Chapter 8
Functionally Oriented Treatment Planning
Aim
The aim of this chapter is to describe the principles of the shortened dental arch concept.
Outcome
At the end of this chapter, the reader should be aware that it is not always necessary to replace all missing teeth. The decision to replace teeth should be based on whether prosthetic replacement will improve function, appearance and comfort. Limiting treatment goals to provide functional rather than a complete dentition is becoming acceptable in light of recent research findings.
Do We Need to Replace all Missing Teeth?
In many cases, patient and dentist opinion differs on what sort of dental treatment is required. This disparity between professionally assessed treatment need and patient demand is particularly apparent in older patients. When a patient presents with missing teeth, the clinician should consider the following:
-
Does the patient have any problems chewing food?
-
Does the patient have any appearance or cosmetic concerns arising from the missing teeth?
-
Does the patient have any discomfort arising from the missing teeth?
-
Is there any evidence of occlusal instability as a result of the missing teeth?
If the answer to any one of these questions is “yes”, then there is a good case to be made for replacing the missing teeth. If the answer to all of these questions is “no”, then replacing the missing teeth is not necessary. Population-based studies indicate that patients not sufficiently motivated to use RPDs decline to wear them. A common finding from these studies is that missing posterior teeth are not always considered a problem by patients. However, patients are often persuaded to seek replacement of teeth when anterior teeth are lost. They may feel compelled to wear an RPD to replace both anterior and posterior missing teeth when their primary concern is the anterior tooth space, and this may be a source of dissatisfaction.
A further consideration is the issue of biological price – does the potential benefit of providing a prosthesis outweigh the potential damage it may cause to the remainder of the natural dentition? RPDs are associated with high levels of dental caries and periodontal disease, particularly in patients who have inadequate oral hygiene measures. Conventional fixed bridgework may involve extensive tooth preparations that may damage the vitality of the retainer teeth.
Older adults often have differing functional needs to younger adults, and do not always require a fully intact dentition to have adequate oral function. As adults gradually lose teeth, they have the capability to adapt to the limitations this imposes. Patients who have adapted well to tooth loss are unlikely to seek treatment to replace missing teeth unless anterior teeth are lost. A further consideration is the ability of an older adult to undertake a long course of treatment. Frail patients or those with chronic debilitating illness may be unable to accept prolonged courses of treatment and more modest treatment goals should be established.
Influences on Tooth Replacement Decisions
The clinician must determine the following when considering treatment options to replace missing teeth:
-
Patient’s motivation – their previous dental history will give an indication of compliance.
-
Finance – how much is the patient willing to pay for dental treatment?
-
Ability to attend for treatment.
Possible treatment options for replacing missing teeth in partially dentate patients are shown in Fig 8-1. Highly motivated patients are likely to seek tooth replacement, and this is indicated when the patient has satisfactory plaque control procedures. They should also be willing to attend for numerous appointments and be able to finance complex treatment. Some patients may not be able to afford expensive treatment, or be willing to attend for numerous visits for dental treatment. Modest treatment goals should be established for these patients and this may involve limitation of treatment goals to provide a functional rather than a complete dentition.
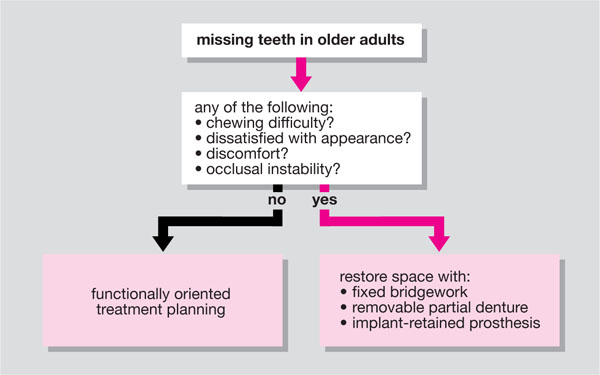
Fig 8-1 Possible treatment options for the replacement of missing teeth in older adults.
The Shortened Dental Arch Concept
Rationale
Many epidemiological studies have indicated that older adults do not always seek treatment to replace missing posterior teeth. Further researchers have suggested that older patients have differing functional needs to younger adults and may not need treatment to replace all missing teeth. A final consideration is that financial resources for dental treatment are diminishing, and dentists will increasingly have to think strategically about long-term treatment goals. Kayser and co-workers proposed the shortened dental arch (SDA) concept as a means of limiting treatment goals to provide a functional rather than a complete dentition. This concept is underpinned by directing treatment resources at preserving the anterior and premolar teeth. They identified these teeth as strategic teeth, or teeth considered important to the patient. Posterior teeth are replaced if they are likely to improve function, comfort or aesthetics.
Indications/contraindications to shortened dental arches
The indications for SDA are:
-
Caries and periodontal disease mainly confined to the posterior teeth.
-
There is a favourable prognosis for the anterior and premolar teeth.
-
Limited financial resources for dental care.
These criteria are rather broad, but essentially mean that there must be a good prognosis for the anterior and premolar teeth if this treatment strategy is going to work. This is intended to be a lifelong strategy and not a short-term stopgap./>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


