Chapter 8
Dental surgery design, disinfection and managing aerosols
Environmental hygiene is an important component of good infection control and an essential component of standard precautions. Overall, the practice environment should be clean, dry, well lit and well ventilated. This provides not only a pleasant environment to work but also one which increases patient confidence that the practice is a safe and professional surgery to visit.
DENTAL SURGERY DESIGN
Room size
Room should be of sufficient size to allow ready access to dental chair and to perform procedure unhindered (typical size: 17 m2). The surgery should allow unimpeded access for operators and patients, and have a design which facilitates environmental cleaning, access for disabled and access in case of a medical emergency. (For surgery designs, visit Department of Health Estates and Facilities Directorate (formerly NHS Estates) hosted by the Department of Health website at www.dh.gov.uk.)
Ventilation
Room should be well ventilated (open window) or air conditioned.
- Recommended fresh air supply rate should not be <5–8 L/second per occupant
- Air-cooled air conditioning is preferred; filters should be replaced regularly
- Ventilation systems should exhaust to the outside of the building
- Avoid free-standing or desktop mechanical fans if possible as they circulate dust, splatter and aerosols around the surgery
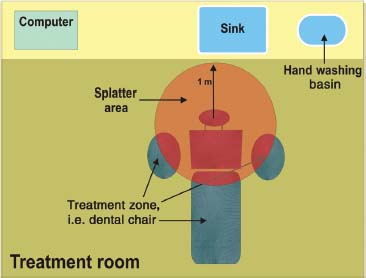
Figure 8.1 Diagram of zones within the dental surgery where contamination is likely to occur.
Work surfaces and zoning
- Areas within clean and dirty ‘zones’ for practice should be clearly identified to reduce the risk of cross-contamination (Figure 8.1)
- The room should be uncluttered to allow easy access for cleaning
- Work surfaces should be easy to clean, joint free and impermeable, and wherever possible curve up at the wall to avoid sharp, difficult-to-clean corners
Flooring
- Floors should be non-slip and wherever possible curve up the wall by at least 3 inches (to allow effective routine cleaning and cleaning of blood/body fluid spillages)
- The floor should be cleaned daily with detergent and warm water
- Carpets are not appropriate as they are harder to keep clean and cannot be reliably disinfected. Bacteria and fungi have been found growing in carpet in surgeries
Dental chair
Dental chair should be impermeable, intact and easy to wipe down. Good chair design with smooth seamless joins in the covering and control panels facilitates rapid cleaning and avoids build-up of microbial contamination.
Lighting
- Lighting should be of a suitable construction that allows easy cleaning and does not allow a build-up of dust
- Lighting used for patient examination must be fitted with a heat filter
- Handles should be covered with disposable plastic cover which is replaced between patients
Fixtures and fittings
- Fixtures and fittings should be clean, and coverings intact and in a good state of repair
- Upholstered furniture should be wipeable. Cloth-upholstered furnishings unless they are specially coated are harder to keep clean and cannot be reliably disinfected
Washbasins and hand hygiene
- An easily accessible hand washbasin should be available in the room, preferably with elbow-operated mixer taps. It should be specifically dedicated for hand washing and not used for cleaning instruments
- Hand washing sinks should not be fitted with plugs or overflows and the water jet must not flow directly into the plughole
- Wall-mounted (so can be elbow-operated) antimicrobial hand wash solution and non-medicated soap solution (with pump applicator) should be used. Antimicrobial solutions and soaps can become contaminated with microbes and support their growth. Do not top up half-empty containers. Either completely empty, clean and dry containers before refilling or use disposable containers
- Wall-mounted alcohol hand rub/gel should be available for hand decontamination for use on clean hands between patients
- Wall-mounted absorbent disposable paper towels should be provided
Clinical waste
A foot-operated clinical waste sack holder should be conveniently located in the room (see Chapter 10 on clinical waste management).
Sharps containers
An approved sharps container correctly assembled should be located within easy reach of the clinician, but out of the reach of unauthorised persons and children.
Storage of equipment and chemicals
- There should be adequate storage to enable the room to remain uncluttered and ensure that work surfaces are readily accessible and easy to clean
- Lockable cupboard(s) should be available to store medicines/disinfectants/chemicals in accordance with COSHH (1999) regulations
- Sterile stock should be stored on shelving in a secure, cool, dry and clean environment in order to maintain the integrity of the sterile product and its packaging
- Shelving should be readily cleanable and allow for free movement of air around the stored product
Protective clothing
Protective clothing should be readily available in the room, including disposable latex gloves and latex-free alternatives (sterile and non-sterile), disposable plastic aprons, masks and protective eyewear (goggles and visors).
Personal belongings should be kept in a separate room.
SURFACE CLEANING AND DECONTAMINATION
General cleaning
- The practice should have a nominated person to oversee that cleaning standards are maintained. A written protocol may be useful to ensure that standards are maintained
- All areas should be cleaned and damp dusted regularly. Detergent and hot water are adequate for most routine cleaning requirements. The dental clinical area should be cleaned and damp dusted daily
- Equipment such as mops, buckets and cloths should be specifically designated for the area of use and stored clean and dry. Mops should be washed regularly and stored inverted after use
Surface cleaning
The area around the dental unit becomes contaminated by direct splatter, by droplet nuclei and by touching surfaces with gloved hands. Surface cleaning prevents transmission of infection by direct contact with hands and equipment. (Note: Hand hygiene also prevents transmission of surface contaminants.) Dental chair, dental handpiece unit, 3-in-1 syringe handle and hoses, lights, bracket table and cabinets, all will require surface cleaning and disinfection. Try to avoid touching and thereby contaminating drawer handles, pens, computer keyboards and door handles with gloved hands. Pens are a well-recognised vehicle for transmission of MRSA.
Areas within the ‘dirty zone’, dental chair, dental handpiece unit, lights, bracket table and cabinetry, all will require surface cleaning and disinfection (Table 8.1).
You will need to check with the manufacturer whether the equipment can be cleaned with a detergent and/or disinfected. Commonly used surgery disinfectants are veridical and low residue, such as isopropyl alcohol spray or diluted hypochlorite solution (see Table 12.3 in Appendix).
Table 8.1 Areas requiring decontamination between patients
| Dirty zones: |
|
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


