7
The MIS and V-MIS Surgical Procedure
Stephen K. Harrel
Introduction
Minimally invasive surgery (MIS) is based on the concept of using small incisions to perform surgical procedures that have previously been performed through larger surgical access openings. The term “minimally invasive surgery” was first applied to periodontal surgical procedures in 1995 [1]. The procedure was described as minimally invasive surgery or MIS. Several variations and techniques for performing MIS have been described. These include the original MIS approach that used surgical telescopes for visualization, a variation of this approach using the glass fiber endoscope for visualization, and the most recently described technique of Videoscope-Assisted MIS (V-MIS). Each of these techniques is considered to be an MIS technique with each change in visualization technology, thereby allowing for smaller incisions and greater magnification.
Following the initial description of MIS, the technique was further explored in several case series published over the next five years [2–5]. These papers reported excellent clinical results over an extended time period. The largest of these case series had 194 surgical sites that were followed for 9–54 months. All patients had closed scaling and root planing performed under local anesthetic at least 6 week before the surgical procedure. At the time of surgery, the pockets to be surgically treated ranged from 5 to 16 mm. The mean improvement in pocket probing depth was 4.58 mm, and the mean improvement in clinical attachment level (CAL) was 4.87 mm. A detailed description of the technique for performing MIS was published in 1999 [3].
Further research on MIS has been published more recently. A prospective study of the use of MIS with enamel matrix derivative (EMD) was published with 1-year data in 2005, and the 6-year data on the same cases published in 2010 [6,7]. These studies showed that there was a significant amount of improvement in pocket probing depth and CAL when MIS was performed. A total of 160 sites were treated with EMD using an MIS approach. The presurgical pocket probing depths following closed subgingival scaling and root planing were 5 mm or greater with a range of 5 mm–12 mm. At 1 year and at 6 years, the mean pocket probing depths were 3.09 mm and 3.06 mm, respectively. The mean improvement in CAL at 1 and 6 years post surgery was 3.33 mm and 3.36 mm, respectively. All pocket probing depths were less than 4 mm at all reevaluations. One of the most clinically significant findings in this study was the lack of clinically detectable recession at both measurement intervals. Recession is a major concern associated with all types of periodontal surgery. The lack of recession following MIS is an important finding because it indicates that the risk of unaesthetic gingival contours, food impaction, and thermal sensitivity is minimal following MIS regenerative surgery.
Recently, a videoscope has been designed for use with MIS [8,9]. This videoscope was described in Chapter 2. The use of the videoscope has allowed for smaller surgical access openings when performing MIS, and the procedure is described as Videoscope-Assisted Minimally Invasive Surgery V-MIS. A large university based study of V-MIS indicates that there is a further improvement over MIS when V-MIS is used. The mean presurgical pocket probing depths following closed subgingival scaling and root planing were 5.23 mm with a mean CAL of 5.86 mm and 0.82 mm of recession. At 6 months following V-MIS, the mean pocket probing depth was 2.28 mm while all pocket probing depths were less than 3 mm. There was an improvement in CAL of 3.00 mm. There was also a small, but statistically significant, improvement in soft tissue height of 0.29 mm [10]. This study further emphasizes that the MIS and specifically the V-MIS surgical technique yield good improvement in pocket probing depths and CAL while not causing clinical and esthetic complications associated with recession. The surgical technique described in this chapter will be based on the V-MIS approach to minimally invasive surgery.
Surgical principles
There are certain principles that guide all MIS procedures. The first is to preserve as much blood supply to the periodontal tissues as possible. Preserving the blood supply means that split thickness dissection is used for all flap reflection and a periosteal elevator is never used. This is a critical aspect of MIS. A major source of blood supply for the periodontal tissues is the periosteum. The reflection of the periosteum with a perosteal elevator significantly disturbs the blood supply to the gingival tissue and underlying bone. Care should be taken to leave the periosteum intact. The bone should only be exposed within the defect itself. A second principle of MIS is to cause minimum traumatic damage to the periodontal tissue. In most traditional regenerative periodontal surgery, it is routine to make large flaps and widely reflect the soft tissue from the bone. With MIS, care is taken to use as small an incision as possible, use split thickness dissection to reflect the soft tissue only to the edge of the osseous defect, and to put as little pressure on the tissue as possible. When successful, at closure the tissue should have the appearance of the surrounding un-incised tissue and to not have a bruised or cyanotic appearance. A third principle of MIS is to replace the soft tissue at or above the presurgical height with no tension on the tissue. Suturing is kept as simple as possible, and sutures are only placed at the base of the flap. The thin coronal portion of the papilla is never penetrated with a needle as it is felt this negatively impacts the blood supply to this thin vulnerable tissue. Instead of suturing the papilla, the tissue is approximated and positioned coronally by finger pressure on wet gauze. The use of the videoscope allows for smaller incisions and flaps that do not have to be reflected to the extent necessary with other means of visualization which aids closure of the tissue.
Steps in V-MIS or MIS
The surgical technique for MIS using either telescopes or a glass fiber endoscope and V-MIS using a videoscope is similar in many ways. The following description will detail the use of a videoscope for V-MIS. The same steps can be followed for MIS using surgical telescopes or a surgical microscope. With V-MIS, smaller access incisions and less flap reflection can be used than with traditional MIS surgical approaches. Major variations in technique necessitated by different visualization technology will be noted in the steps as they are described.
Case selection
V-MIS/MIS is usually indicated for isolated defects. Standard nonsurgical treatment (oral hygiene instruction, closed subgingival scaling and root planing, and occlusal adjustment where appropriate) should be performed prior to making a decision on the type of surgical approach that may be necessary. Often following nonsurgical treatment, a patient who initially presented with generalized periodontal inflammation will instead present with most pocket probing depths at an acceptable level for the maintenance of periodontal health. However, there will frequently be isolated, usually interproximal, defects that are 5 mm or greater in pocket probing depth. (Figure 7.1) The radiographs of these areas should be carefully evaluated and a decision made whether bone loss is present and if so are regenerative procedures indicated. If the defects are localized and are adjacent to periodontally healthy tissue, these defects are the ideal sites for using V-MIS.
Figure 7.1 Charting of a quadrant where V-MIS is indicated. Pocket probing depth chart post initial preparation indicating an isolated defect between the first and second molar. This isolated defect is ideally indicated for a V-MIS/MIS approach.
In cases where the periodontal destruction is more generalized with many contiguous areas of deeper pocket probing depths, it may not be possible to use a minimally invasive approach as it has been described in the literature. (Figure 7.2) However, many of the principles described for use with minimally invasive surgery such as smaller flaps and minimizing trauma to the tissue can still be used for the treatment of more generalized periodontal damage despite the necessity for a more extensive reflection of tissue. The videoscope because of its ability to provide improved visualization and magnification can be very useful in performing these more generalized (nonminimally invasive) surgical procedures.
Figure 7.2 Charting of a quadrant where more generalized (non-V-MIS/MIS) surgery is indicated. Pocket probing depth chart post initial preparation showing generalized defects that indicate the need for a more generalized surgical approach than V-MIS/MIS. Small incision surgery and the use of the videoscope will be of benefit for this case, but more extensive (longer) incisions will be necessary.
Incision and flap design
The flap design for V-MIS/MIS procedures will vary with the location, extent of the osseous defect, and visualization devices that are available. The presence of an osseous defect can be diagnosed with routine pocket measurements, but the extent of bone loss should be verified by bone sounding after the patient has been anesthetized. Where possible, only a single lingual or palatal flap is used. Lingual access and visualization is much easier when a videoscope is available. Lingual access approaches are difficult to use when surgical telescopes or a surgical microscope are used. These instruments give a straight view into the surgical field, which means a mirror must be used with a lingual flap approach. By contrast, the videoscope can be placed directly into the lingual opening, which results in a clear view of the surgical site. (Figures 7.3 and 7.4)
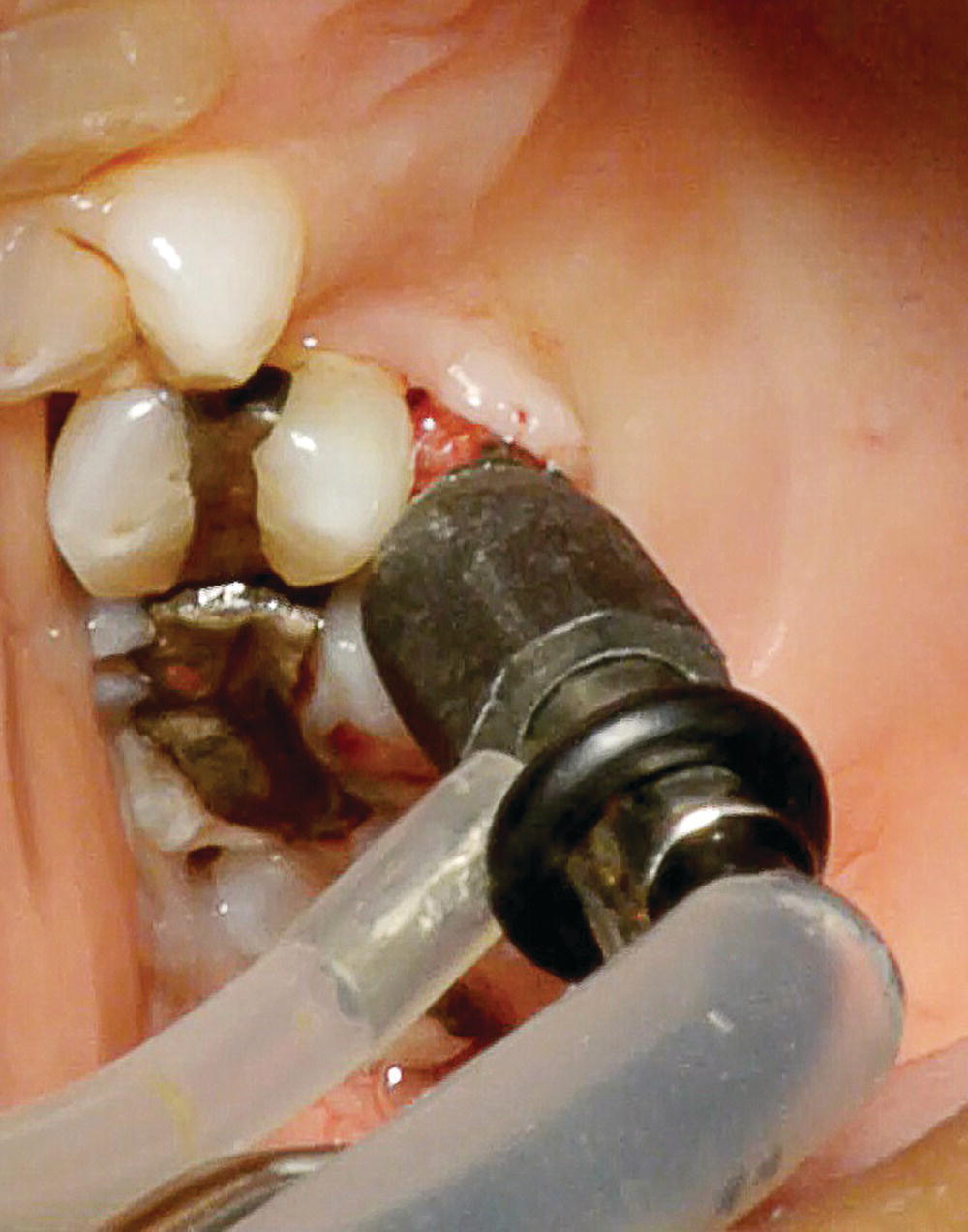
Figure 7.3 The videoscope is placed through a single MIS access flap on the palate allowing for full visualization of the interproximal defect.

Figure 7.4 The interproximal defect from Figure 7.3 as visualized by the videoscope.
Assuming an interproximal defect that does not extend beyond the line angles of adjacent teeth, the first incision is placed in the intersulcular space from the line angle of each tooth extending into the interproximal area. Care should be taken to stay in the sulcus and not remove a collar of tissue with this incision (Figure 7.5). This requires that the blade be placed against the tooth and pushed to the base of the defect. The blade should not be allowed to incise the tissue in the body of the papilla, and care should be taken to not cross the body of the papilla with these incisions. The second incision should be a horizontal (mesial-distal) incision across the body of the papilla (Figure 7.6). This incision should be placed relatively high on the papilla but not extend into the area of the col. The col should be preserved in place if at all possible. Once the horizontal incision is made, a split-thickness dissection is performed to create the access flap (Figure 7.7). This should be done only with sharp dissection. A periosteal elevator should never be used to elevate this flap.
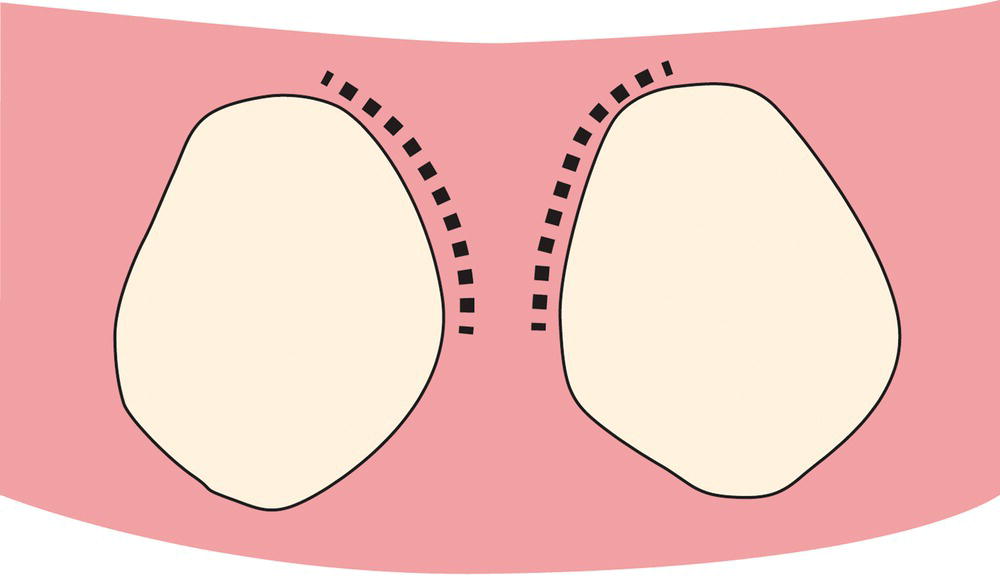
Figure 7.5 An outline drawing of the initial sulcular incisions. These initial incisions are made in the sulcus of the teeth adjoining the periodontal defect. The incisions are kept strictly within the sulcus by placing the blade against the adjacent root surface. No collar of tissue is removed with this incision, and care is taken to not join the two incisions.
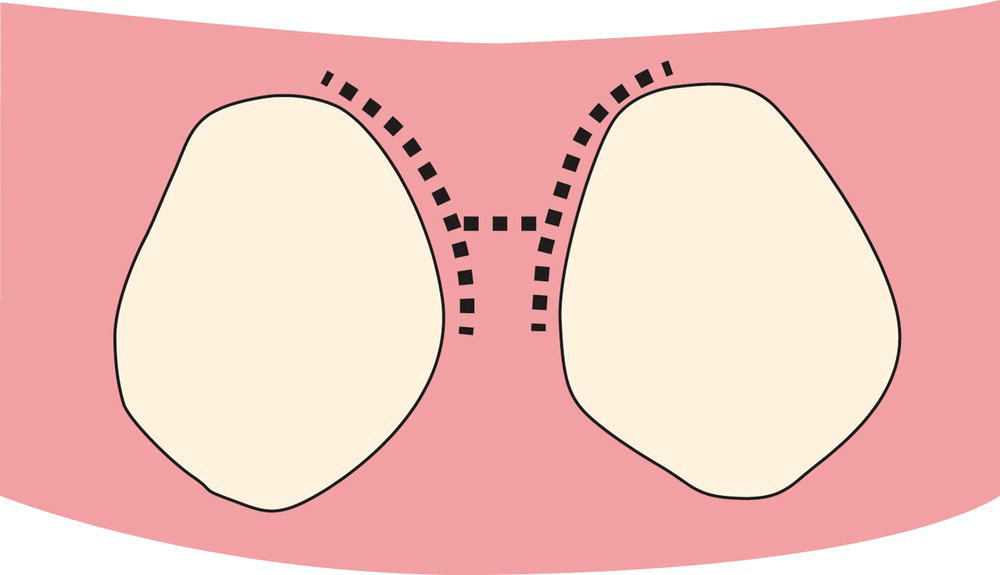
Figure 7.6 An outline drawing of the incision jointing the two sulcular incisions across the papilla. The two initial incisions are connected on the surface (buccal or lingual) where the access flap will be elevated. This connecting incision is made apical to the col tissue. The col tissue and the papilla on the nonsurgical side remain intact and are not elevated.
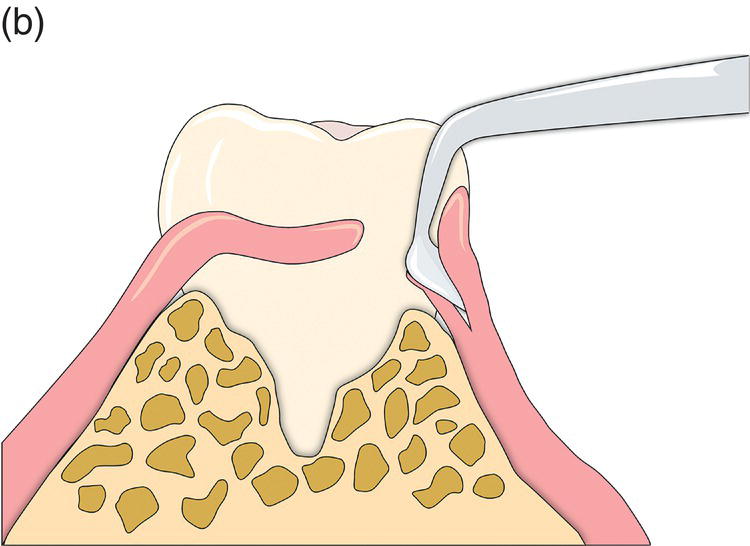
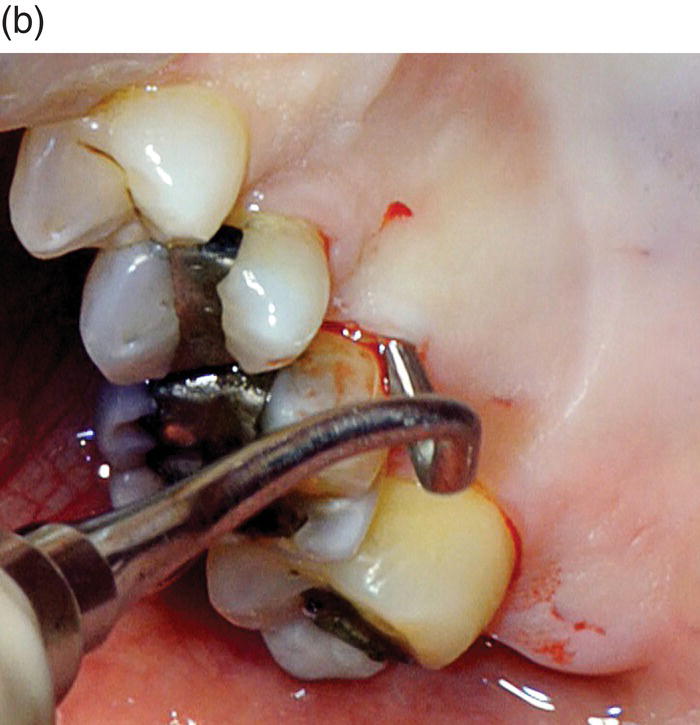
Figure 7.7 (a) Outline drawing of using a modified Orban knife to reflect the access flap. The access flap is reflected with sharp dissection only leaving the periosteum in place on the bone. A periosteal elevator should not be used. Because of its rigidity, a small Orban knife is ideal for this step. (b) Clinical use of a modified Orban knife for the sharp dissection.
Various blades can be used for making these incisions. The following suggestions for blades are those used by the author. The initial sulcular incisions are made with a 12b blade (Figure 7.8). This is a standard curved disposable scalpel blade where both edges of the curve are sharpened. This blade has the advantage of some rigidity and the ability to be utilized in a push–pull motion. This has been found to be very useful for the sulcular incisions. This blade may also be used to make the horizontal incision across the body of the papilla. The sharp dissection of the papilla is performed with a modified Orban knife. A standard Orban knife is reduced in size by approximately one third of its width (Figure 7.9). The rigidity of the Orban knife is very helpful for reflecting the flap because it allows for a split thickness dissection as well as the ability to “pull” on the flap as the incision is made. Other blades that may be helpful are the so-called microsurgical blades (Figure 7.10). The size of these blades allows good access to small spaces, but the blade’s lack of rigidity is often a significant impediment to their use. These blades also tend to have a “spring” that causes the blade to move suddenly when the blade “catches” on bone or calculus. This sudden movement of the very sharp blade may damage the tissue.
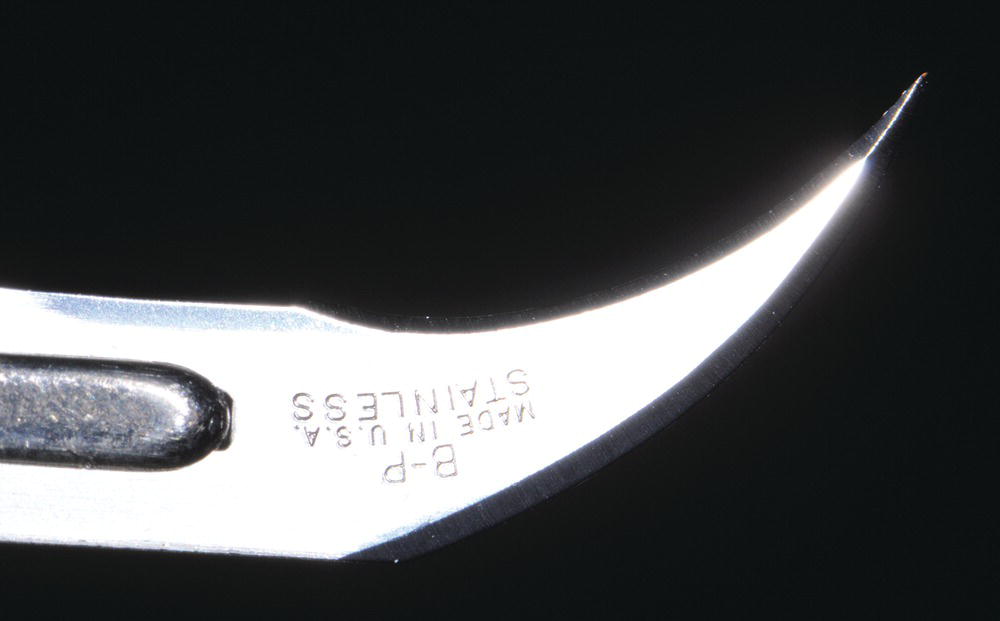
Figure 7.8 Because of its push–pull cutting capabilities and its relative rigidity, a disposable 12b blade is ideal for making the initial sulcular incisions and the incision across the papilla.
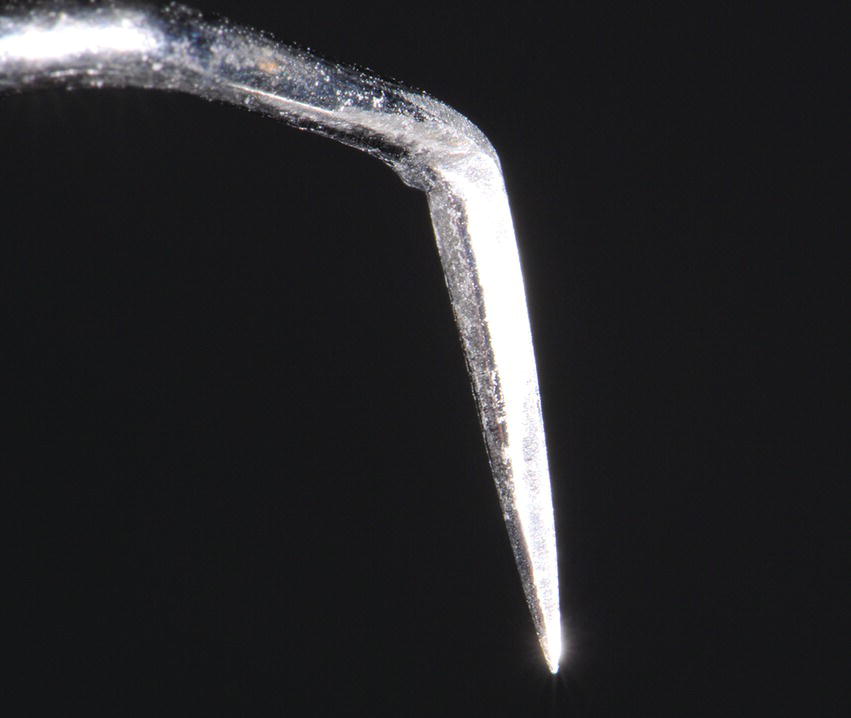
Figure 7.9 A standard Orban knife modified by reducing its width by approximately one third is ideal for making the split thickness incision that is used to elevate the access flap. The rigidity of this blade allows for the cutting of the tissue and also displacing/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


