Chapter 7
Management of Periodontal Diseases
Aim
This chapter aims to consider the current classification of periodontal diseases; review best practice for screening and diagnosis of periodontal diseases; and give an overview of the periodontal therapy falling within the remit of a competent GDP.
Outcome
Having read this chapter the reader will be familiar with the screening, diagnosis and initial management of periodontal diseases in a general dental practice environment and be able to identify patients who would benefit from referral to a specialist.
The Role of the General Dental Practitioner
The GDP is the major provider of primary dental care and has a significant role in oral health education, screening to detect periodontal disease and following diagnosis to arrange appropriate care.
The dentist can coordinate and encourage a preventive approach to dental health throughout the practice, in the recognition that all members of the dental team can influence a patient’s periodontal health. For example, every member of staff can and should encourage and support patients in smoking cessation. Dental nurses with an Oral Health Educator Certificate can manage Preventive Dental Units and assist individual patients to develop and maintain good oral hygiene. The success and stability of almost every aspect of dental care is dependent upon establishing a high standard of plaque control.
The dental hygienist has additional skills appropriate to the provision of an effective non-surgical course of periodontal therapy. The majority of periodontal disease is of a chronic form and only 8% of dentate adults in the UK have loss of attachment of 6 mm or more. Thus, the number of patients requiring complex specialist treatment is low and the delegation of initial non-surgical periodontal care to a dental hygienist is appropriate due to the high quality and reduced cost of treatment. The role of the hygienist in long-term maintenance of periodontal health has been well documented. Studies of the long-term outcome of periodontal treatment have demonstrated convincingly that maintenance of a high standard of oral hygiene prevents or at least reduces the progression of periodontal diseases.
In the provision of restorative dental care (Chapter 10) the dentist should work closely with the dental technician to ensure that both fixed and removable prostheses are designed and constructed to facilitate oral hygiene and avoid occlusal trauma to the remaining teeth (Chapter 9). Thus, there are relatively few periodontal patients who cannot be treated and maintained to high standards within the confines of a general dental practice and the whole dental team has a role to play in the prevention of periodontal disease.
Periodontal disease in its early stages causes few, if any, symptoms and patients are often unaware that they have a problem. It is therefore the duty of the GDP to monitor and screen patients for the presence of periodontal diseases. Where clinical findings indicate disease, relevant radiographs should be obtained. The practitioner should, following diagnosis, develop a treatment plan with specified therapeutic outcomes.
The long-term outcome of periodontal therapy is dependent upon patient compliance. It should be recognised that not all patients will be psychologically or physically capable of complying with the optimal standard of oral hygiene and some may even decline therapy. Nevertheless, all patients have the right to make an informed choice in relation to periodontal management.
All periodontal assessments should be recorded in the clinical notes. In particular probing pocket depths, clinical attachment levels, bleeding sites, plaque scores and mobility should be recorded. All clinically successful modalities of periodontal therapy include the substantial reduction of subgingival plaque. The outcome of periodontal therapy should be assessed in relation to patient comfort and aesthetics. Once periodontal stability has been achieved it is essential to arrange a supportive care programme.
Clinical Guidelines for Screening
Periodontal diseases can occur in any patient regardless of age. It is therefore vital to perform a periodontal screening examination for all patients at regular intervals. An assessment of each individual patient’s “risk” of developing periodontal disease will influence the frequency of maintenance. The British Society of Periodontology and the Faculty of General Dental Practitioners of the Royal College of Surgeons of England have both produced clinical guidelines recommending routine screening for periodontal disease.
The Basic Periodontal Examination (BPE) is the recommended screening method. The use of BPE is an essential feature in orthodontic and complex restorative treatment planning. The benefits and limitations of the BPE are detailed in the first book of the Quintessentials series (Chapple and Gilbert 2002). The BPE codes and their relevance to periodontal treatment needs are shown in Table 7-1 and Fig 7-1.
| BPECode | Clinical status | Treatment needs | |
| 0 | Coloured band is completely visible no calculus no gingival bleeding | Healthy periodontium | Repeat screening. |
| 1 | Coloured band is completely visible no calculus plaque and gingival bleeding | Gingivitis | Oral hygiene instruction. |
| 2 | Calculus supra- and or Gingivitis subgingival, iatrogenic plaque retention factors (prfs), no pockets >3 mm coloured band completely visible | Oral hygiene instruction, scaling, remove plaque retention factors. | |
| 3 | Coloured area of the probe remains partly visible in the deepest pocket in the sextant | Periodontitis, shallow pocketing 5 mm or less | Non-surgical periodontal care within remit of general dental practitioner. |
| 4 | Coloured area of probe completely disappears | Periodontitis, deep pockets ≥ 5.5 mm | May require complex specialist periodontal care. |
| * | Annotates other codes | Furcation involvement or attachment loss exceeding 7 mm in total | Signifies poor prognosis. Consider specialist opinion. |
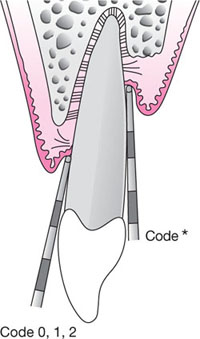
Fig 7-1a Line diagram illustrating the BPE coding system 0, 1, 2 + *.
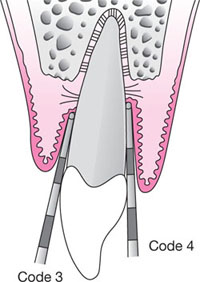
Fig 7-1b Diagram illustrating the BPE coding system for codes 3 and 4.
Table 7-2 summarises the recommendations for radiographic examination of patients when clinical examination reveals the presence of periodontal disease. A variety of panoramic radiographic equipment is available. Panoramic films are of use only when good quality imaging of the anterior sextants can be achieved.
Diagnosis
Screening using the BPE can highlight the presence of periodontal disease, but a detailed history and examination are required to reach a diagnosis and formulate a detailed treatment plan. These topics are detailed in Chapple and Gilbert 2002. A periodontal examination should include:
-
Standard of oral hygiene, location and quantity of plaque and calculus deposits.
-
Note of plaque retention factors.
-
Assessment of the gingiva for signs of inflammation, recession and hyperplasia.
-
Periodontal probing, recording probing pocket depths, bleeding on probing and suppuration.
-
Location of furcation defects.
-
Presence and degree of tooth mobility.
-
Occlusal assessment to include static and dynamic function, wear faceting and premature contacts.
-
Oral mucosal assessment for signs of systemic diseases.
-
Radiographic examination (see Table 7-2).
| Disease | Distribution | Severity | Radiograph |
| Gingivitis | None | ||
| Periodontitis | generalised | mild (LOA ≤ 3mm) | DPT |
| moderate (LOA >3mm but <5mm) | DPT and supplemental films of localised areas (e.g. furcation involvements) using PAs or vertical bitewings | ||
| severe (LOA >5mm) | periapicals of standing teeth or DPT if considering clearance | ||
| Periodontitis | localised – posterior teeth only affected | mild | horizontal bitewings |
| moderate | vertical bitewings | ||
| severe | periapicals of affected teeth or DPT initially ± supplemental PAs | ||
| Periodontitis | localised – anterior teeth only affected | mild | periapicals of affected teeth or DPT initially ± supplemental PAs |
| moderate | as above | ||
| severe | as above | ||
| Periodontitis | localised involving anterior and posterior teeth | mild | DPT |
| moderate | DPT initially ± vertical bitewings for posteriors ± PAs for anterior teeth | ||
| severe | periapicals of standing teeth or DPT initially ± supplemental PAs |
LOA = loss of attachment; DPT = dental pantomograph; PA = periapical x-ray
Classification of periodontal diseases
The classification of periodontal diseases is complex. In addition to thorough clinical examination, a detailed social, medical and family history should be obtained to assist diagnosis. The most recent classification resulting from the 1999 Illinois International Workshop for the Classification of Periodontal Diseases and Conditions is summarised in Table 7-3. A detailed appraisal of this system is discussed in Chapple and Gilbert 2002.
| Gingival diseases | |
| Dental plaque-induced gingival diseases | Gingivitis associated with dental plaque only Gingival diseases modified by systemic factors Gingival diseases modified by medications Gingival diseases modified by malnutrition |
| Non-plaque-induced gingival lesions | Gingival diseases of specific bacterial origin Gingival diseases of viral origin Gingival diseases of fungal origin Gingival lesions of genetic origin Gingival manifestations of systemic conditions Traumatic lesions Foreign body reactions Not otherwise specified (NOS) |
| Periodontal diseases | |
| Chronic periodontitis | Localised Generalised |
| Aggressive periodontitis | Localised Generalised |
| Necrotising periodontal diseases | Necrotising ulcerative gingivitis Necrotising ulcerative periodontitis Abscesses of the periodontium |
| Periodontitis associated with endodontic lesions | |
| Developmental or acquired deformities and conditions | |
| Periodontitis as a manifestation of systemic diseases | Haematological disorders Genetic disorders Not otherwise specified (NOS) |
This classification attempts to relate disease to differing aetiologies, prognosis and treatment modalities. The difference between chronic (Fig 7-2) and aggressive (Fig 7-3) forms of periodontitis are summarised in Table 7-4 and Table 7-5 gives details of the differences between periodontal and periapical abscesses. It is important to note that there is no indication to use systemic antimicrobial drugs in the management of chronic periodontitis, but they do have a role in the management of aggressive disease. It is not the remit of this book to discuss the clinical management of the most common periodontal diseases; this will be covered in the third book of the present series, Successful Periodontal Therapy: A Non-Surgical Approach.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


