Neoplasia
Anne Cale Jones, Paul D. Freedman, Joan Andersen Phelan and John E. Kacher
After studying this chapter, the student will be able to:
1. Define each of the words in the vocabulary list for this chapter.
2. Explain the difference between a benign tumor and a malignant tumor.
3. Define leukoplakia and erythroplakia.
4. Describe the clinical and microscopic features of a calcifying odontogenic cyst and compare and contrast this lesion with an ameloblastoma.
5. Define each of the following neoplasms, describe the clinical features of each, and explain how they are treated: papilloma, squamous cell carcinoma, verrucous carcinoma, basal cell carcinoma, pleomorphic adenoma, trabecular and canalicular adenoma, adenoid cystic carcinoma, mucoepidermoid carcinoma, ameloblastoma, calcifying epithelial odontogenic tumor, adenomatoid odontogenic tumor, odontogenic myxoma, central cementifying and ossifying fibromas, benign cementoblastoma, ameloblastic fibroma, ameloblastic fibro-odontoma, odontoma, peripheral ossifying fibroma, lipoma, neurofibroma and schwannoma, granular cell tumor, congenital epulis, rhabdomyosarcoma, hemangioma, lymphangioma, Kaposi sarcoma, melanocytic nevi, malignant melanoma, torus, exostosis, osteoma, osteosarcoma, chondrosarcoma, leukemia, lymphoma, multiple myeloma, and metastatic jaw tumors.
Aberrant ( ) Deviating from the usual or natural type; atypical.
) Deviating from the usual or natural type; atypical.
Benign ( ) A condition that is not life-threatening, not cancerous, not malignant.
) A condition that is not life-threatening, not cancerous, not malignant.
Benign tumor ( ) A tumor that is not malignant and favorable for treatment and recovery.
) A tumor that is not malignant and favorable for treatment and recovery.
Carcinoma ( ) Malignant tumor of the epithelium.
) Malignant tumor of the epithelium.
Central ( ) In oral pathology, describing a tumor or lesion occurring within bone.
) In oral pathology, describing a tumor or lesion occurring within bone.
Dysplasia ( ) Disordered growth; alteration in size, shape, and organization of adult cells.
) Disordered growth; alteration in size, shape, and organization of adult cells.
Encapsulated ( ) Surrounded by a dense band of fibrous connective tissue.
) Surrounded by a dense band of fibrous connective tissue.
Enucleation ( ) Complete surgical removal without cutting into the lesion.
) Complete surgical removal without cutting into the lesion.
Hyperchromatic ( ) Microscopic staining that is more intense than normal.
) Microscopic staining that is more intense than normal.
Hyperplasia ( ) Abnormal increase in the number of cells in an organ or tissue.
) Abnormal increase in the number of cells in an organ or tissue.
In situ ( ) Confined to the site of origin without invasion of neighboring tissues.
) Confined to the site of origin without invasion of neighboring tissues.
Invasion ( ) Infiltration and active destruction of surrounding tissues.
) Infiltration and active destruction of surrounding tissues.
Malignant ( ) Tending to produce death, able to metastasize; describing cancer.
) Tending to produce death, able to metastasize; describing cancer.
Neoplasia ( ) New growth; the formation of tumors by the uncontrolled proliferation of cells.
) New growth; the formation of tumors by the uncontrolled proliferation of cells.
Neoplasm ( ) Tumor; a new growth of tissue in which growth is uncontrolled and progressive.
) Tumor; a new growth of tissue in which growth is uncontrolled and progressive.
Neoplastic ( ) Pertaining to the formation of tumors by the uncontrolled proliferation of cells.
) Pertaining to the formation of tumors by the uncontrolled proliferation of cells.
Oncology ( ) The study of tumors or neoplasms.
) The study of tumors or neoplasms.
Pedunculated ( ) Attached by a stalk.
) Attached by a stalk.
Peripheral ( ) In oral pathology, describing a lesion that occurs on the gingiva or alveolar mucosa.
) In oral pathology, describing a lesion that occurs on the gingiva or alveolar mucosa.
Pleomorphic ( ) Occurring in various forms.
) Occurring in various forms.
Primary tumor (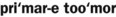 ) Original tumor; the source of metastasis.
) Original tumor; the source of metastasis.
Sarcoma ( ) Malignant tumor of the connective tissue.
) Malignant tumor of the connective tissue.
Sessile ( ) Attached by a broad base.
) Attached by a broad base.
Classification of Tumors
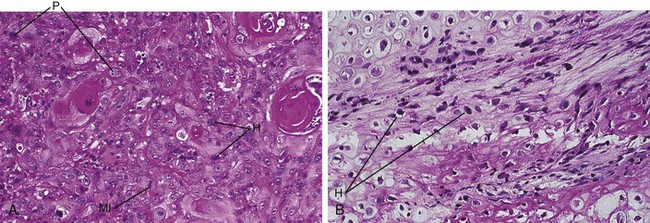
Benign tumors almost always resemble normal cells, whereas malignant tumors vary in their microscopic appearance. Malignant tumors composed of neoplastic cells that resemble normal cells are called well-differentiated tumors. Malignant tumors may also be poorly differentiated. The cells of these tumors have only some of the characteristics of the tissue from which they were derived. Still others may be undifferentiated or anaplastic and do not resemble at all the tissue from which they were derived. Malignant tumors are often composed of cells that vary in size and shape (pleomorphic) (Figure 7-1). The nuclei of these cells are darker than those of normal cells (hyperchromatic) and exhibit an increased nuclear-to-cytoplasmic ratio (Figure 7-1). Normal and abnormal mitotic figures are seen in the nucleus of the neoplastic cells (Figure 7-1, A). Abnormal mitotic figures are those that are not dividing normally; therefore the shape of the dividing nucleus does not follow the shape of a normal mitotic figure. Table 7-1 compares benign and malignant tumors.
TABLE 7-1
Comparison of Benign and Malignant Tumors
| BENIGN | MALIGNANT |
| Usually well differentiated | Well differentiated to anaplastic |
| Usually slow growth | Slow to rapid growth |
| Mitotic figures are rare | Mitotic figures may be numerous |
| Usually encapsulated | Invasive and unencapsulated |
| No metastasis | Metastasis likely |
Names of Tumors
The prefix of the name of a tumor is determined by the cell or tissue of origin. The suffix –oma is used to indicate a tumor. The prefix of the name of a benign or malignant tumor is also determined by the cell or tissue of origin. For example, a benign tumor of fat is called a lipoma, and a benign tumor of bone is called an osteoma. Malignant tumors are named in a similar fashion. Malignant tumors of epithelium are called carcinomas, and malignant tumors of connective tissue are called sarcomas. Therefore a malignant tumor of squamous epithelium is called a squamous cell carcinoma or an epidermoid carcinoma, and a malignant tumor of bone is called an osteosarcoma (osteogenic sarcoma). Carcinomas are about 10 times more common than sarcomas. Table 7-2 lists tumors according to their tissue or cell of origin.
TABLE 7-2
| TISSUE OF ORIGIN | BENIGN TUMOR | MALIGNANT TUMOR |
| Epithelium | ||
| Squamous cells | Papilloma | Squamous cell or epidermoid carcinoma |
| Basal cells | Basal cell carcinoma | |
| Glands or ducts | Adenoma | Adenocarcinoma |
| Neuroectoderm | ||
| Melanocytes | Nevus | Melanoma |
| Connective Tissue | ||
| Fibrous | Fibroma | Fibrosarcoma |
| Cartilage | Chondroma | Chondrosarcoma |
| Bone | Osteoma | Osteosarcoma |
| Fat | Lipoma | Liposarcoma |
| Endothelium | ||
| Blood vessels | Hemangioma | Angiosarcoma |
| Lymphatic vessels | Lymphangioma | Lymphangiosarcoma |
| Muscle | ||
| Smooth muscle | Leiomyoma | Leiomyosarcoma |
| Striated muscle | Rhabdomyoma | Rhabdomyosarcoma |
Tumors of Squamous Epithelium
Papilloma
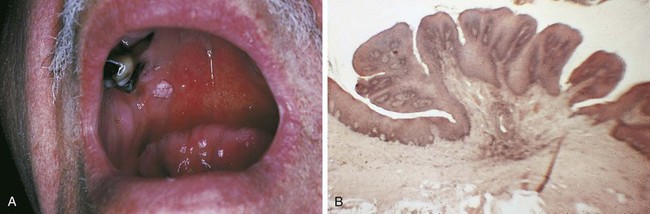
The papilloma is a benign tumor of squamous epithelium that presents as a small, exophytic, pedunculated or sessile growth. These tumors are composed of numerous papillary projections that may be either white or the color of normal mucosa (Figure 7-2). The color of the lesion depends on the amount of surface keratin; the more keratin, the whiter the lesion appears clinically.
Other oral lesions that may resemble a papilloma clinically are a verruca vulgaris (common wart) and condyloma acuminatum (venereal wart). These two lesions are caused by human papillomaviruses and are described in Chapter 4. They are differentiated from the papilloma by microscopic examination. Special procedures can be used to identify specific viral particles within these lesions. Evidence suggests that low-risk types of HPV are involved in the etiology of oral squamous papillomas, but microscopic evidence of HPV infection is generally not present in squamous papillomas.
Premalignant Lesions
Leukoplakia
In any discussion of premalignant lesions of the oral mucosa, it is important to define the term leukoplakia. Leukoplakia is a clinical term and does not refer to a specific microscopic appearance. It is defined as a white plaquelike lesion of the oral mucosa that cannot be rubbed off and cannot be diagnosed clinically as a specific disease (Figure 7-3, A and B).
Leukoplakia is sometimes referred to as idiopathic leukoplakia to emphasize that the specific cause of the lesion is not known. The white lesion illustrated in Figure 7-4 is more accurately called smokeless tobacco–associated keratosis rather than a leukoplakia because the direct cause of the lesion is known.
Erythroplakia
Erythroplakia is a clinical term used to describe an oral mucosal lesion that appears as a smooth red patch or a granular red and velvety patch (see Figure 7-3, C). A lesion that shows a mixture of red and white areas is generally called speckled leukoplakia rather than erythroplakia. Most cases of erythroplakia occur in the floor of the mouth, tongue, and soft palate. Erythroplakia is much less common than leukoplakia. In one study 60 cases of leukoplakia were seen for every 1 case of erythroplakia. When examined microscopically, 90% of cases of erythroplakia demonstrate epithelial dysplasia or squamous cell carcinoma. Because of these microscopic findings, erythroplakia is considered a more serious clinical finding than leukoplakia (a biopsy must be performed to establish a definitive diagnosis).
Treatment of erythroplakia depends on the microscopic diagnosis.
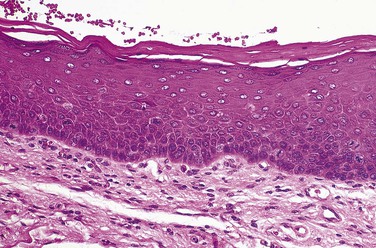
Epithelial Dysplasia
Microscopic examination of epithelial dysplasia demonstrates abnormal maturation of epithelial cells with disorganization of the epithelial layers; hyperplasia of the basal cells; and epithelial cells with enlarged and hyperchromatic nuclei, increased nuclear-to-cytoplasmic ratios, abnormal keratinization, and increased numbers of normal and abnormal mitotic figures (Figure 7-5). Microscopically, epithelial dysplasia differs from squamous cell carcinoma in that there is no invasion of the abnormal epithelial cells through the basement membrane into the underlying tissue. Severe dysplasia involving the full thickness of the epithelium is called carcinoma in situ.
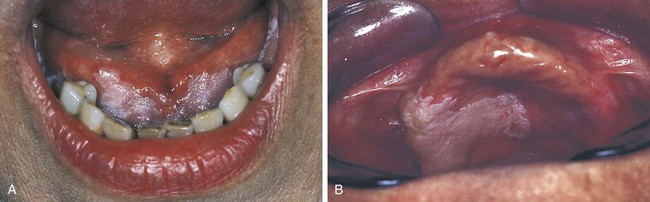
Squamous Cell Carcinoma
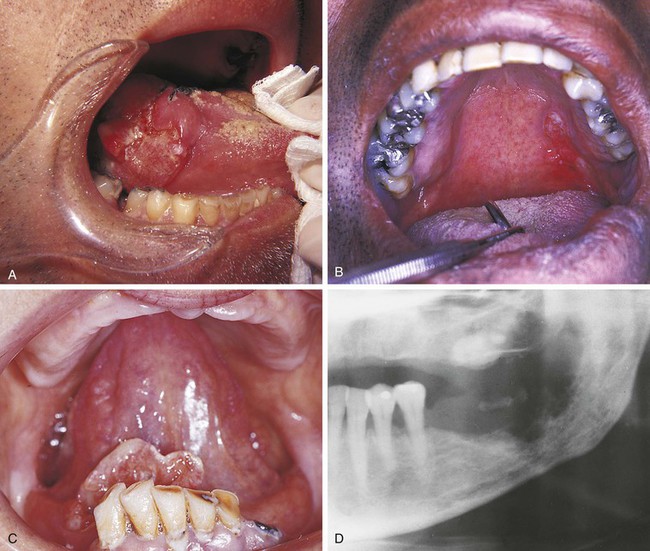
Squamous cell carcinoma, or epidermoid carcinoma, is a malignant tumor of the squamous epithelium. It is the most common primary malignancy of the oral cavity and, like other malignant tumors, can infiltrate adjacent tissues and metastasize to distant sites. Squamous cell carcinoma usually metastasizes to lymph nodes of the neck and then to more distant sites such as the lungs and liver. Clinically, squamous cell carcinoma usually presents as an exophytic ulcerative mass (Figure 7-6), but early tumors may be white and plaquelike (leukoplakia), erythematous (red) and plaquelike (erythroplakia), or a mixture of erythematous and white areas (speckled leukoplakia). Squamous cell carcinoma can infiltrate and destroy bone (Figure 7-6, D).
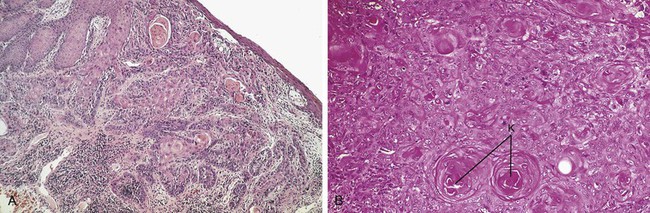
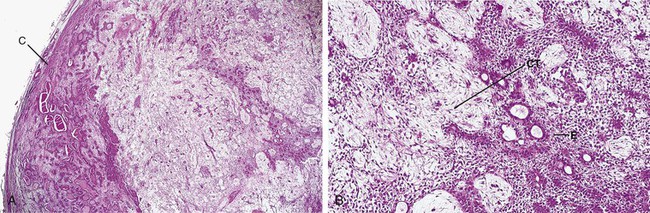
The essential microscopic feature of a squamous cell carcinoma is the invasion of tumor cells through the epithelial basement membrane into the underlying connective tissue (Figure 7-7, A). Invasive sheets and nests of neoplastic squamous cells characterize this tumor. Although squamous cell carcinoma is a malignant tumor, it exhibits features that allow the cells to be recognized as squamous epithelial cells. In well-differentiated tumors these features are easily recognized; however, they may not be easily seen in a poorly differentiated squamous cell carcinoma. Because keratin is a product of squamous epithelium, well-differentiated tumors show keratin formation. In addition to normal surface keratin, the keratin may be seen in individual cells within the tumor and as structures called keratin pearls (Figure 7-7, B). The neoplastic cells are not normal cells. They contain large hyperchromatic nuclei and numerous mitotic figures. Some of the mitotic figures appear normal, whereas others are bizarre (Figure 7-7, B).
Squamous cell carcinomas may occur anywhere in the oral cavity, but most tumors arise on the floor of the mouth, ventrolateral tongue, soft palate, and tonsillar pillar. The clinical appearance of squamous cell carcinoma occurring in several different locations may be seen in Figure 7-6.
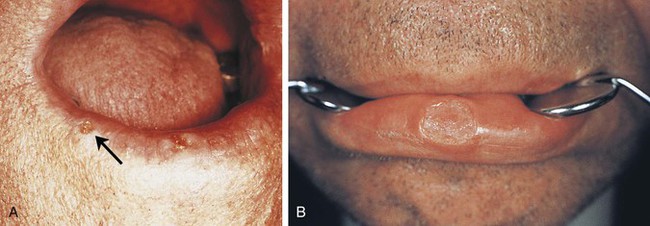
Squamous cell carcinomas may occur on the vermilion border of the lips and skin of the face (Figure 7-8). In this location they are associated with sun exposure (actinic cheilitis and actinic keratosis) and tend to be more common in individuals with fair skin. The prognosis for squamous cell carcinoma of the lips and skin is much better than that for squamous cell carcinoma of the oral mucosa. Sun exposure causes recognizable changes of the vermilion border of the lips. The color changes from dark and uniform to mottled grayish-pink. The interface of the vermilion border and the skin becomes blurred, and linear fissures are seen at right angles to the line of the interface. Microscopically, damage from ultraviolet rays as a result of sun exposure is seen as changes that range from degeneration of the collagen under the epithelium to a condition called solar or actinic cheilitis, in which mild-to-severe epithelial dysplasia occurs. Avoidance of sun exposure and the use of a sun-blocking agent are important in preventing the damaging effects of sunlight.
Risk Factors
Several risk factors have been associated with the development of squamous cell carcinoma. The most significant is tobacco—including cigar, pipe, and cigarette smoking; snuff dipping; and tobacco chewing. Alcohol consumption appears to add to the risk of oral squamous cell carcinoma, especially in individuals who also use tobacco products. High-risk types of human papillomavirus (HPV) have been identified in squamous cell carcinomas of the oropharynx and have been suggested to be important factors in the pathogenesis of these cancers… There is evidence that HPV contributes to the transformation of normal epithelial cells into malignant epithelial cells (HPV infection is discussed in Chapter 4). There is no evidence that chronic irritation (i.e., an ill-fitting denture) is an initiating factor in the development of oral cancer.
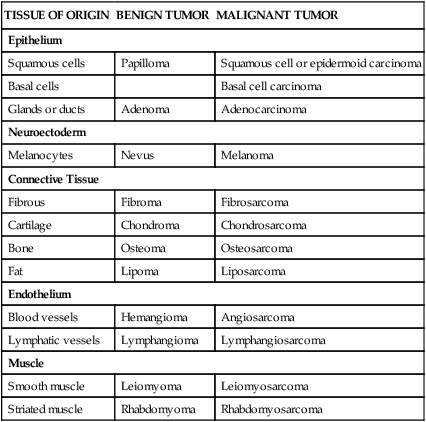
Treatment and Prognosis
Squamous cell carcinoma generally is treated by surgical excision. Radiation therapy or chemotherapy may be used in combination with surgery. On occasion, radiation therapy is used alone. The prognosis of squamous cell carcinoma is related to the size and location of the tumor and the presence or absence of metastases. The smaller the tumor is at the time of treatment, the better the prognosis. For oral squamous cell carcinoma, determining the size of the tumor and the presence or absence of cervical lymph node involvement and distant metastasis is important in predicting the patient’s prognosis. These are assessed using a system called the TNM staging system; the higher the stage, the worse the prognosis (Box 7-1 and Table 7-3). Metastasis to cervical lymph nodes is associated with a much poorer prognosis, as is the presence of distant metastasis. Therefore, it is important to clinically identify asymptomatic areas of leukoplakia and erythroplakia while they are small and to remove all potentially premalignant lesions.
TABLE 7-3
| STAGE | TUMOR | NODE | METASTASIS |
| I | T1 | N0 | M0 |
| II | T2 | N0 | M0 |
| III | T3 | N0 | M0 |
| T1 | N1 | M0 | |
| T2 | N1 | M0 | |
| T3 | N1 | M0 | |
| IV | T1 | N2 | M0 |
| T2 | N2 | M0 | |
| T3 | N2 | M0 | |
| T1 | N3 | M0 | |
| T2 | N3 | M0 | |
| T3 | N3 | M0 | |
| T4 | N0 | M0 | |
| Stage IV includes any patients with M1. | |||
Adapted from International Union against Cancer: TNM classification of malignant tumours (Sobin LH, Wittekind C, editors), ed 6, New York, 2002, Wiley-Liss.
Patients who have undergone radiation therapy for malignant tumors of the head and neck often experience severe xerostomia (dry mouth) as a result of radiation damage to the salivary gland tissue. These patients require preventive dental care consisting of nutritional counseling, topical fluoride application, and meticulous home care. Oral manifestations of therapy for oral cancer are included in Chapter 9.
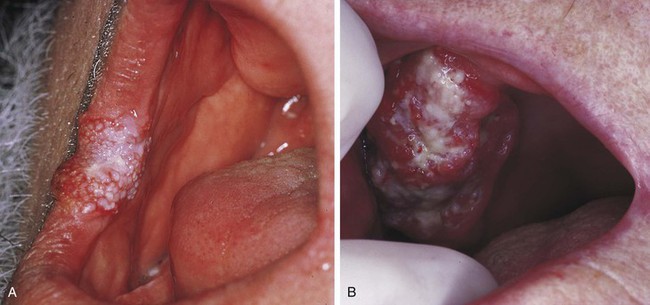
Verrucous Carcinoma
Verrucous carcinoma is a specific type of squamous cell carcinoma that is separated from other squamous cell carcinomas because it has a much better prognosis. Clinically, it appears as a slow-growing exophytic tumor with a pebbly white and red surface (Figure 7-9). Most cases occur in men over 55 years of age and involve the vestibule and buccal mucosa. The use of smokeless tobacco products has been associated with the development of verrucous carcinoma. Microscopic examination demonstrates a tumor composed of numerous papillary epithelial proliferations. The spaces between these papillary projections are filled with keratin (keratin plugging). The epithelium is well differentiated, does not contain atypical cells, and exhibits broad-based rete pegs that penetrate deeply into the connective tissue. The epithelial basement membrane is intact, and the tumor does not show invasion of tumor cells through the basement membrane, as is seen in squamous cell carcinoma.
Basal Cell Carcinoma
Basal cell carcinoma is a malignant skin tumor associated with sun exposure. This particular neoplasm does not occur in the oral cavity. Basal cell carcinoma frequently arises on the skin of the face and appears as a nonhealing ulcer with characteristic rolled borders (Figure 7-10). Most cases arise in white adults, and no sex predilection is seen.
Salivary Gland Tumors
Benign and malignant tumors may arise in either the major or minor salivary glands. Tumors may occur within the parotid, submandibular, or sublingual glands; or they may involve any of the minor salivary glands located throughout the oral cavity. Intraorally, minor salivary gland tumors are located most commonly at the junction of the hard and soft palates. They can also occur on the labial and buccal mucosa, the retromolar area, the floor of the mouth, and rarely the tongue (Figure 7-11). Tumors of minor salivary gland origin are much more common in the upper lip than in the lower lip.
Pleomorphic Adenoma (Benign Mixed Tumor)
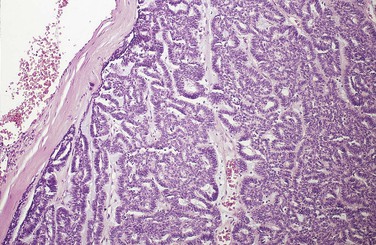
The pleomorphic adenoma is a benign salivary gland tumor. It is the most common salivary gland neoplasm and accounts for about 90% of all benign salivary gland tumors. Microscopic examination reveals an encapsulated tumor composed of tissue that appears to be a mixture of both epithelium and connective tissue (Figure 7-12). For this reason this tumor is often called a benign mixed tumor. The connective tissue–like part can vary from loose and dense fibrous connective tissue to cartilage. The tissue that looks like connective tissue is derived from a salivary gland cell called a myoepithelial cell.
The most common extraoral location for the pleomorphic adenoma is the parotid gland. The most common intraoral site is the palate. However, these tumors can occur wherever salivary gland tissue is present. Clinically, the pleomorphic adenoma appears as a slowly enlarging, nonulcerated, painless, dome-shaped mass (see Figure 7-11, A and C). The surface can be ulcerated if traumatized. Its size can range from a few to several centimeters. Most pleomorphic adenomas occur in individuals over 40 years of age, and a female predilection has been noted. Pleomorphic adenomas have also been reported in children.
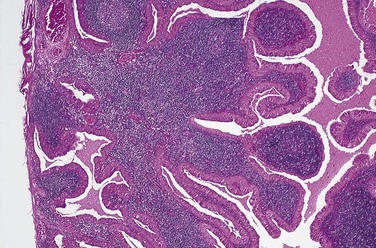
Monomorphic Adenomas
Monomorphic adenomas are benign encapsulated salivary gland tumors that occur less frequently than the pleomorphic adenoma. They are composed of a uniform pattern of epithelial cells (Figure 7-13). These tumors do not have the connective tissue–like component seen in a pleomorphic adenoma. Several specific types of monomorphic adenoma have been identified on the basis of their microscopic patterns. Trabecular adenoma and canalicular adenoma are monomorphic-type adenomas that are named for the microscopic pattern of the tumor. These tumors occur most commonly in adult women, with a predilection for the upper lip and buccal mucosa. A papillary cystadenoma lymphomatosum is another type of monomorphic adenoma. It is also called a Warthin tumor. Microscopic examination of this particular variant demonstrates an encapsulated tumor composed of two types of tissue: epithelial and lymphoid (Figure 7-14). The epithelial component is neoplastic. It lines papillary projections that protrude from cystic structures. Sheets of lymphocytes surround the cystic structures. In some cases the lymphoid component demonstrates germinal center formation. A Warthin tumor presents as a painless, soft, and compressible or fluctuant mass, usually located in the parotid gland. This tumor often develops bilaterally and occurs predominantly in adult men. Intraoral examples are very rare.
All monomorphic adenomas are treated by surgical excision. Recurrence is rare.
Mucoepidermoid Carcinoma
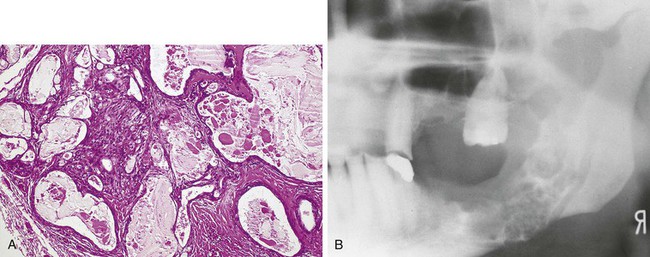
Mucoepidermoid carcinoma is a malignant salivary gland tumor. It is an unencapsulated, infiltrating tumor composed of a combination of mucous cells interspersed with squamous-like epithelial cells called epidermoid cells (Figure 7-15). Most studies show the mucoepidermoid carcinoma to be the most commonly occurring malignant salivary gland tumor of intraoral minor salivary gland origin.
Mucoepidermoid carcinomas involving the major glands occur most often in the parotid gland, whereas minor gland tumors are most common on the palate. They appear clinically as slowly enlarging masses (see Figure 7-11, D). On occasion, a mucoepidermoid carcinoma may arise centrally within bone (Figure 7-15, B), usually in the mandibular premolar and molar region. In this location it appears as either a unilocular or multilocular radiolucency (Figure 7-15, B). A central mucoepidermoid carcinoma is derived from either salivary gland tissue trapped within bone or the transformed epithelial lining of a dentigerous cyst (a developmental odontogenic cyst that forms around the crown of an unerupted or impacted tooth; see Chapter 5).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


 ) Characterized by a loss of differentiation of cells and their orientation to one another; a characteristic of malignant tumors.
) Characterized by a loss of differentiation of cells and their orientation to one another; a characteristic of malignant tumors. ) Fragments of abnormal immunoglobulins excreted in the urine of patients with multiple myeloma.
) Fragments of abnormal immunoglobulins excreted in the urine of patients with multiple myeloma. ) Surgical removal.
) Surgical removal. ) A protein, also called an antibody, synthesized by plasma cells in response to a specific antigen.
) A protein, also called an antibody, synthesized by plasma cells in response to a specific antigen. ) Clinical term used to identify a white, plaquelike lesion of the oral mucosa that cannot be wiped off or diagnosed as any other disease.
) Clinical term used to identify a white, plaquelike lesion of the oral mucosa that cannot be wiped off or diagnosed as any other disease. ) Cancer; a tumor that is resistant to treatment and may cause death; a tumor that has the potential for uncontrolled growth and dissemination or recurrence, or both.
) Cancer; a tumor that is resistant to treatment and may cause death; a tumor that has the potential for uncontrolled growth and dissemination or recurrence, or both. ) (plural, metastases [
) (plural, metastases [ ]) Transport of neoplastic cells to parts of the body remote from the primary tumor and the establishment of new tumors at those sites.
]) Transport of neoplastic cells to parts of the body remote from the primary tumor and the establishment of new tumors at those sites. ) Tumor formed by cells that have been transported from the primary tumor to sites not connected with the original tumor.
) Tumor formed by cells that have been transported from the primary tumor to sites not connected with the original tumor. ) A term, used in microscopy, to describe dividing cells caught in the process of mitosis (
) A term, used in microscopy, to describe dividing cells caught in the process of mitosis ( ).
). ) An elevation of a single type of immunoglobulin; detected by a process called immunoelectrophoresis.
) An elevation of a single type of immunoglobulin; detected by a process called immunoelectrophoresis. ) (plural, nevi [
) (plural, nevi [ ]) A benign tumor consisting of melanocytes (nevus cells); also a circumscribed, usually pigmented, congenital malformation of the skin or oral mucosa.
]) A benign tumor consisting of melanocytes (nevus cells); also a circumscribed, usually pigmented, congenital malformation of the skin or oral mucosa. ) Tooth forming.
) Tooth forming. ) Neoplasm; also, a swelling or enlargement.
) Neoplasm; also, a swelling or enlargement. ) Absence of normal differentiation; anaplasia; a characteristic of some malignant tumors.
) Absence of normal differentiation; anaplasia; a characteristic of some malignant tumors. ) A ring of lymphatic tissue formed by the two palatine tonsils, the pharyngeal tonsil, the lingual tonsil, and intervening lymphoid tissue.
) A ring of lymphatic tissue formed by the two palatine tonsils, the pharyngeal tonsil, the lingual tonsil, and intervening lymphoid tissue.