Chapter 7
I’ve Got a Grating Joint
Mrs Smith is a patient whom you have known for several years. She has attended for routine examinations; she wears partial upper and lower acrylic dentures that are old and worn and have poor occlusion. She is missing most of her posterior teeth in both arches. Her dentures are several years old and she is now lacking posterior support. She is 67 years of age and, although you have encouraged her in the past to get new dentures, she wishes to continue with the ones that she has because she feels that she is too old to adapt to something new.
She has attended for her 6-monthly examination and mentions to you in passing that she has discomfort in her left ear. She said that she has had a crunching or grating noise in her ear when she moves her jaw for 4 or 5 years but she has recently become aware of discomfort. She feels that her mouth opening is restricted; she has no pain on waking, but feels that her discomfort comes on with function and gets worse as the day goes on. She says that her jaw feels ‘heavy’. She does not get headaches and says that the pain is located to the area immediately in front of her ear and ‘is in my ear’. She has osteoarthrosis and is awaiting admission to hospital for a hip replacement. She has also recently been diagnosed with breast cancer and has had a general anaesthetic for a lumpectomy. The pathology has been reported as being a benign lump. She had a mastectomy 12 years ago and underwent a course of radiotherapy and chemotherapy. She is taking tamoxifen and an antidepressant. She is a retired teacher.
Examination
She has a class II, division I, basal bone and incisal relationship. She has an overjet of 6 mm and she is now aware of having to posture her jaw forwards to be able to chew but this is uncomfortable. She feels that she has a restricted range of movement, only being able to open comfortably to two finger widths. You measured this as 25 mm. The left TMJ is tender on lateral and intra-auricular palpation. You examined the temporalis and masseter muscles digitally and the lateral pterygoid muscles against resistance. She has no obvious masticatory muscle tenderness. Even without the use of a stethoscope you were able to hear a crepitation or grating noise from her left TMJ when she opened her mouth widely. Mrs Smith reported that she felt that her bite had changed somewhat but you are unable to detect any significant occlusal abnormalities because of the poor occlusion of her dentures. This was also because she was very ‘hand shy’, as she did not want you to palpate her TMJ, and because she could not comfortably move her mandible from side to side. You found it very difficult to establish her centric jaw relationship.
She was very anxious about her symptoms because of her previous history of breast cancer as she felt that she might have a tumour. She insisted on you referring her for a radiograph.

Although you would not normally have required a radiograph, you agreed to do so in this instance because there was good reason to allay her very obvious anxiety and, in the circumstances, you felt that this test was justifiable.
Radiographic Examination
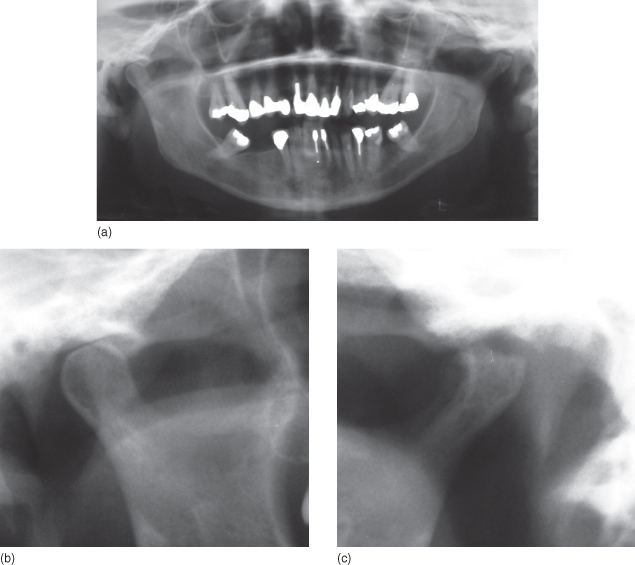
You requested a DPT. This showed a normal outline of the mandibular condyle on the right side but showed loss of the condylar outline of the mandibular condyle on the left side and sclerosis of the articular fossa (Figure 7.1).
Figure 7.1 (a) Dental panoramic tomogram; (b) close-up of normal joint right; (c) close-up of degenerative joint disease left.
Diagnosis
Your diagnosis was osteoarthrosis in the TMJ on the left side.
Treatment
It is suggested the natural history and progress of osteoarthrosis from the first clinical sign to the final subsidence of pain and stiffness, if untreated, can vary from 1 year to 3 years but on occasion the condition may take longer to stabilise and symptoms to improve. Simple symptomatic treatment gives encouragement and makes the disease more tolerable for the patient. Most patients with osteoarthrosis of the TMJ do not appear to have significant problems; it is mainly acute exacerbations and reduced range of movement that necessitate active intervention. In Mrs Smith’s case she was aware of the crepitation which had been present for years. This did not concern her, and you and she had talked about it before. What was new, however, was the discomfort and difficulty with chewing. These were her immediate concerns.
Explanation and Reassurance 
Patients are encouraged by the fact that this disease often improves spontaneously as the TMJ retains the capacity to repair and remodel throughout life. It should be explained that symptoms may worsen before they improve. A useful way of illustrating this is to draw a graph or curve which will assist in explaining the prognosis of the condition (Figure 7.2).
Figure 7.2 Diagrammatic presentation of the progress of osteoarthrosis symptoms.
(Reprinted from Ogus MD, Toller P. Common Disorders of the Temporomandibular Joint. Bristol: John Wright & Sons Ltd, 1981, with permission; © 1981.)
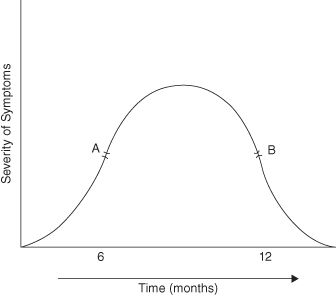
It is conceded that at the time of consultation it may be difficult to assess the patient’s precise position on the curve. Therefore if the current stage is at point A, a period of deterioration will precede improvement. If on the other hand it is at point B, th/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


