Chapter 8 Adhesion
Section A The Evolution of Adhesive Techniques
Brief History of Clinical Development and Evolution of the Procedure
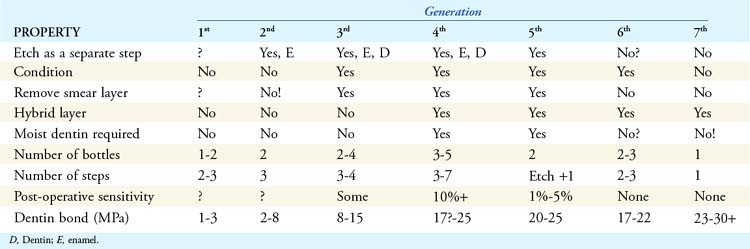
The “generational” definitions help to identify the chemistries involved, the strengths of the dentinal bond, and the ease of use for the practitioner (Box 8-1). Ultimately this type of classification benefits the dentist and patient by simplifying the clinician’s chairside choices.
Box 8.1 Generations of Dental Adhesives
Relating Function and Esthetics
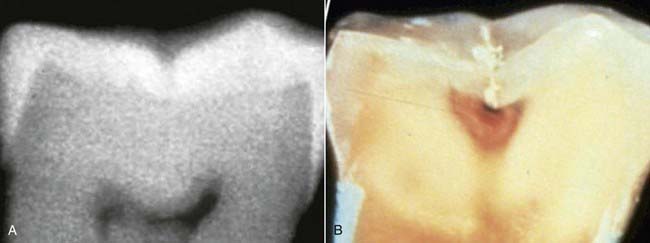
In many parts of the world, restorative dentistry has been described and taught as “conservative dentistry.” It has hardly been conservative of tooth structures, however; traditional methods and materials have been aggressive and highly invasive, requiring the removal of otherwise healthy enamel and dentin for various reasons, including extending the cavity for the retention of the final restoration and extending a preparation for the prevention of recurrent decay. Thus, healthy tooth structures were condemned to removal by the demands of non-adhesive restorative materials (Figure 8-1).
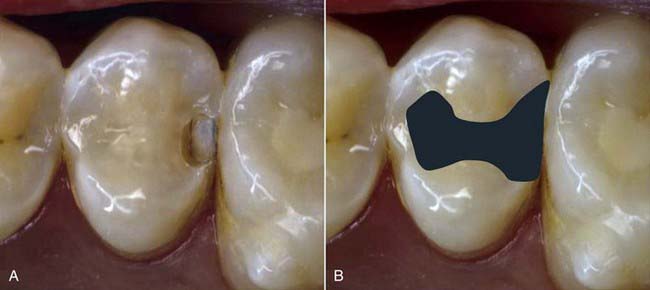
FIGURE 8-1 A, Small interproximal decay. B, Nonadhesive amalgam extended for retention and prevention.
Fortunately, the current era of dentistry has witnessed the development of new materials, new techniques, and new instruments that make conservative dentistry practical and ultraconservative dentistry a reality. Adhesive restorations eliminate the need for more extensive retentive preparations (Figure 8-2). Enamel-mimicking composites (both hybrid and flowable) offer long-lasting tooth structure replacement with minimum requirements for restorative bulk. Little or no healthy tooth material must be removed simply to allow for adequate thickness of the filling material. Innovative materials, particularly when combined with early detection and conservative treatment make the development of esthetics possible within every dental practice.
Clinical Considerations
Early Detection and Treatment
• How does one effectively diagnose these much smaller lesions in the teeth?
• Should these smaller lesions be left to grow larger for easier diagnosis and access or should they be intercepted while they are still small?
The accurate diagnosis of minute lesions may be quite difficult with traditionally accepted techniques. The shape of pit and fissure lesions tends to mask the size and extent of the defect when the dentist is using an explorer. Forty-two percent of these fissures have a narrow occlusal opening and vary in shape as they progress inward in the tooth. Caries is initiated in the lateral walls of the fissure and progresses downward toward the dentino-enamel junction (DEJ). The narrow occlusal opening tends to prevent the entry of the explorer into the larger chambers of the lesion. Often only a stickiness of the instrument in the tooth surface is reported. In fact, histologic cross-section has confirmed a ratio of only 25% accuracy in diagnosing decay underlying the occlusal surface using the traditional explorer method (Figure 8-3). This is hardly an impressive rate of success.
Radiographic diagnosis is an important tool for the practicing dentist. Radiographs can detect caries when none are observed clinically. However, negative radiographic results can be misleading. All too often the tooth has caries that the radiographic process will not reveal. This is known as the phenomenon of hidden caries, a condition in which the tooth appears caries free clinically and/or radiographically but is found to be carious by other diagnostic means (Figure 8-4, A). Subsequent cross-sectioning of the tooth clearly reveals caries that has originated at the base of a fissure and is now spreading along the DEJ (Figure 8-4, B).
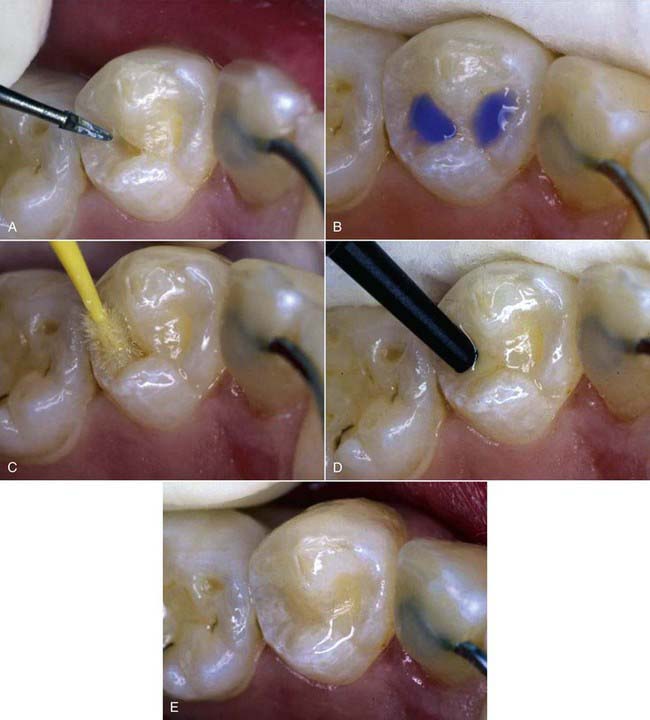
The practice of sealing pits and fissures has enjoyed widespread acceptance. There is continued concern, however, about the placement of sealants over undiagnosed caries. Because it is often difficult to determine the status of caries activity in fissures, an exploratory technique, or excisional biopsy, offers the best access and the best diagnostic and conservative technique for the maximum retention of healthy tooth structures combined with the assured removal of all decay. The excisional Fissurotomy bur (SS White Burs, Inc., Lakewood, New Jersey) remodels the anatomy of the fissure, facilitating the access, the acid etching, and the bonding of composite resin into the cavity preparation. lf this can be accomplished with minimal patient discomfort, preferably without any anesthetic, patient acceptance will be high, and the dentist’s conservationist goals can be attained (Figure 8-5).
Material Options
The dental practitioner has many options in the area of adhesives. As described earlier, there are seven distinct generations of adhesives. Each generation has its own advantages and disadvantages; some of the earlier generations are currently not in widespread use because better methods have superseded them quite effectively. Only generations four through seven are commonly used at this time (Table 8-1).
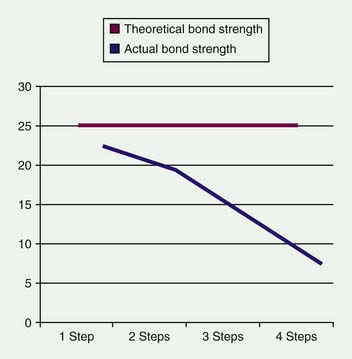
This generation was the first wherein the bonding strength to dentin was greater than the polymerization shrinkage of the composite. As a result, the composite did not shrink away from the tooth-resin interface during polymerization, thereby leaving a gap that could develop into a collector for oral fluids and bacteria. The drawback of fourth-generation systems was the need for multiple components. Kits had three to five components and required three to seven distinct steps in their protocol, a very time-consuming and technique-sensitive exercise. Certain components had to be mixed equally, and in a specific order, chairside. This is rather difficult to accomplish predictably on a regular basis, as evidenced by the common situation in which one of the “equal mix” components was always used up more quickly than the other. The unequal amounts of the components often compromised the adhesive strength of the bonding agent. Although the final bonding strength to dentin was theoretically 25 MPa, in actual fact it was often less than 17 MPa, the minimum adhesion needed to avoid marginal gaps caused by polymerization shrinkage of the composite. Clinically, the greater the number of steps, the greater the likelihood of inadvertent procedural error (Figure 8-6).
The chemistry of fifth (as well as sixth and seventh) generation adhesives is not compatible with dual cure restorative materials such as cements and core buildups. Thus, an accessory dual-cure additive was introduced by many manufacturers to make the strictly light-cured fifth-generation adhesives compatible with dual-cure restorative materials. Theoretically, the dual-cure fifth-generation adhesives were light initiated but would polymerize within 5 minutes in the absence of light, as well. According to a number of published reports based on clinical testing, only Pulpdent’s DenTASTIC UNO-DUO system (Figure 8-7, A) and Bisco’s One-Step Plus system (Figure 8-7, B) were shown to truly have dual-cure properties. Many practitioners who attempted the use of fifth-generation dual-cure products other than the two noted above were very disappointed with their cementation results.
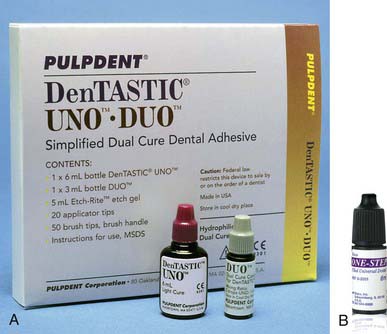
FIGURE 8-7 A, DenTASTIC UNO-DUO system. B, One-Step Plus system.
(A courtesy Pulpdent Corporation, Watertown, Massachusetts. B courtesy Bisco, Schaumburg, Illinois.)
Other Considerations
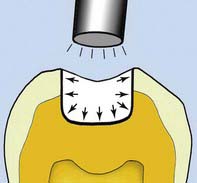
One of the most important clinical considerations for the selection of adhesive products is the bonding strength required at the adhesive interface. This question first arose with the development of adhesive materials in the 1950s, and it is still a somewhat controversial topic. Certain basic principles have been conclusively established and are well accepted. In the 1980s and 1990s, a number of studies, including Munksgaard in 1985 and Retief in 1994, found that a minimum of 17 MPa of adhesion to tooth structure was required for successful adhesion. The 17 MPa represents the force of the polymerization contraction of the composite resin restorative material. If there is less than 17 MPa of adhesion to either the enamel or the dentin, the polymerization force of the composite resin is greater than the force adhering the material to the enamel, dentin, or both. The forces of polymerization cause the resin to contract toward the center of the composite, pulling the restorative material away from the walls of the cavity (Figure 8-8). A small gap is created, which then allows micro-infiltration of bacteria and plaque that eventually causes marginal breakdown. The fluid inflow and outflow at the restorative interface carries bacteria and sugars deep into the tooth-restorative interface and eventually causes decay. In time, a dark line appears at the margin of the restoration.
Where the bonding agent’s adhesive strength to the dentin and the enamel exceed the 17 MPa of polymerization contraction, the shrinkage of the composite is toward the walls of the cavity (Figure 8-9). The laws of entropy dictate that the polymerization contraction process always tends to go in the direction of least resistance (or higher attraction). The composite is thus more attracted to the dentin and to enamel surfaces than it is to itself. Because the shrinkage is toward the walls and away from the center, no marginal gap develops. This makes marginal infiltration of bacteria and oral fluids far less likely, and thus prevents decay and eventual breakdown. The meniscus developed in the center of the restorative material is simply filled in by the next layer of composite resin. This is why an adhesive must have bonding strengths both to enamel and to dentin of more than 17 MPa to be clinically acceptable. Ideally, the bond strengths to enamel and dentin should be relatively equal. If, for example, the adhesion to the enamel is far greater than the bond to the dentin, the stronger force at the enamel interface will tend to pull the composite away from the dentinal margin during the polymerization process, weakening the dentin interface.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses