Nonneoplastic Diseases of Bone
Anne Cale Jones, Joan Andersen Phelan, Olga A.C. Ibsen and John E. Kacher
After studying this chapter, the student will be able to:
1. Define benign fibro-osseous lesion.
2. Define dysplasia as it relates to bone diseases and differentiate the term from epithelial dysplasia.
3. List the benign fibro-osseous lesions that occur in the jawbones.
4. Describe the clinical, radiographic, and microscopic features of periapical cemento-osseous dysplasia, focal cemento-osseous dysplasia, and florid cemento-osseous dysplasia.
5. Compare and contrast periapical cemento-osseous dysplasia, focal cemento-osseous dysplasia, and florid cemento-osseous dysplasia.
6. Compare and contrast monostotic fibrous dysplasia with polyostotic fibrous dysplasia.
7. Compare and contrast the radiographic appearance, microscopic appearance, and treatment of fibrous dysplasia of the jaws with those of ossifying fibroma of the jaws.
8. Compare and contrast the three types of polyostotic fibrous dysplasia.
9. Describe the microscopic appearance of Paget disease of bone and describe its clinical and radiographic appearance when the maxilla or mandible is involved.
10. Describe the clinical, radiographic, and microscopic features of central giant cell granuloma and aneurysmal bone cyst.
Café au lait ( ) Refers to a macular skin pigmentation that is the color of coffee with milk.
) Refers to a macular skin pigmentation that is the color of coffee with milk.
Dysplasia ( ) Disordered growth; abnormal development.
) Disordered growth; abnormal development.
Neoplasia ( ) New growth; the formation of tumors by the uncontrolled proliferation of cells.
) New growth; the formation of tumors by the uncontrolled proliferation of cells.
Neoplastic ( ) Pertaining to the formation of tumors by the uncontrolled proliferation of cells.
) Pertaining to the formation of tumors by the uncontrolled proliferation of cells.
Nonneoplastic diseases of bone that affect the maxilla and mandible fall into multiple categories. Inherited diseases that affect bone are discussed in Chapter 6, and benign and malignant neoplasms of bone are discussed in Chapter 7. The purpose of this chapter is to delineate several other nonneoplastic diseases of bone that are important for a dental hygienist to understand but are not covered elsewhere in this text. These include three forms of cemento-osseous dysplasia: (1) periapical, (2) florid, and (3) focal. In addition, the dental hygienist should also be familiar with the various types of fibrous dysplasia and the clinical and radiographic features of Paget disease, central giant cell granuloma, aneurysmal bone cyst, and osteomalacia.
Benign Fibro-Osseous Lesions
Benign fibro-osseous lesions that affect the maxilla and mandible include central and peripheral cementifying and ossifying fibromas, periapical cemento-osseous dysplasia, florid cemento-osseous dysplasia, focal cemento-osseous dysplasia, and fibrous dysplasia (Box 8-1).
Periapical Cemento-Osseous Dysplasia
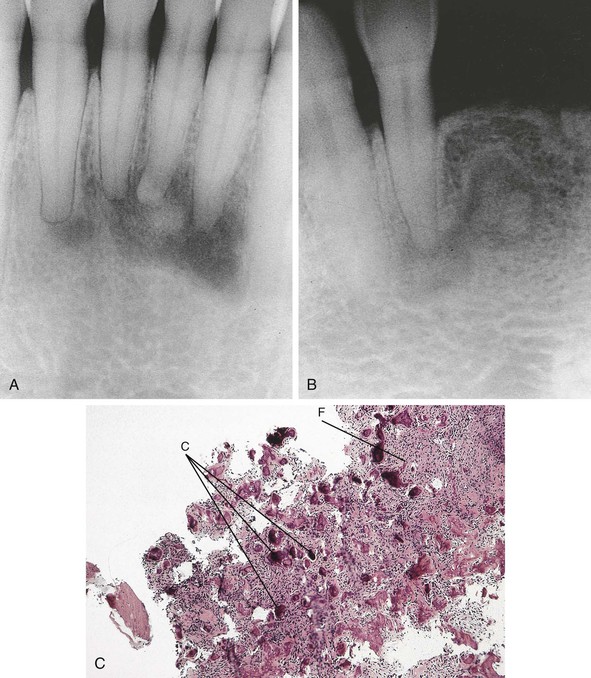
Periapical cemento-osseous dysplasia is a relatively common disease of unknown cause that affects periapical bone (Figure 8-1, A and B). The term cementoma was used in the past for this disease. However, because the disease does not represent a neoplasm, this term is inappropriate and should be avoided.
The diagnosis of periapical cemento-osseous dysplasia is usually established on the basis of its characteristic clinical and radiographic features. Historical and clinical information and radiographic appearance are both important in establishing the diagnosis. Pulp testing confirms that teeth are vital. A biopsy may be necessary in cases in which the characteristic radiographic features are not evident. Microscopic examination reveals a fibro-osseous lesion. Like other fibro-osseous lesions, periapical cemento-osseous dysplasia is composed of a combination of fibrous tissue and calcifications. The calcifications in this lesion may resemble bone, cementum, or both. Early lesions consist mainly of fibrous tissue, whereas long-standing lesions contain fibrous connective tissue interspersed with numerous calcifications (Figure 8-1, C). If a patient demonstrates radiographic changes characteristic of an early lesion, follow-up examinations may be necessary to ensure that a correct diagnosis was established. Once the condition is recognized, no treatment is necessary. The lesion remains asymptomatic and localized.
Florid Cemento-Osseous Dysplasia
Florid cemento-osseous dysplasia occurs most often in black women older than 40 years of age. The cause of this disease is unknown. Radiographically, it differs in location from periapical cemento-osseous dysplasia in that it typically affects more than one quadrant of the maxilla and mandible, often in the posterior areas. On occasion, an early radiolucent phase similar to that seen in periapical cemento-osseous dysplasia may be identified. However, the majority of cases present as radiopaque masses of irregular opacification (Figure 8-2). There is usually no bone expansion.
Fibrous Dysplasia
Types of Fibrous Dysplasia
Polyostotic Fibrous Dysplasia
Clinical examination reveals a painless enlargement of the affected bone or bones. Jaw involvement typically appears as a painless, progressive, unilateral enlargement of the maxilla or mandible. When fibrous dysplasia involves the maxilla, the disease usually extends into the maxillary sinuses. Involvement of the jaws may occur in any type of fibrous dysplasia. The classic radiographic appearance of fibrous dysplasia is a diffuse radiopacity that is described as resembling “ground glass” (Figure 8-3, A). The abnormal bone blends into the adjacent normal bone, making it difficult to determine the periphery of the lesion. A patchy radiolucency with central opacifications and a dense radiopacity have also been observed in fibrous dysplasia. The radiolucent or radiopaque appearance of fibrous dysplasia depends o/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


 ) Benign lesion of bone characterized microscopically by cellular fibrous connective tissue admixed with irregularly shaped bone trabeculae or cementoid material.
) Benign lesion of bone characterized microscopically by cellular fibrous connective tissue admixed with irregularly shaped bone trabeculae or cementoid material. ) Not neoplastic.
) Not neoplastic.