST | Type of study (quality of evidence) | Interventions | No. pax | No. defects | CAL gain | PD reduction | Δ REC |
| Cortellini and Tonetti [36] | Case cohort (level 2) | MIST + EMD | 13 | 13 | 4.8 ± 1.9 | 4.8 ± 1.8 | 0.1 ± 0.9 |
| Cortellini and Tonetti [39] | Case cohort (level 2) | MIST + EMD | 40 | 40 | 4.9 ± 1.7 | 5.2 ± 1.7 | 0.4 ± 0.7 |
| Cortellini et al. [37] | Case cohort (level 2) | MIST + EMD | 20 | 44 | 4.4 ± 1.4 | 4.6 ± 1.3 | 0.2 ± 0.6 |
| Ribeiro et al. [40] | RCT (Level 1) | MIST | 15 | 15 | 2.82 ± 1.19* | 3.55 ± 0.88* | 0.54 ± 0.58* |
| MIST + EMD | 14 | 14 | 3.02 ± 1.94* | 3.56 ± 2.07* | 0.46 ± 0.87* | ||
| Ribeiro et al. [41] | RCT (level 1) | MIST | 14 | 14 | 2.85 ± 1.19* | 3.51 ± 0.90* | 0.48 ± 0.51* |
| MINST (RPL) | 13 | 13 | 2.56 ± 1.12* | 3.13 ± 0.67* | 0.45 ± 0.46* |
MINST, minimally invasive non surgical technique (RPL with the aid of a microscope); MIST, minimally invasive surgical technique.
*No statistical difference.
Table 8.2 Modified-minimally invasive surgical technique (M-MIST): clinical studies.
| M-MIST/SFA | Type of study | Interventions | No. pax | No. defects | CAL gain | PD reduction | Δ REC |
| Cortellini and Tonetti [38] | Case cohort | M-MIST + EMD | 15 | 15 | 4.5 ± 1.4 | 4.6 ± 1.5 | 0.07 ± 0.3 |
| Cortellini and Tonetti [42] | RCT | M-MIST | 15 | 15 | 4.1 ± 1.4* | 4.4 ± 1.6* | 0.3 ± 0.6* |
| M-MIST + EMD | 15 | 15 | 4.1 ± 1.2* | 4.4 ± 1.2* | 0.3 ± 0.5 | ||
| M-MIST + EMD + BioOss | 15 | 15 | 3.7 ± 1.3* | 4.0 ± 1.3* | 0.3 ± 0.7* | ||
| Trombelli et al. [43] | RCT | SFA | 12 | 12 | 4.4 ± 1.5* | 5.3 ± 1.5* | 0.8 ± 0.8* |
| SFA + HA + GTR | 12 | 12 | 4.7 ± 2.5* | 5.3 ± 2.4* | 0.4 ± 1.4* | ||
| Mishra et al. [44] | RCT | M-MIST | 12 | 12 | 2.6 ± 0.8* | 3.8 ± 0.9* | 0.5 ± 0.5* |
| M-MIST + rhPDGF-BB | 12 | 12 | 3.0 ± 0.9* | 4.2 ± 0.6* | 0.8 ± 0.6* |
M-MIST, modified minimally invasive surgical technique; SFA, single flap approach; rhPDGF-BB, recombinant human platelet derived growth factor.
*No statistical difference.
Table 8.1 refers to MIST studies in which the interdental papillary tissues have been elevated to uncover the interdental space completely. This approach is supported by three cohort studies [36,37,39] and two controlled studies [40,41].
Table 8.2 reports studies in which the access to the defect was gained through the elevation of a small buccal flap, without elevation of the interdental papilla. This approach is supported by a cohort study [38] and three controlled studies [42–44]. Interestingly, the cited randomized clinical trials performed using minimally invasive surgical approaches (with or without papilla elevation) do not report any difference in terms of clinical outcomes between the minimally invasive control flap approach and the test in which a regenerative material/product was introduced under the flap. The reported outcomes raise a series of hypotheses that focus on the intrinsic healing potential of a wound when ideal conditions are provided with the surgical approach. In other words, the outcomes of these studies challenge clinicians with the possibility to obtain substantial clinical improvements without using products or materials applying surgical techniques that do enhance per se blood clot and wound stability. In particular, the advanced flap design of the M-MIST greatly enhances the potential to provide space and stability for regeneration by leaving the interdental papillary soft tissues attached to the root surface of the crest-associated tooth and by avoiding any palatal flap elevation. The interdental soft tissues are the stable “roof” of a room where the blood fills in and forms a clot. The hanging papilla prevents the collapse of the soft tissues, thereby maintaining space for regeneration. The anatomic bone deficiencies are potentially supplemented by the peculiar flap design that provides additional “soft tissue walls” to the missing bony walls improving stability: walls of the “room” are the residual bony walls, the root surface, and the buccal/lingual soft tissues. The minimal flap extension and elevation also minimizes the damages to the vascular system favoring the healing process of the tiny soft tissues.
Clinical indications and diagnostic procedures
Delivering periodontal surgery in general and regenerative treatment in particular requires knowledge, skills, experience, and a well-defined step-by-step approach.
The first step of periodontal therapy is always cause-related therapy, aimed at obtaining patient compliance, reduction of oral bacterial loads, and control of gingival infection.
At completion of nonsurgical cause-related therapy, patients have to be carefully reevaluated. A full periodontal evaluation should be performed to check for (Flow chart 8.1) the following aspects:
- The compliance of the patient in terms of plaque control: a very low load of bacterial plaque is a major goal of cause-related therapy and key to periodontal regeneration. Optimal regenerative outcomes have been reported in patients keeping full-mouth plaque score lower than 15% [5].
- The control of periodontal infection: low level of bleeding on probing is another major goal of cause-related therapy and is again extremely important for the regenerative approach. Optimal regenerative outcomes have been reported in patients having full-mouth bleeding score lower than 15% [5].
- The presence of residual pockets or furcations: after successful nonsurgical phase, most of baseline increased pocket probing depths should have been resolved or greatly reduced.
- Additional goals of cause-related therapy are control of behavioral and systemic conditions, such as smoking habits, stress, and systemic diseases (e.g., diabetes).
Chart 8.1
The presence of residual deep pocket probing depths might indicate the need for periodontal surgery. Surgical treatment of pockets can follow different paths from flap surgery, to resective surgery, to regenerative/reconstructive surgery. Clinical goals of regenerative surgery are to (i) reduce pocket probing depth through attachment gain while limiting the gingival recession and (ii) increase the functional support of the involved teeth. However, periodontal regeneration is not always applicable [5] (Flow chart 8.2). Ample evidence shows that it is highly predictable in the treatment of pockets associated with deep and shallow intrabony defects. Its applicability to furcations is questioned by the scientific community: good outcomes are reported only for the treatment of degree II furcations on lower molars. At present, there is no evidence supporting the application of periodontal regeneration to pockets associated with horizontal bone destruction.
Chart 8.2
Intrabony defects have been classified according to their morphology in terms of residual bony walls, width of the defect (or radiographic angle), and in terms of their topographic extension around the tooth [45]. Three-wall, two-wall, and one-wall defects have been defined on the basis of the number of residual alveolar bone walls. Frequently, intrabony defects present a complex anatomy consisting of a three-wall component in the most apical portion of the defect, and two- and/or one-wall components in the more superficial portions. Such defects are frequently referred to as combination defects. It is therefore mandatory to clearly diagnose the type of bone defect associated with the pocket. This assessment is based on periodontal probing. The presence of an interproximal intrabony defect is anticipated when there is a difference in the interproximal attachment level between two neighboring teeth. This difference represents the intrabony component of the defect: if the mesial surface of a tooth has an attachment level of 10 mm and the distal surface of the neighboring tooth has an attachment level of 4 mm, the depth of the intrabony component is 6 mm (Figure 8.1a–d). The diagnosis has to be confirmed with a periapical radiograph that provides relevant information about the morphology of both the defect and the root. However, in many instances, the radiograph underestimates the real depth of the defect.

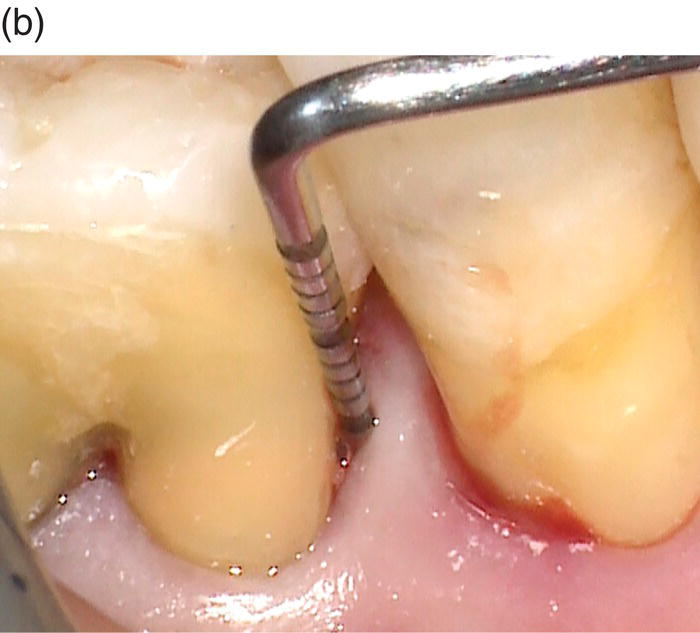
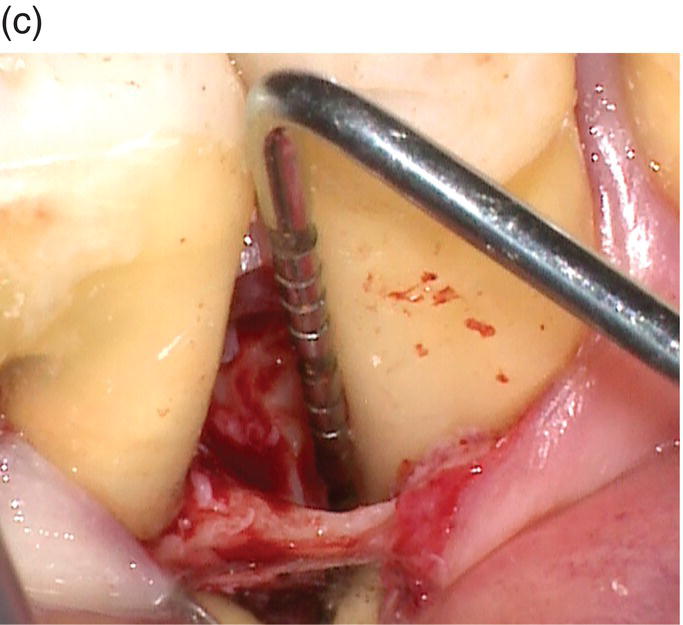
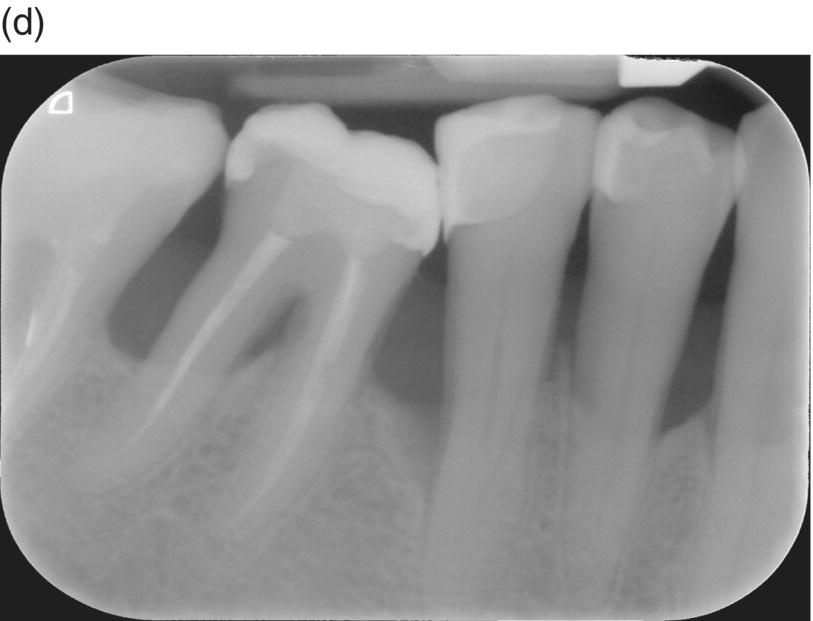
Figure 8.1 (a) The periodontal probe shows a 10 mm pocket on the distal side of the lower right second premolar. (b) A probing depth of 4 mm is detected at the mesial side of the lower right first molar. (c) The intrabony component of this three-wall defect is 6 mm. (d) Radiographic image of the intrabony defect.
When the presence of an intrabony defect is confirmed, the morphology and extension of the defect and/or the presence of additional defects at neighboring teeth should be carefully inspected. Bone sounding under local anesthetic is highly recommended as a very predictable diagnostic tool to get sound information on the extension of bone destruction.
This accurate diagnosis is necessary to select the type of surgical approach and the regenerative materials to be applied to the given clinical condition. In fact, different surgical approaches have been developed through time,which incorporate clear differences in terms of flap design and suturing technique. All the proposed surgical techniques have a common foundation in the attempt to fully preserve the defect-associated interdental papillae and all the buccal and lingual keratinized gingiva by applying intrasulcular incisions. The traditional papilla preservation flaps [15,24] are large and very mobile flaps that allow for ample accessibility and visibility of the defect area, for easy application of biomaterials and barriers, and for the coronal positioning of the buccal flap to cover barriers and biomaterials. The MIST [36], on the contrary, was designed to mobilize just the defect-associated papilla and to reduce flap extension as much as possible. The Modified-MIST [38], based on the elevation of a tiny buccal flap, further enhanced this concept by avoiding the interdental papilla as well as the palatal flap dissection and elevation.
The flow chart 8.3 indicates how to select the flap design according to the defect morphology and extension. Whenever a bone defect involves one or two sides of a root and is cleansable from a small buccal window, an M-MIST can be applied. If such a defect is not cleansable from the buccal window, the interdental papilla is elevated applying a MIST approach. A large papilla preservation flap (MPPT or SPPF), extended to the neighboring teeth and including also a periosteal incision and/or vertical releasing incisions, will be chosen in the presence of a very severe and deep defect, involving three or four sides of the root, requiring ample visibility for instrumentation and the placement of biomaterials and/or barriers.
Chart 8.3
Minimally invasive surgical technique
The MIST [36,39] is based on the elevation of the defect-associated interdental papilla along with minimally extended buccal and lingual flaps.
The entry incision is performed on the buccal side of the interdental papilla that is dissected with two different approaches according to the width of the interdental space. The width of the interdental space is measured with a periodontal probe as the distance between the two root surfaces; the periodontal probe is positioned horizontally about 2 mm apical to the tip of papilla. In some instances the interdental space is uneven on the buccal and on the lingual/palatal aspect: for example, frequently, the interdental space between the upper cuspid and the bicuspid is narrower on the palatal side than on the buccal one. In these instances, the measurement has to be taken on the palatal side.
In narrow interdental spaces (<2 mm), a buccal diagonal cut is selected, as described in the simplified papilla preservation flap (SPPF)[24]. This incision starts in the interdental sulcus of the defect-associated tooth: the microblade runs toward the contact point, strictly intrasulcular, then c/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


