chapter 7 Oral Sedation
ADVANTAGES
The oral route possesses several advantages over other routes of drug administration:
Complications are possible whenever drugs are administered, regardless of the route of administration. Drug idiosyncrasy, allergy, and overdose in addition to other adverse actions can and do occur. Drug-related side effects are less likely to develop after enteral drug administration (i.e., oral, rectal) than after parenteral drug administration. In addition, adverse reactions following oral administration are often much less intense than those noted following parenteral administration of the same drug. This is not to imply that serious complications do not occur following oral drug administration. Berger, Green, and Melnick1 reported cardiac arrest following oral diazepam intoxication, and Gill and Michaelides2 described an anaphylactic response to oral penicillin. Other serious adverse reactions to orally prescribed drugs, including suicide, have been reported.3–5
DISADVANTAGES
Disadvantages associated with the oral route include the following:
When prescribing drugs for oral administration before coming to the dental office, the dentist must rely on the patient to take the drug as prescribed (the proper dose at the proper time). Although most patients will medicate themselves properly, some do not. This potential problem, termed noncompliance, is significant in medicine, especially in relation to long-term drug administration (e.g., antihypertensive drugs). The Council on Patient Information and Education estimates that 35% to 50% of all prescriptions dispensed by physicians are taken incorrectly by patients and that one in five patients never even bother to have the prescription filled. One in seven stops taking the drug too soon. Noncompliance rates among patients older than 65 years are more than 55%.6 Although noncompliance is not as critical a problem in the dental situation, the administration of too small or too large a dose, too soon or too late, may significantly alter the drug’s effectiveness during the treatment period. A common form of noncompliance is the taking of a dose larger than that prescribed; the patient’s rationale is “if one (tablet or capsule) is good, then two or more will be better.” This type of thinking leads to oversedation, overdose, and other unwanted and unpleasant complications. Fortunately (in this situation, at least) the erratic and incomplete absorption of orally administered drugs minimizes the development of serious problems from drug overadministration.
On many occasions, I have observed this phenomenon in pediatric dental patients: A parent or guardian administers a tablespoon of drug instead of a teaspoon, or a larger dose than desired, because the child did not take all of the first dose. Significant overdose, with attendant respiratory depression, can develop in this manner if the administered drug is a CNS depressant. The consequences of these actions are formidable, with potential morbidity or mortality as the result. This has led to the enactment of legislation in a number of states restricting the use of oral sedation in patients younger than 13 years of age to dentists who have received appropriate education and training in this patient population.7 Oral sedation regulations vary considerably.
Oral Sedation in Children. As of April 2008, the American Dental Association (ADA) was aware of three states having enteral sedation permits specific to administration to minors (e.g., Louisiana has a permit entitled “restricted” that allows the dentist to administer to adults only). Three other states mention within their enteral sedation permit language stating, “additional training requirements to administer to children.” Three other states have language within their enteral sedation laws that require the dentist to have a parenteral “conscious” sedation permit to administer enteral to children.7
Oral Sedation in Adults. The ADA is aware of two states having oral sedation permits specific to adults. This does not take into account those other states that require the dentist to obtain a parenteral sedation permit to administer to children. For example, Idaho has a limited permit and comprehensive permit. The comprehensive (IV sedation) permit is required to administer to children; therefore one could argue that the limited is an adult-only permit.7
Oral Sedation, in General to Any Patient. Absent occasional references to PALS (pediatric advanced life support) for dentists treating pediatric patients, the ADA is aware of 14 states that have fairly straightforward options for enteral permits that do not mention additional training for administration to pediatric or minor patients.7
Absorption
Because the small intestine is the primary site for drug absorption, it is important to get the drug through the mouth, esophagus, and stomach and into the small intestine as rapidly as possible. The removal of foods and other substances from the stomach occurs by contraction of the antrum of the stomach. The time required for a substance to be expelled from the stomach is the gastric emptying time. Liquids, when taken alone, require approximately 90 minutes to be removed, and a mixed meal of food and liquid requires about 4 hours to reach the duodenum. Liquids are discharged from the stomach into the duodenum at a rate of 10 ml/min. The presence of fat in the stomach significantly increases gastric emptying time. It is therefore recommended, as a general rule, that oral drugs be taken with a glass of water (approximately 8 oz) in the absence of food. In this manner, the drug’s delivery to the duodenum is maximized, permitting more reliable absorption. Anxiety is another factor that delays gastric emptying. It is estimated that gastric emptying time can be delayed by as much as two times in the fearful patient,8 thereby delaying the onset of action of antianxiety drugs. Thus a negative cycle is established. Oral antianxiety drugs are administered 1 hour before treatment to lessen the patient’s fear of impending dental or surgical care, yet the very fear that we are seeking to manage inhibits the absorption of the drug into the cardiovascular system. This helps explain why, in the presence of extreme fear, orally administered drugs may prove ineffective despite having been administered as directed by the dentist.
Drugs administered in aqueous solution are more rapidly absorbed than those given as an oily solution or in tablet or capsule form. The tablet or capsule must first dissolve in the gastric fluid before absorption can occur. Once it has dissolved, the size of the resulting particles of drug is important. The smaller the particle is, the greater the rate of drug absorption.9 There is significant variation in the clinical effectiveness of different forms (i.e., liquid, capsule, tablet) of the same drug (see Bioavailability).
Some drugs, such as morphine, cannot be administered orally because a significant level of drug inactivation occurs before they reach the cardiovascular system. Although the acidity of the stomach is the major cause of this, intestinal contents can also affect the actions of oral drugs. The hepatic first-pass effect is also involved. Drugs absorbed from the GI tract (stomach, intestine, colon) are first delivered to the liver via the hepatic portal system before entering into the systemic circulation. The liver is rich in enzymes that biotransform certain drugs into pharmacologically inactive byproducts. A prime example of this is the antidysrhythmic drug lidocaine. Lidocaine is so completely transformed via the hepatic first-pass effect that the drug is essentially useless when administered orally.10 However, modifying the chemical structure of lidocaine produced the chemical analog tocainide, which is clinically effective as an oral antidysrhythmic.11 In the area of drugs used for anxiety reduction, there is a subtle (but not clinically significant) hepatic first-pass effect noted with the opioid analgesics.
The presence of food in the stomach decreases absorption of drugs into the cardiovascular system by increasing gastric emptying time, and if the drug is bound to food, it will not be available for absorption.12 As mentioned previously, it is recommended that oral drugs be ingested with a full glass of water without food (unless a drug specifically requires that it be administered along with food as a means of minimizing gastric upset).
RATIONALE FOR USE
A second use for oral sedation is one that is often overlooked by a busy clinician. As noted earlier (see Chapter 4), not only do patients with fears of dentistry or surgery become apprehensive immediately before their appointment, often their anxieties start to build the day before the scheduled appointment. These persons might be unable to sleep the night before the appointment as they anticipate their upcoming “ordeal” and will be fatigued when they appear in the dental office the next day, a factor leading to a lowering of the pain reaction threshold. An antianxiety or hypnotic drug taken 1 hour before sleep (1 hr hs) the night before the appointment can help ensure a restful night’s sleep and a more stress-tolerant patient during treatment.
DRUGS
A source of information regarding recommended dosages of drugs is the drug package insert or publications such as Facts and Comparisons,13 Physicians’ Desk Reference,14 or Mosby’s Dental Drug Reference, eighth edition.15 Online sources of drug information, such as ePocrates.com16 or Mosby’s MD Consult17 are readily available for downloading onto a desktop computer or hand-held device. An advantage of online drug data resources is that they are updated on a regular basis.
A common problem associated with the use of recommended doses is that they often lead to inadequate anxiety reduction in the dental or surgical setting. There is a reasonable explanation for this: The package insert recommends a certain dose of a drug to induce sedation or sleep in a nonstress situation, such as the home environment. The dose of a drug that would effectively relax an apprehensive individual at home will probably prove ineffective when the stresses of the dental office environment are added. For this reason, the doses recommended for oral sedation in this chapter and in many textbooks of pediatric dentistry may be somewhat higher than those in the package inserts.18,19
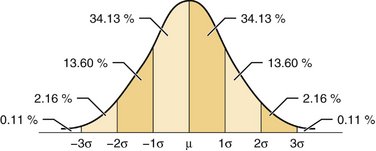
Many antianxiety and sedative-hypnotic drugs for oral administration are produced in three dosage forms. When a dosage is chosen for stress reduction in dental practice, these three dosage forms correlate with the normal distribution (“bell-shaped”) curve (Figure 7-1). The middle dosage form represents the “average” dose, producing clinically effective results (in nonstress situations) in approximately 70% of persons receiving it. The larger dosage form is for persons in whom the average dose proves to be ineffective or who have a greater degree of anxiety. The smaller dosage form is for persons in whom the average dose provides too intense a clinical effect, for persons with a lesser degree of anxiety, for elderly patients, or for debilitated patients. It must be remembered that the added stresses associated with dental or surgical treatment will increase the percentage of patients requiring larger than “usual” doses for management of their treatment-related fears.
Although titration (individualization of drug dosages) is not possible with orally administered drugs—a significant impediment to their safe use—it is possible in situations in which oral drugs are to be used over multiple appointments to titrate by appointment. This concept was introduced to me by Dr. Ronald Johnson, then chairman of the Department of Pediatric Dentistry at the University of Southern California.20 Quite simply, titration by appointment means that the dentist will assess the efficacy of sedation achieved at the first appointment with a given drug dosage and, if necessary, increase or decrease the dosage of drug(s) administered at subsequent appointments. Therefore over a period of two to three visits, the appropriate dosage for that patient can be achieved (titrated). Titration by appointment is discussed more fully in the chapter on pediatric sedation (see Chapter 35).
ANTIANXIETY DRUGS
Benzodiazepine Antianxiety Agents
The benzodiazepines are the most effective drugs currently available for the management of anxiety. They also possess skeletal muscle–relaxant properties and are anticonvulsants. More than 2000 benzodiazepines have been synthesized since 1933. Chlordiazepoxide was the first benzodiazepine introduced (1960). In 2008 (May) 31 benzodiazepines (Table 7-1) were available worldwide. Fourteen of the commonly used benzodiazepines are categorized as sedative-hypnotics, 15 as anxiolytics, 7 indicated for use as antiepileptic drugs, and 1 as a skeletal muscle relaxant. (Some drugs are indicated for more than one group.)
| Sedative-Hypnotic Benzodiazepines |
Pharmacology
Mode of Action
Specific receptors for benzodiazepines have been isolated within the spinal cord and the brain. The location of these receptors parallels that of γ-aminobutyric acid (GABA), the major inhibitory neurotransmitter in the brain, and of glycine, the major inhibitory neurotransmitter in the spinal cord.22 Benzodiazepines act by intensifying the physiologic inhibitory effects of GABA by interfering with GABA reuptake.23–25
Central Nervous System
The principal behavioral effects of the benzodiazepines are the following:
It is interesting that when aggression and hostility are held in check by fear and anxiety, the ingestion of a benzodiazepine or other anxiolytic drug may produce a “paradoxic” increase in aggression. Other CNS depressants, such as the barbiturates, produce these same effects, but only at doses that produce drowsiness and motor incoordination. The benzodiazepines commonly achieve this action without these side effects.26
Other CNS actions of the benzodiazepines include skeletal muscle–relaxant properties and anticonvulsant effects.27,28 The site of action of the muscle-relaxant properties of benzodiazepines is as yet undetermined; however, it is thought that the effect is central rather than peripheral. Skeletal muscle relaxation appears to be caused by a combination of central depression of the brainstem reticular formation and depression of polysynaptic spinal reflexes.27,29 Anticonvulsant actions of benzodiazepines are produced by a depression of epileptiform discharge in the cerebral cortex and an enhancement of electrical activity of Purkinje cells. For effective anticonvulsant activity, the benzodiazepines must be administered intravenously (although intramuscularly and intranasally administered midazolam has terminated seizures).30 Diazepam and clonazepam are currently approved for anticonvulsant therapy.
Respiratory System
All sedative-hypnotics and antianxiety drugs (including benzodiazepines) are potential respiratory depressants. At usual therapeutic oral dosages in healthy normal-responding patients (middle of the bell-shaped curve), the benzodiazepines, administered alone, do not produce clinically significant respiratory depression and do not potentiate the depressant effects of opiates. Cases of significant respiratory depression and respiratory arrest following oral benzodiazepine ingestion have been reported.31,32
Cardiovascular System
Following oral administration to a healthy patient (American Society of Anesthesiologists [ASA] 1), benzodiazepines produce virtually no changes in cardiovascular function. Indeed, the benzodiazepines are frequently used in the management of anxiety and depression associated with cardiac disease. They are preferred to the barbiturates and other sedative-hypnotics in this situation primarily because they do not produce unwanted degrees of CNS depression or restlessness and because they do not produce cardiovascular depression at therapeutic levels.33
Absorption, Metabolism, Excretion
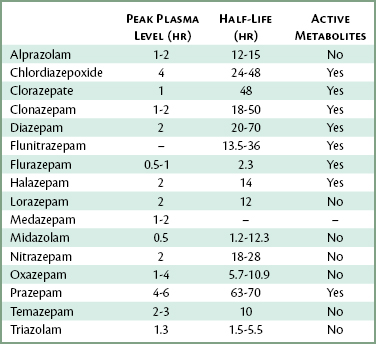
Following oral administration, all benzodiazepines are absorbed relatively rapidly and reliably from the GI tract. The rate at which maximum plasma levels develop exhibits significant variation among the different benzodiazepines and among individuals. Approximate time for peak plasma levels following oral administration of several benzodiazepines is shown in Table 7-2.
Table 7-2 Onset of Peak Plasma Levels Following Oral Administration of Benzodiazepines
| Drug | Peak Plasma Level (hr) |
|---|---|
| Flurazepam | 0.5-1 |
| Midazolam | 0.5 |
| Triazolam | 1.3 |
| Medazepam | 1-2 |
| Alprazolam | 1-2 |
| Oxazepam | 1-4 |
| Nitrazepam | 2 |
| Diazepam | 2 |
| Lorazepam | 2 |
| Halazepam | 2 |
| Temazepam | 2-3 |
| Chlordiazepoxide | 4 |
| Prazepam | 4-6 |
Benzodiazepines undergo biotransformation in the liver. There is considerable variation in the half-lives of these drugs: Diazepam’s elimination half-life is 20 to 70 hours, whereas triazolam’s is 1.5 to 5.5 hours. In addition, many of the benzodiazepines have biotransformation products that are pharmacologically as active as the parent drug (Table 7-3).
Nitrazepam, oxazepam, lorazepam, midazolam, triazolam, temazepam, and alprazolam are biotransformed into pharmacologically inactive metabolites. The combination of rapid absorption from the GI tract (1 to 4 hours), short elimination half-life (5.7 to 9 hours), and inactive metabolites makes oxazepam an attractive drug for the management of anxiety within the dental or surgical environment. Lorazepam, on the other hand, with a slow rate of absorption (2 hours) and a half-life of 12 hours (range 9 to 24 hours), is less appealing. Triazolam, with a rapid onset of action and short half-life (1.5 to 5.5 hours), is ideally suited as a hypnotic in dentistry.34–36
Dependence
Psychological and physiologic dependence may develop to benzodiazepines.37 The incidence of physiologic dependence is considerably less than that of psychological dependence. Physiologic dependence is unlikely to develop unless the patient takes doses much greater than therapeutically necessary over long periods of time. Within the dental setting, there is little likelihood of this occurring.
Oral Benzodiazepines in Dentistry
Although there are indications for the use of other drugs in specific instances, the drugs most ideally suited for pretreatment anxiolysis via oral administration in the dental and surgical setting are oxazepam and diazepam. For patients requiring sedation (hypnosis) to sleep restfully the evening before their treatment, flurazepam and triazolam are preferred. In the past decade, oral triazolam has become a very popular drug for the provision of minimal to moderate sedation in dentistry in North America.38–40 Triazolam will be reviewed in depth in the section of sedative-hypnotic benzodiazepines.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses