Adhesive Cementation
When Should Adhesive Cementation Be Used?
What Are the Properties of Adhesive Cements?
Which Materials Can Be Adhesively Luted?
How Should Different Materials Be Conditioned for Adhesive Cementation?
How Should Dental Tissues Be Conditioned for Adhesive Cementation?
How Important Is the Thickness of the Cement?
Indications and Clinical Procedures for Indirect Restorations of Adhesively Luted Front Teeth
In the dental field, adhesion is undoubtedly one of most widely used terms of the last decade.
Daily practice has changed with the use of adhesive techniques and composites, which are used not only for direct restorations in the anterior and posterior but also for indirect restorations and prosthetic dentistry, owing to improvements in luting materials (Figures 8-1 to 8-4).
What is Adhesive Cementation?
This chapter will not discuss glass-ionomer cements, given their unsatisfactory adhesion compared with resin cements (Rosenstiel, Land, and Crispin, 1998) and the fact that this type of material is used in dentistry for traditional cementation in lieu of the most widespread and traditional techniques employing zinc oxyphosphate cement. The chapter will instead focus on cementations with resin products and conditioning systems for adhesive substrates, which are also resin based.
Another key distinction must be made regarding resin cements, depending on the type of activation of the polymerization reaction. In fact, there are self-curing cements, and their setting reaction depends on the mixing of a base and an accelerator; light-curing cements (Figures 8-5 to 8-7), which are not mixed with an activator but whose base paste contains photoactivators that can react to light stimulation at a particular wavelength; and dual cements, which have both light-curing and self-curing characteristics.
When Should Adhesive Cementation Be Used?
Materials that have good color characteristics but poor response to mechanical and physical stress (such as feldspathic and die-cast ceramics) require very strong cementation—in terms of adhesive bonding—to restore the crown stiffness lost after partial or total removal of the enamel of the natural tooth and thus attain acceptable mechanical features. Therefore in these cases it is essential to choose an adhesive protocol with resin cement and conditioning of the prepared tooth and the inner surface of the restoration (Figure 8-8).
What are The Properties of Adhesive Cements?
The ideal properties of cements are analyzed according to different aspects (Massironi and Ferraris, 2004): mechanical and physical, biologic, functional, and esthetic.
Mechanical and Physical Properties
Biologic Properties
Caries Resistance and Low Solubility
Secondary carious lesions at the tooth-restoration interface are among the most common causes of failure (Karlsson, 1986; Glantz and colleagues, 1993). In order to avoid this occurrence it is essential that the cement be unable to dissolve in the oral environment, especially at the prosthetic margin where this would leave room for bacterial contamination and the possible onset of carious lesions. Moreover, the ability to release substances that can remineralize dental hard tissues, such as fluoride, is an excellent way to confer caries-resistant properties to adhesive cements. In addition to materials such as glass-ionomer cements, which release fluoride naturally (Wilson, Groffman, and Kuhn, 1985), this property has also been added to certain resin cements.
Handling Properties
Adequate Setting Time
It is important that cements have an adequate working time to allow handling before placement in the oral cavity for bonding. Manual mixing requires a minimum time that varies depending on the material, but, given the many variables involved with manual procedures, it is generally preferable to use mechanical mixing with applicators that contain premeasured amounts of material and provide proper and predictable mixing. Mechanical mixing also seems to optimize the characteristics of the material (Kern, Schaller, and Strub, 1993).
Esthetic Properties
Color Stability
The luting material may undergo color changes owing to curing and aging. In the case of a translucent restoration made of glass-ceramic or composite resin, this can affect the result to some extent. Therefore the material must have excellent color stability (Asmussen, 1983; Berrong, Weed, and Schwartez, 1993; Imaz and colleagues, 1995).
Which Materials Can Be Adhesively Luted?
The fact remains that adhesive luting is often synonymous with low solubility in oral fluids because of the characteristics of the resin cements used for this type of cementation. Therefore trends in the market and among dentists could go toward employing adhesive cementation to achieve a better prognosis, even in cases of less retentive abutments and especially to prevent secondary caries. Indeed, the latter continues to be the most frequent cause of failure in fixed prosthetic dentistry (Karlsson, 1986; Glantz and colleagues, 1993), essentially because of inaccurate margins of the restoration and excessive dissolution of the cement in contact with oral fluids.
In order to further prevent the possibility of secondary caries, certain resin luting materials provide a gradual release of fluoride (Rosenstiel, Land, and Crispin, 1998), although according to some studies (Wiegand, Buchalla, and Attin, 2007) there is no apparent direct correlation between fluoride release and the significant reduction of secondary caries.
How Should Different Materials Be Conditioned for Adhesive Cementation?
Metals
Noble and non-noble alloys have a wide variety of adhesion values to different types of cement, including resin-based ones (Aboush and Yenkins, 1989; Atta, Smith, and Brown, 1990; Fayyad, 1990; Kohli and colleagues, 1990; Cotert and Ozturk, 1996). The final adhesion is micromechanical, and it usually requires some type of surface treatment to increase the adhesive bond.
Noble alloys have lower adhesive ability than other materials such as base-metal alloys (Sen, Nayir, and Pamuk, 2000). Nevertheless, for many types of restoration this is not an absolute limitation to their clinical use. For example, metal-ceramic crowns can carry an excellent prognosis with nonadhesive cementation, because retention is mainly ensured by the shape of the prosthetic abutment regardless of the type of definitive cement that is used. Moreover, by having a rigid substrate below the ceramic coating, this type of restoration does not need to adhere strongly to the substrate to improve the response to mechanical and physical stress.
It is believed that one of the most effective systems for metal conditioning entails the use of a promoter solution (usually fluid) before application of a resin cement (Turner and Sinclair, 1990; Nabadalung, Powers, and Connelly, 1998) such as phosphate monomer–based materials.
Another very effective treatment for obtaining adhesion with a resin adhesive system on metal dental materials is tribochemical silicatization (which will be described in the section on composite and crystalline ceramic bonding) and subsequent treatment with a silane (Matinlinna and Vallittu, 2007).
Likewise, metal can be conditioned with macroretentions and specific primers for metal alloys, thus allowing better adhesion between the metal and coating material, especially with composite resins (Figure 8-9). In recent years composite-metal prostheses won the favor of many clinicians, and the improved adhesion between these two materials may have contributed to the growing use of this technique.
Composite Materials
The aspect of indirect restorations that is most prone to problems—even in the case of cementation of composite restorations—is cements exposed to the oral environment (Kawai, Isenberg, and Leinfelder, 1994; Shinkai and colleagues, 1995). Nevertheless, the low water solubility of resin cements (Rosenstiel, Land, and Crispin, 1998) contributes to a good prognosis.
There are factors that can benefit indirect ceramic restorations, such as improved reproduction of the stiffness of natural tooth enamel (Magne and Douglas, 1999a, 1999b, and 2000) and certain color characteristics, even if the esthetic performance of modern composites has improved markedly in recent years.
With respect to older composite materials, modern ones offer better wear resistance (Ferracane and Condon, 1992; Park, 1996), physical properties (Uçta li, Wilson, and Zaimo lu, 1993; Reinhardt, Boyer, and Stephens, 1994), and color stability (Wendt and Leinfelder, 1992; Donly and colleagues, 1999). Indirect composite restorations can be placed even in the anterior with excellent results.
Various studies have investigated the possible treatment of composite surfaces for best adhesion (Swift and colleagues, 1992; Stokes, Tay, and Pereira, 1993; Hummel and colleagues, 1997) and good durability. Several treatments can be performed before application of an adhesive bonding agent: slight surface roughening with a bur, the application of hydrofluoric acid, the application of orthophosphoric acid, and blasting with aluminum oxide or silica-coated aluminum oxide (silicatization). In addition to these treatments, a silanizing agent commonly known as silane can also be applied. Silane is effective when the substrate surface contains silica particles, which composites contain naturally.
Recent studies have shown that orthophosphoric acid etching is not effective in increasing the adhesion between two composite surfaces (Valandro and colleagues, 2007), although dentists sometimes use this treatment to clean the surface further after conditioning. In reality, the latter aspect requires further scientific investigation.
Some studies show that silicatization (a chemical tribologic silica-coating process) and subsequent silanizations confer higher adhesion values compared with other treatments (Ozcan and colleagues, 2007).
Other authors believe that sandblasting and the subsequent application of silane are the most effective treatments, although, of the two treatments, blasting with 50-micron aluminum oxide can be considered more important than silane treatment for the purpose of better adhesion (D’Arcangelo and Vanini, 2007). The same study notes that hydrofluoric acid and silane on the composite do not significantly increase adhesion.
In conclusion, adhesion attained with sandblasting performed both with 30-micron silica-coated (silicatization) alumina particles and 50-micron alumina particles exhibits similar and very high adhesion values, followed in both cases by application of silane (Valandro and colleagues, 2007).
Therefore one of the most effective protocols is the following:
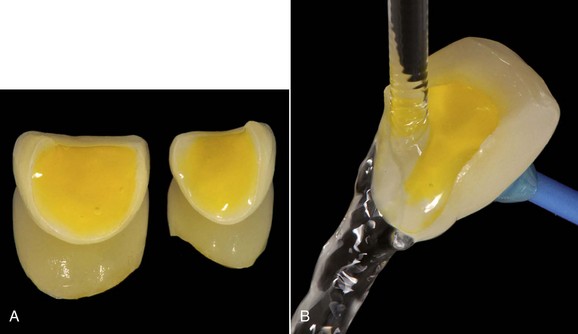
• Sandblasting of the inner surface of the restoration with aluminum oxide for about 10 seconds (Figure 8-10)
• Silanization (if necessary with activation by a hot air jet or in special ovens for silane drying)
• Drying after about 30 seconds
• Application of a layer of resin bonding agent and luting with a dual-cure resin or a light-curing restoration composite (which is usually heated first in a special oven) inside the restoration or on the dental preparation
Glass Ceramics
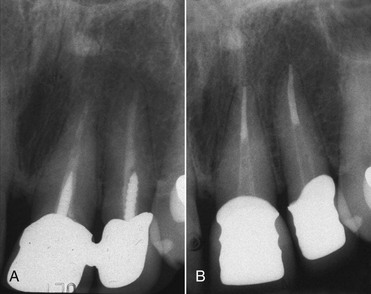
This type of ceramic can be feldspathic, commonly used as a coating in metal-ceramic prostheses (Weinstein, Katz, and Weinstein, 1962) (see Figures 8-1 and 8-2, A) or as a coating for metal-free restorations with a core with high mechanical resistance (Andersson and Oden, 1993). Other glass ceramics are die-cast, such as materials containing lithium silicate, which respond better than feldspathic ceramics to mechanical and physical stress (Raigrodski, 2004).
Because of their high translucency and esthetic characteristics, glass ceramics are ideal materials for porcelain veneers (McLaughlin, 1998), and they are also indicated for partial restoration in the posterior, such as ceramic inlays (Blatz, 2002).
In any event, it should also be considered that, if not properly supported by a rigid structure, all glass ceramics unfortunately offer limited performance when they are subjected to masticatory loads—for example, flexural strength and mechanical stress in general (Raigrodski, 2004). However, when final cementation is performed according to the appropriate procedures for adhesive bonding with composite material, this can increase the resistance to fracture of the ceramic restoration (Jensen, Sheth, and Tolliver, 1989) and the tooth-restoration complex, which can regain the crown stiffness lost when the natural enamel was removed (Magne and Douglas, 1999a, 1999b, 2000).
Good surface roughness and a clean surface are essential conditions in order to give the resin interdigitation and ensure a good chemical bond to the ceramic surface (Semmelmann and Kulp, 1968; Jochen and Caputo, 1977; Ferrando and colleagues, 1983; Sorensen and colleagues, 1991; Bailey and Bennett, 1992; Chen, Matsumura, and Atsuta, 1998a, 1998b). The type of surface conditioning may vary: surface roughening (Semmelmann and Kulp, 1968), preparation of ceramics with rotary instruments to create a rough surface (Semmelmann and Kulp, 1968; Jochen and Caputo, 1977; Ferrando and colleagues, 1983), acid etching of the surface (Bailey and Bennett, 1992), and sandblasting (Calamia, 1985; Lacy and colleagues, 1988). More than one treatment can be performed on the same artifact, and they can be combined in an attempt to achieve even better results in terms of adhesion. The application of hydrofluoric acid is an effective way to create a suitable surface before the application of various adhesive conditioning agents, increase the roughness of the ceramic material, and attain micromechanical retention between adhesive and substrate.
The application of 2.5% to 10% hydrofluoric acid on the surface for about 2 to 3 minutes seems to be the most effective way to roughen the surface of glass ceramics and prepare it for a strong adhesive bond (Sorensen and colleagues, 1991; Chen, Matsumura, and Atsuta, 1998a, 1998b) (Figure 8-11, A). After acid etching the etching gel should always be rinsed completely with water (Figure 8-11, B). The residue of ceramic salts derived from hydrofluoric acid conditioning can be noted on the surface of the restoration and must be removed, because these salts can adversely affect adhesion. Etching with orthophosphoric acid or solvents such as acetone or alcohol can be used for this purpose. Usually the next step is immersion in pure, clear alcohol in an ultrasonic cleaner for a few minutes (2 to 4 minutes).
Another type of conditioning is blasting with aluminum oxide particles (average grain particle 50 microns). However, according to several studies that examined repair after chipping, this treatment has not proven to be as effective when used alone without etching (Lacy and colleagues, 1988). Thorough sandblasting of the ceramic surface can often lead to an excessive loss of material and cause fractures (Calamia, 1985; Kern and Thompson, 1994). Therefore sandblasting is not advisable for metal-free restorations consisting of a fragile material with a low resistance to fracture, such as glass ceramic. A study (Kato, Matsumura, and Atsuta, 2000) that compared sandblasting with different types of etching concluded that hydrofluoric acid provided the best and most durable results in terms of adhesive bonding.
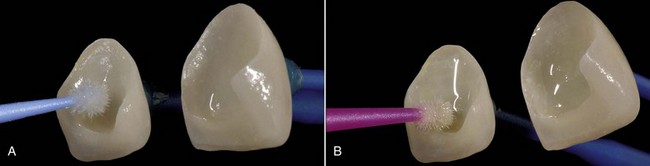
Pretreatment with hydrofluoric acid (which is the treatment recommended by the authors) is followed by chemical conditioning with the application of silane (Figure 8-12, A), which predisposes to covalent bonds, and hydrogen (Horn, 1983; Bailey, 1989).
Silane is considered the factor that most contributes to creating adequate adhesion between resin cements and glass ceramics (Paffenbarger, Sweeney, and Bowen, 1967; Horn, 1983; Calamia, 1985; Lacy and colleagues, 1988; Stokes, Hod, and Tidmarsh, 1988; Tjan and Nemetz, 1988; Bailey, 1989; Bertolotti, Lacy, and Watanabe, 1989; Diaz-Arnold and Aquilino, 1989; Diaz-Arnold, Schneider, and Aquilino, 1989; Diaz-Arnold and colleagues, 1993; Matsumura and colleagues, 1989; Cooley, Tseng, and Evans, 1991; Llobell and colleagues, 1992; Pratt and colleagues, 1992; Suliman, Swift, and Perdigao, 1993; Kern and Thompson, 1994; Thurmond, Barkmeier, and Wilwerding, 1994; Aida, Hayakawa, and Mizukawa, 1995; Kupiek and colleagues, 1996; Pameijer, Louw, and Fischer, 1996; Chen, Matsumura, and Atsuta, 1998a, 1998b; Kamada, Yoshida, and Atsuta, 1998; Shahverdi and colleagues, 1998; Braga and colleagues, 1999; Barghi, 2000; Della Bona, Anusavice, and Shen, 2000; Estafan and colleagues, 2000; Frankenberger, Kramer, and Sindel, 2000; Kato, Matsumura, and Atsuta, 2000; Rosentritt and colleagues, 2000; Szep and colleagues, 2000). Moreover, one of the aims of silane is to increase the wettability of ceramics, allowing better contact with the adhesive resin material. One study showed that without pretreatment with hydrofluoric acid, silane does not yield the same results, while the two procedures combined led to a decrease in marginal microleakage (Sorensen and colleagues, 1991).
Two-component silane ensures better stability by avoiding hydrolysis or dissolution of the solvent, as can happen when the silanization agent is in a single, ready-to-use solution. It is advisable to note the appearance of the silane before use. The solution should be clear. If it looks cloudy, it should not be used (Blatz, Sadan, and Kern, 2003b).
Before coming in contact with the cement, a light-curing resin bonding agent (see Figure 8-12, B), which can be filled to varying extents, is usually applied to the inner surface of the artifact. It is not generally cured until the restoration has been placed with the luting cement, and the excess material has been removed completely. The adhesive is applied very thinly with an applicator or a small brush and is left to settle for about 30 seconds. Then it is carefully blown with an air jet so that it will be spread only over the inner surface of the restoration.
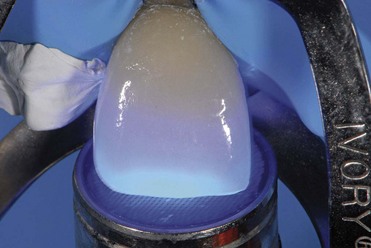
It is preferable that only light-curing cement be used with glass-ceramic restorations, especially if it is applied thinly, because the applied light has a high power (at least 1000 mW/cm2) and can completely convert the composite material through the ceramic layer. The main advantage of this system is that it permits complete removal of excess cement before polymerization, which will occur only if all the excess material is removed while the material is still in a plastic state (see Figure 8-8). Dual-cure composites not only leave the clinician very little time to remove the material that overflows during cementation, but they can also be too fluid, making/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses