Esthetic Management of the Dentogingival Unit
Claude R. Rufenacht
The preservation of a healthy periodontal attachment is a prerequisite for successful restorative procedures. It has been demonstrated that margin placement, fit of restoration, restorative material, emergence profile, and tooth contour are factors that may contribute to the disturbance of this state of health.1–5Even the best clinician must face postinsertion gingival inflammation as a consequence of an overlooked evaluation of the clinical situation or as a result of faulty clinical procedures.
Sound knowledge of the normal anatomy of the dentogingival unit should be present if the clinician wants to avoid violating the conditions necessary for maintaining health or jeopardizing the physiologic and esthetic result of any restorative procedure.
The dentogingival unit is composed of two parts: (1) the connective fibrous tissue attachment, and (2) the epithelial attachment or junctional epithelium.6,7
In a study that involved 325 measurements taken from clinically normal specimens, it has been established8 that there is some form of proportional dimensional relationship among the crest of the alveolar bone, the connective tissue attachment, and the junctional epithelium, as well as a repetitive consistency in these proportions.
It has been shown (Fig 7-1) that the sulcus depth averages 0.69 mm, the junctional epithelium averages 0.97 mm, and the connective fibrous tissue attachment averages 1.07 mm. Of these three tissue components the supracrestal connective fibrous attachment seems to exhibit the least variability. The combined dimension of the connective tissue attachment and the junctional epithelium reaches 2.04 mm and is referred to as the biologic width. The biologic width appears to exist in any periodontium, and the importance of not violating this physiologic dimension was suggested by Ochsenbein and Ross9 and stressed by other authors.1,10–12 When margin placement impinges into the biologic width, inflammation and bleeding cannot be avoided; as a result, a loss of attachment with apical migration of the junctional epithelium and periodontal pocket formation occurs.
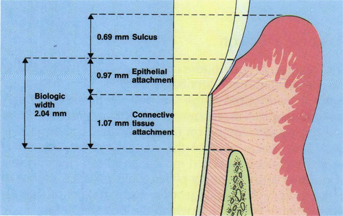
Fig 7-1 This diagrammatic representation has been progressively developed by the studies of a number of authors. It describes the dimensions and relations of the different elements of the dentogingival unit. It should be impressed and visualized whenever clinical practice reaches the gingival level.
The location of the bottom of the gingival attachment at the cementoenamel junction (CEJ) is considered by many a transitional stage. As age progresses the epithelium is apt to proliferate in an apical direction. In so doing it establishes a firm union with the cemental surface. The apical shift of the dentogingival junction is termed passive eruption (Figs 7-2 and 7-3). This concept of passive eruption as a physiologic process seems to derive mainly from microscopic examination of human teeth at different ages, in which the bottom of the sulcus is visualized at different levels below the CEJ. It may be that passive eruption or the apical shift of the gingivo-epithelial junction is not a physiologic process. This could be explained by considering the fact that nearly all civilized adults have had a history of acute or chronic tissue inflammation, with a concomitant destruction of the connective fibrous attachment. The clinical picture is then characterized by the recession of the gingival margin or the retention of the original level and a deepening of the pocket.
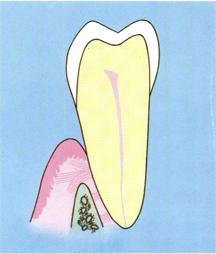
Fig 7-2 Passive eruption describes the apical shift of the gingival attachment along the root surface.

Fig 7-3 Clinical view of a passive eruption that is held by many as the result of successive chronic or acute inflammatory processes.
Many adults exhibit short anatomic crowns with gingival tissue located occlusally or incisally. As opposed to passive eruption, this clinical situation is referred to as delayed passive eruption in which the junctional epithelium did not migrate apically and remains along the convexity of the anatomic crown, giving the impression of a transitional stage in the phase of a normal tooth eruption. Lip, tongue, and muscle interferences have been suggested among the reasons that prevent teeth from exhibiting a normal and total eruption. In a healthy state, the gingival margin is generally located on the enamel and the junctional epithelium from the base of the sulcus to the CEJ, and the gingival fiber apparatus takes place between the osseous crest and the CEJ.13 The mucogingival junction is considered in a normal location when positioned either coronal or apical to the crest of the bone. A more precise classification, based on histologic findings of clinical situations in the adult exhibiting deviations from this normality, has been proposed.14
With reference to the norm, an excessive amount of gingival tissue or an inadequate position of the osseous crest related to the CEJ can be stated. These types of situations that have been also named altered passive eruption can be evaluated according to the following factors:
1. Location of the mucogingival junction.
2. Location of the gingival margin.
3. Location of the CEJ.
4. Location of the osseous crest.
This approach will enable the clinician to evaluate the situation and to adopt the appropriate method of treatment, limited to gingival and mucogingival procedures or extended to osseous surgical procedures (Figs 7-4 to 7-7).
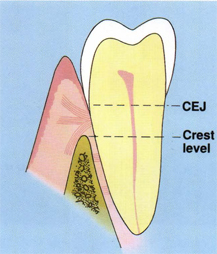
Fig 7-4 Differential diagnosis of delayed tooth eruption. An excessive amount of gingiva covering in the occlusal direction of the anatomic crown can be noted. The mucogingival junction is apical to the alveolar crest. (From Coslet et al.14)
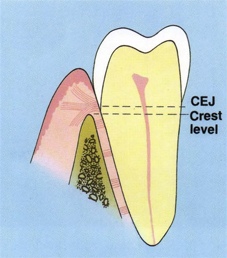
Fig 7-5 Differential diagnosis of delayed tooth eruption. The alveolar crest is situated at the level of the cementoenamel junction and the mucogingival junction apical to the alveolar crest. (From Coslet et al.14)
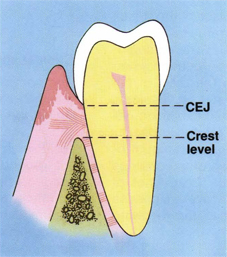
Fig 7-6 Differential diagnosis of delayed tooth eruption. The mucogingival junction is situated at a level coronal to the alveolar crest, and the anatomic relationships existing between the other elements appear normal. (From Coslet et al.14).
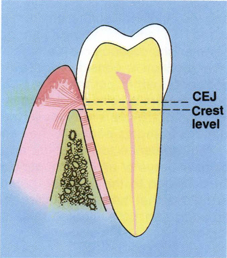
Fig 7-7 Differential diagnosis of delayed tooth eruption. The position of cementoenamel junction relative to the alveolar crest does not allow the normal insertion of the connective tissue attachment. The mucogingival junction is located coronal or at the level of the alveolar crest. (From Coslet et al.14)
Clinical situations
The complexity of the necessary clinical and technical steps to routinely construct restorations without damaging the healthy periodontium should give credit to those who advise supragingival margin placement of restoration.15,16–18However, daily practice does not allow for routine supragingival margin placement, which is judged esthetically unacceptable in the anterior area19 or inadequate in the posterior area when dealing with reduced crown height where emphasis should be put on mechanical retentions. Intrasulcular margin placement must be accepted as inevitable. In modern dentistry appropriate management of these factors with respect to the environment has been widely described. Healthy gingival tissue surrounding dental elements or dental restoration is part of structural beauty, and a protocol of treatment to maintain this state will be proposed in chapter 10. Unfortunately, proper intrasulcular margin placement is often impossible because of the deep location of caries and previous overzealous tooth preparations. The same impossibility can be stated regarding clinical situations exhibiting high located horizontal root fractures or endodontic perforation (Figs 7-8 and 7-9).

Fig 7-8 Subgingival root fracture. This clinical situation presents, on the buccal level, similarities to that described in Fig 7-5, and suggests treatment possibilities.

Fig 7-9 Clinical situation following minimal tooth lengthening by means of forced eruption with fiber resection. This procedure made possible margin placement without violating the biological width.
Tooth maintenance does not leave any alternative for treatment other than lengthening the dental element to expose sufficient sound tooth structure coronally to the junctional epithelium for proper placement of the margin of the restoration.
To />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


