8 Immune-Mediated, Autoimmune, and Granulomatous Conditions
Granulomatous Inflammation
True granulomas are collections of epithelioid histiocytes with variable inflammation and giant cells. Necrotizing granulomas are often seen in infectious processes and diseases of collagen degradation and necrobiosis. Table 8-1 lists the common granulomatous processes affecting the oral cavity; those caused by infections are discussed in Chapter 4.
| Granulomatous Inflammation | Distinguishing Features |
|---|---|
| Reactive | |
| Foreign body granuloma | Refractile or nonrefractile foreign material present; sometimes foreign material not identified |
| Intrinsic (e.g., ruptured hair follicle, cholesterol, keratin) | History of trauma or introduction of foreign material |
| Extrinsic | Dermal filler, amalgam |
| Infectious | |
| Bacterial infection (e.g., Bartonella henselae) | Warthin-Starry stain |
| Mycobacterial infection (often necrotizing) | Acid-fast bacillus or Fite stain |
| Spirochetal infection (e.g., tertiary syphilis gumma) | Warthin-Starry, Dieterle, or modified Steiner stain |
| Deep fungal infections | Methenamine silver or PAS stain; may see pseudoepitheliomatous hyperplasia |
| Others | |
| Sarcoidosis | Hilar lymphadenopathy, elevated ACE levels |
| Crohn disease | Gastrointestinal symptoms, positive endoscopic findings |
| Orofacial granulomatosis | Idopathic or related to Crohn disease |
| Wegener granulomatosis | Upper respiratory or renal findings, c-ANCA positive |
| Lichenoid granulomatous inflammation | Coexisting lichenoid stomatitis |
| Palisaded granulomas (e.g., rheumatoid nodule) | History of rheumatoid arthritis or necrobiotic disease |
ACE, Angiotensin converting enzyme; c-ANCA, cytoplasmic antineutrophil cytoplasmic antibodies; PAS, periodic acid–Schiff.
Foreign Body Granulomas
Etiopathogenesis and Histopathologic Features
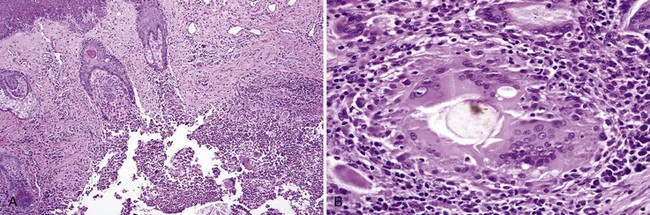
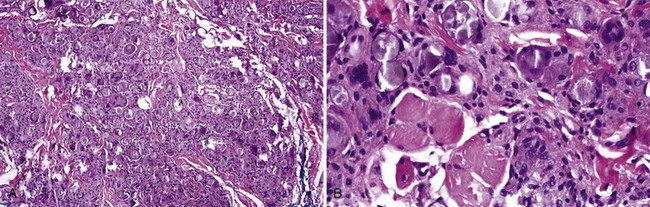
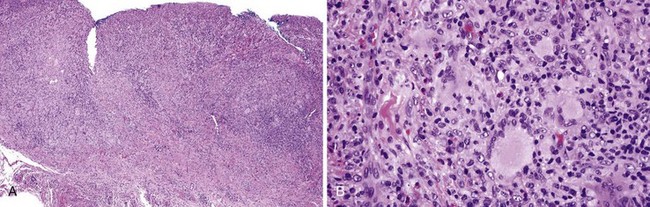
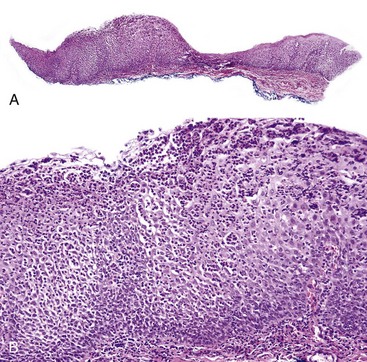
• Proliferation of epithelioid histiocytes and foreign body giant cells, nonnecrotizing; refractile or nonrefractile foreign material may be identified (Fig. 8-1).
• Poly-l-lactic acid fillers are refractile fusiform or geometric structures (Fig. 8-2).
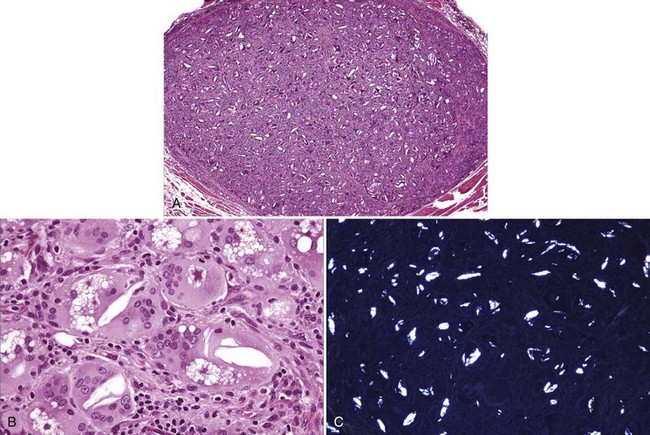
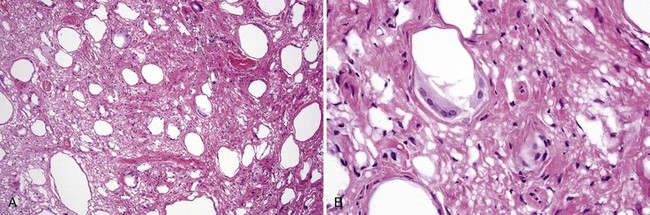
• Lipid and silicone granulomas have cytoplasmic vacuoles of varying sizes (Figs. 8-3 and 8-4).
• Calcium hydroxylapatite consists of gray-brown microspheres, 25 to 40 microns in diameter, that are nonrefractile; they stimulate endogenous collagen production and are resorbed within a few months, but they may cause a granulomatous response (Fig. 8-5).
• Foreign body granulomas are common in odontogenic cysts (see Chapter 14), around amalgam tattoos (see Chapter 9), and in keratinizing squamous cell carcinomas (see Chapter 11).
Differential Diagnosis
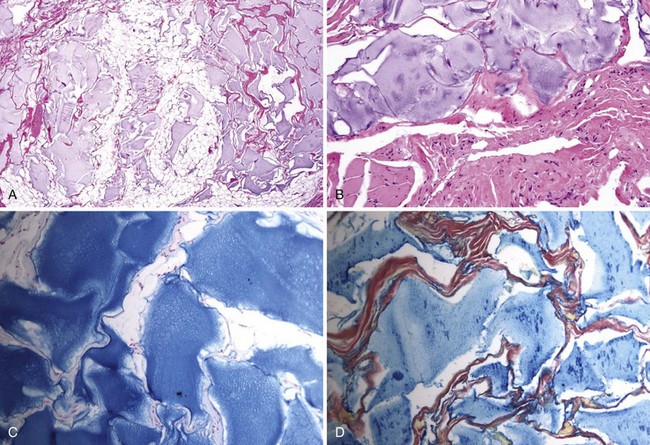
• Hyaluronic acid fillers appear as amorphous basophilic pools of ground substance that stains for alcian blue and colloidal iron; they do not incite a reaction (Fig. 8-6).
• Palisaded granulomas of necrobiosis lipoidica, granuloma annulare, and rheumatoid arthritis are rarely encountered intraorally.
Ficarra G, Mosqueda-Taylor A, Carlos R. Silicone granuloma of the facial tissues: a report of seven cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94:65-73.
Jham BC, Nikitakis NG, Scheper MA, et al. Granulomatous foreign-body reaction involving oral and perioral tissues after injection of biomaterials: a series of 7 cases and review of the literature. J Oral Maxillofac Surg. 2009;67:280-285.
Lombardi T, Samson J, Plantier F, et al. Oral granulomas after injection of cosmetic fillers. Histopathologic and clinical study of 11 cases. J Oral Path Med. 2004;33:115-120.
Narins RS, Coleman WP3rd, Glogau RG. Recommendations and treatment options for nodules and other filler complications. Dermatol Surg. 2009;35(suppl 2):1667-1671.
Requena L, Requena C, Christensen L, et al. Adverse reactions to injectable soft tissue fillers. J AM Acad Dermatol. 2011;64:1-34.
Sage RJ, Chaffins ML, Kouba DJ. Granulomatous foreign body reaction to hyaluronic acid: report of a case after melolabial fold augmentation and review of management. Dermatol Surg. 2009;35(suppl 2):1698-1700.
Skov BG. Rheumatoid nodule in the oral mucosa. J Oral Path Med. 1987;16:403-405.
Orofacial Granulomatosis and Crohn Disease
Orofacial granulomatosis may be idiopathic or the first sign of Crohn disease.
Clinical Features
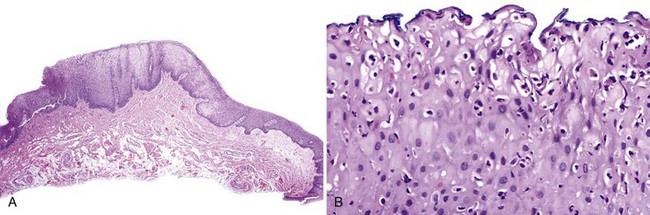
• Generally affects young adults; lips show diffuse or localized rubbery swelling that does not remit (unlike angioedema); tissues feel tight and sore (Fig. 8-7, A and B).
• May also show concomitant swelling of the gingiva; long-standing cases show cobblestoning and fissuring of mucosa from edema.
• Melkersson-Rosenthal syndrome, in addition to the lip swelling, exhibits fissured tongue and facial palsy; because fissured tongue is very common and facial palsy in this syndrome is very rare, it is unclear if this is a true syndrome.
• Crohn disease—in addition to the aforementioned features, there may also be papular folds of tissue in the maxillary and mandibular sulci, aphthous-like ulcers, gastrointestinal symptoms, and thickened and erythematous appearance of perivermilion skin (see Fig. 8-7, C); oral findings precede the diagnosis of intestinal disease in 50% of cases; some patients may also present with pyostomatitis vegetans (see later).
Etiopathogenesis and Histopathologic Features
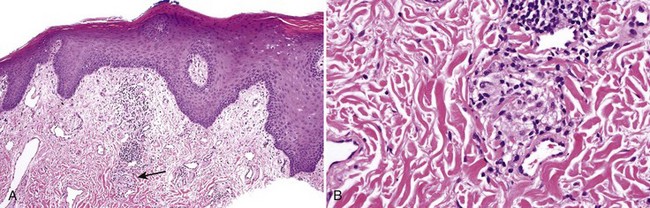
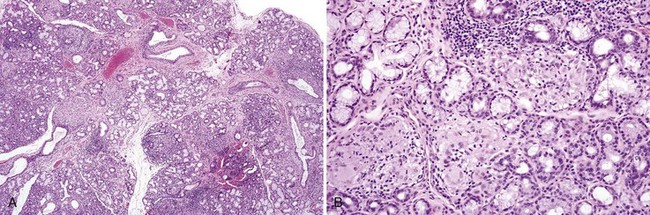
• Nonnecrotizing granulomas are noted and may be subtle in early disease (especially in idiopathic orofacial granulomatosis) (Fig. 8-8) or more florid in later disease; granulomas of Crohn disease may occur in salivary glands and may contain eosinophils (Figs. 8-9 and 8-10); multiple levels should be performed, if necessary, through the entire block to locate granulomas; edema and chronic inflammation alone are not sufficient for the diagnosis.
Differential Diagnosis
• Other granulomatous processes must be ruled out with histochemical stains.
• Granulomas of sarcoidosis are nonnecrotizing and well demarcated or “naked” (Fig. 8-11); patients are often blacks, have hilar lymphadenopathy, and elevated levels of angiotensin-converting enzyme; labial salivary gland biopsies show granulomas in 33% of cases.
Management and Prognosis
• Patch test for the idiopathic type to determine if hypersensitivity to the environment exists; intralesional steroid injections can be done every week for several weeks, but relapse is common; topical, intralesional, and systemic therapy controls disease in 70% of patients; minocycline or thalidomide helps some patients.
• Gastrointestinal work-up is indicated if there are intestinal symptoms.
Abraham C, Cho JH. Inflammatory bowel disease. N Engl J Med. 2009;361:2068-2078.
Al Johani KA, Moles DR, Hodgson TA, et al. Orofacial granulomatosis: clinical features and long-term outcome of therapy. J Am Acad Dermatol. 2010;62:611-620.
Dupuy A, Cosnes J, Revuz J, et al. Oral Crohn disease: clinical characteristics and long-term follow-up of 9 cases. Arch Dermatol. 1999;135:439-442.
Grave B, McCullough M, Wiesenfeld D. Orofacial granulomatosis—a 20-year review. Oral Dis. 2009;15:46-51.
Harty S, Fleming P, Rowland M, et al. A prospective study of the oral manifestations of Crohn’s disease. Clin Gastroenterol Hepatol. 2005;3:886-891.
Hegarty A, Hodgson T, Porter S. Thalidomide for the treatment of recalcitrant oral Crohn’s disease and orofacial granulomatosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:576-585.
Lourenco SV, Hussein TP, Bologna SB, et al. Oral manifestations of inflammatory bowel disease: a review based on the observation of six cases. J Eur Acad Dermatol Venereol. 2010;24:204-207.
Plauth M, Jenss H, Meyle J. Oral manifestations of Crohn’s disease. J Clin Gastroenterol. 1991;13:29-37.
Saalman R, Mattsson U, Jontell M. Orofacial granulomatosis in childhood—a clinical entity that may indicate Crohn’s disease as well as food allergy. Acta Paediatr. 2009;98:1162-1167.
Tabak L, Agirbas E, Yilmazbayhan D, et al. The value of labial biopsy in the differentiation of sarcoidosis from tuberculosis. Sarcoidosis Vasc Diffuse Lung Dis. 2001;18:191-195.
Tilakaratne WM, Freysdottir J, Fortune F. Orofacial granulomatosis: review on aetiology and pathogenesis. J Oral Pathol Med. 2008;37:191-195.
Pyostomatitis Vegetans
Clinical Findings
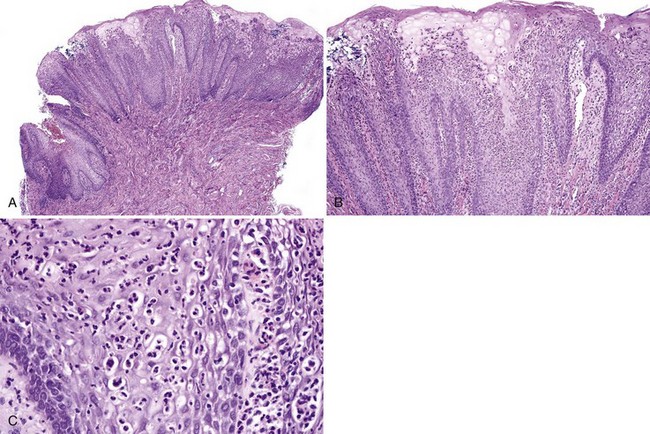
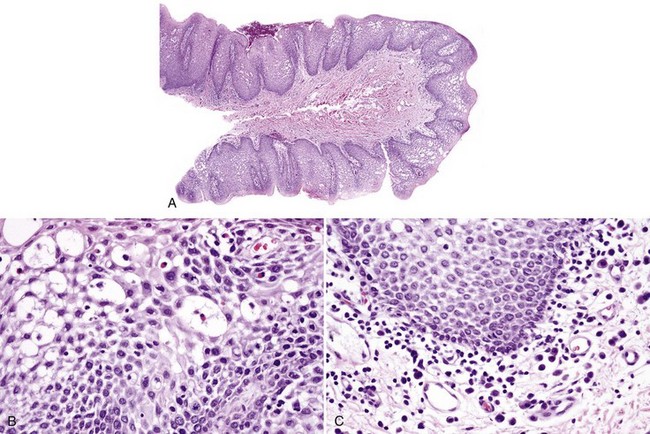
• Shallow ulcers and erosions, miliary abscesses and pustules on erythematous mucosa (Fig. 8-12); vegetations may be a feature; sometimes folding and fissuring of the buccal mucosa occurs.
• Most common associations are ulcerative colitis (approximately 70%), Crohn disease (10% to 15%) and liver disease; peripheral blood eosinophilia is present in 90% of cases; some cases are idiopathic.
Etiopathogenesis and Histologic Features
Pyostomatitis vegetans is the oral counterpart of pyoderma vegetans.
DeRossi SS, Salazar G, Sarin J, Alawi F. Chronic lesions of the gingiva and mucosa. J Am Dent Assoc. 2007;138:1589-1592.
Femiano F, Lanza A, Buonaiuto C, et al. Pyostomatitis vegetans: a review of the literature. Med Oral Patol Oral Cir Bucal. 2009;14:E114-117.
Gonzalez-Moles MA, Gil-Montoya JA, Ruiz-Avila I, et al. Pyostomatitis vegetans: dramatic clinical response to clobetasol propionate treatment in aqueous solution. J Eur Acad Dermatol Venereol. 2008;22:252-253.
Hegarty AM, Barrett AW, Scully C. Pyostomatitis vegetans. Clin Exp Dermatol. 2004;29:1-7.
Ko HC, Jung DS, Jwa SW, et al. Two cases of pyodermatitis-pyostomatitis vegetans. J Dermatol. 2009;36:293-297.
Markiewicz M, Suresh L, Margarone J3rd, et al. Pyostomatitis vegetans: a clinical marker of silent ulcerative colitis. J Oral Maxillofac Surg. 2007;65:346-348.
Immune-Mediated Conditions
Benign Migratory Glossitis (Migratory Stomatitis; Geographic Tongue, Erythema Areata Migrans)
Clinical Findings
• Occurs in 1% to 2% of population, usually in adults
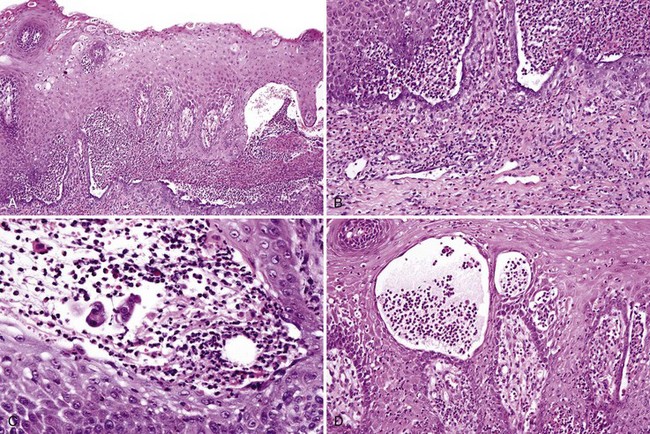
• Well-demarcated, patchy erythematous depapillation of tongue dorsum; raised, linear or circinate, often with discontinuous white peripheral rim; associated with fissured tongue in 25% of cases (Fig. 8-14, A and B); rare on sites other than the tongue (see Fig. 8-14, C)
Etiopathogenesis and Histopathologic Features
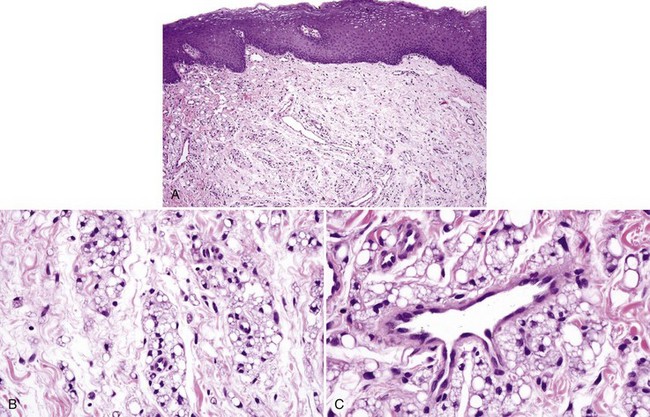
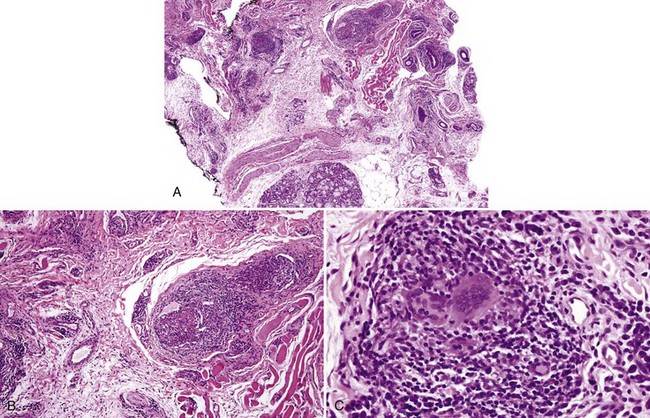
• Loss of filiform papillae; psoriasiform epithelial hyperplasia with spongiosis and spongiotic pustules (involving one third to two thirds of the thickness of the epithelium); variable lymphocytic infiltrate (Figs. 8-15 to 8-17)
Differential Diagnosis
• Candidiasis also shows psoriasiform epithelial hyperplasia and spongiotic pustules that are confined to the superficial two to three layers of keratinocytes; candidal hyphae are identified with periodic acid–Schiff stain.
• Spongiotic pustules at the edge of ulcers or in erosions involve the ulcer edge and the superficial keratinocytes.
Gonzaga HF. Both psoriasis and benign migratory glossitis are associated with HLA-Cw6. Br J Dermatol. 1996;135:368-370.
Goregen M, Melikoglu M, Miloglu O, Erdem T. Predisposition of allergy in patients with benign migratory glossitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:470-474.
Jainkittivong A, Langlais RP. Geographic tongue: clinical characteristics of 188 cases. J Contemp Dent Pract. 2005;6:123-135.
Zargari O. The prevalence and significance of fissured tongue and geographical tongue in psoriatic patients. Clin Exp Dermatol. 2006;31:192-195.
Nonspecific Hypersensitivity Reactions
Etiopathogenesis and Histopathologic Features
Contact hypersensivity reactions are probably within the spectrum of irritant contact stomatitis (see Chapter 7).
Ayangco L, Rogers RS3rd. Oral manifestations of erythema multiforme. Dermatol Clin. 2003;21:195-205.
Chrysomali E, Lozada-Nur F, Dekker NP, et al. Apoptosis in oral erythema multiforme. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:272-280.
Farthing P, Bagan JV, Scully C. Mucosal disease series. Number IV. Erythema multiform/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses