CHAPTER 62
Nerve Repair
Andrew B.G. Tay1 and John R. Zuniga2
1Department of Oral and Maxillofacial Surgery, National Dental Centre, Singapore
2Department of Oral and Maxillofacial Surgery, Southwest Medical Center, Dallas, Texas, USA
Procedure: Trigeminal Nerve Repair
A method of exploring and repairing significant injuries (Sunderland IV to V degree injuries) to injured trigeminal nerve branches: the inferior alveolar nerve (IAN), the lingual nerve (LN), and the infraorbital nerve (ION).
Indications
- Witnessed nerve injury: Partial– or full-diameter nerve damage on direct visual inspection during surgery (including third molar surgery, orthognathic surgery, surgery for maxillofacial trauma, implant surgery, and pathology surgery). Repair at the earliest opportunity under microscopic magnification by a trained microsurgeon offers the best outcomes.
- Primary repair (immediate) is undertaken if conditions are favorable and there is access, microsurgical expertise, facilities, and time available
- Delayed primary repair (3–7 days) may be undertaken if the wound is contaminated or if the patient’s condition, lack of microsurgical expertise, or facilities do not permit immediate repair
- Secondary repair (more than 1 week) may be undertaken if there is no improvement in clinical neurosensory testing
- Nerve injury with evidence of encroachment or disruption of the nerve canal (mandibular and infraorbital) on imaging (computed tomography [CT] or cone beam CT).
- Nonwitnessed nerve injury: Loss or alteration of sensation in the nerve distribution after trauma or injury, without visual evidence of damage but confirmed Sunderland IV or V degree injury by clinical neurosensory testing or adjunctive testing (magnetic resonance neurography, trigeminal nerve conduction, etc.).
- Nerve injury with neuropathic pain: Evidenced by a history of spontaneous or stimulus-evoked burning pain or neuralgic pain in the nerve distribution, with or without allodynia, hyperpathia, or hyperalgesia confirmed by neuropathic pain testing.
- Chemical nerve injury: Caustic agents have damaged the nerve (i.e., endodontic irrigation of socket in close proximity to the IAN).
Contraindications
- Nerve injury with mild or improving sensory loss or with only partial involvement of the nerve distribution
- Nerve injuries with mild or moderate sensory impairment by clinical neurosensory testing and with no evidence of nerve encroachment or disruption on imaging
- Nerve injury in the context of life-threatening or more critical injuries, or in unfavorable situations (e.g., a contaminated wound, an unfit patient, or microsurgical expertise or facilities unavailable) for which delayed or secondary nerve repair would be reasonable
- Nerve injury resulting from local anesthetic injections
- Neuropathic pain of central trigeminal origin or sympathetically mediated pain source
- Patient refusal to undergo nerve exploration and repair
Nonsurgical Management
- Nonsurgical treatment options for nonpainful nerve injuries include observation, medical therapy in the early post-injury phase (e.g., vitamin B complex and steroids), and/or sensory retraining.
- Nonsurgical treatment options for nerve injuries with neuropathic pain include medication (i.e., Gabapentin, Clonazepam, and Amitriptyline), therapeutic nerve blocks, physical therapy (i.e., TENS), and/or behavioral therapy.
Anatomy
- Lingual nerve (LN): The LN is a branch of the mandibular division of the trigeminal nerve and descends between the medial pterygoid muscle and the ramus of the mandible. It is joined by the chorda tympani, a branch from the facial nerve, and 2 cm below the skull base. The chorda tympani carries taste fibers of the anterior two-thirds of the tongue. The LN lies anterior to the IAN and may be located at a variable height from the crest of the mandible (−2 mm to 7 mm). The LN may be located above the lingual plate in 10–17.6% of cases. The LN may be in contact with the surface of the lingual cortex (22.3–62%) a maximum horizontal distance of 7 mm. The LN crosses the lateral surface of the hypoglossus muscle and passes deep to the mylohyoid muscle. It lies superior to the submandibular duct and then crosses downward along the lateral aspect of the duct to turn up along its medial side, on the genioglossus muscle. The LN supplies the tongue as it travels forward along its side. The LN is mono- or oligofascicular proximal to the point where the chorda tympani joins it, and it becomes polyfascicular near the submandibular ganglion. Its fascicular pattern changes every 126 mm on average from this point forward. The LN supplies sensation to the dorsum, lateral and ventral surfaces of the anterior two-thirds of the ipsilateral half of the tongue, mucous membrane of the ipsilateral floor of the mouth, and lingual gingivae of the mandibular teeth.
- Inferior alveolar nerve (IAN): The IAN is a branch of the trigeminal mandibular division and descends below the lateral pterygoid muscle curving on the medial pterygoid muscle, to run between the sphenomandibular ligament and mandibular ramus, and to enter the mandibular foramen. The IAN gives off the mylohyoid branch at the mandibular foramen. The IAN travels with the inferior alveolar artery and vein within the mandibular canal, which descends and proceeds anteriorly in a concave curve and ascends to the mental foramen. The mandibular canal wall has a diameter of 2.0 to 2.4 mm and thins near the mental foramen in 60% to 80% of patients. The mandibular canal is located higher in the mandible in patients younger than 20 years of age and older than 60 years; it is, in order of vertical proximity, closest to the roots of the mandibular third molar, then the second molar, then the first molar, and furthest from the second premolar. The horizontal distance of the canal from the buccal cortex, in descending order, is the second mandibular molar, the first molar, and the third molar and second premolar. The mandibular canal curves superiorly and posterior-laterally to reach the mental foramen. The mental foramen is typically located at a third of the height of the mandible from the inferior border, and mesiodistally at the second or first premolar. Just before the mental foramen, the IAN branches into the incisive branch, which continues anteriorly under the apices of the incisors, and the mental nerve, which exits the mental foramen to enter the soft tissue as 1–4 branches (mean 2 branches) at an angle of 36° to the fibers of the orbicularis oris muscle. The IAN tends to be polyfascicular with a decreasing number of fascicles more distally; the fascicular pattern changes every 2 mm. The IAN supplies the ipsilateral lower lip (vermilion, skin, and mucosa), the chin, the labial-buccal alveolar mucosa from the midline to the molar region, and the ipsilateral teeth, with some midline crossover in 31% of cases.
- Infraorbital nerve (ION): The ION is a branch of the maxillary division of the trigeminal nerve and enters the orbit through the inferior orbital fissure to progress forward with the infraorbital artery in the infraorbital groove, infraorbital canal, and infraorbital foramen. The infraorbital foramen is located roughly 8 mm (range 6.2– 10.7 mm) below the infraorbital rim and is most commonly located in the same vertical plane as the first maxillary premolar. The foramen has a mean diameter of 4.5 mm (range 1–7 mm) and may present as multiple foramina (2–4) in 15% of cases. The ION exits the infraorbital foramen to lie between the levator labii superioris and the levator anguli oris muscles. Outside the foramen, the ION divides into several branches, including the inferior palpebral branches supplying the lower eyelid and cheek, the nasal branches supplying the lateral aspect and alar of the nose, and the superior labial branches supplying the upper lip and labial-buccal gingivae from the midline to the second premolar. While in the infraorbital canal, the ION gives off the anterior and middle superior alveolar branches that supply the maxillary incisors, canines, and premolars.
Surgical Technique for Trigeminal Nerve Repair
- The patient is positioned supine. The surgical table is positioned to allow two surgeons to site on either side of the patient’s head with an operating microscope (two operator eyepieces, microscope focal distance at 250 mm) over the patient’s head.
- General anesthesia via nasal endotracheal intubation with the tube pointing toward the patient’s forehead. A throat pack should be placed.
- For lingual nerve repair, a sandbag is placed under the patient’s shoulders to elevate the mandible.
- The skin and oral cavity are prepped, and local anesthetic containing epinephrine is injected within the operation site for pain control and hemostasis.
Lingual Nerve Repair
Access Phase
- The operating surgeon sits on the same side as the operation site.
- A modified Dingman mouth gag is utilized to position the mouth open, using the tongue blade to keep the tongue away from the operative site (Figure 62.1).
- An intraoral mucosal incision is initiated with a No. 15 Bard–Parker scalpel over the ascending ramus to the distal of the mandibular second molar. A buccal extension from the distal of the molar to the buccal sulcus and a lingual extension to the lingual sulcus curving forward to the mandibular first molar are made. The buccal and lingual supraperiosteal flaps are raised with a periosteal elevator and Metzenbaum curved dissecting scissors. The flaps are secured to the modified Dingman frame with 3-0 or 4-0 black silk sutures (Figure 62.2).
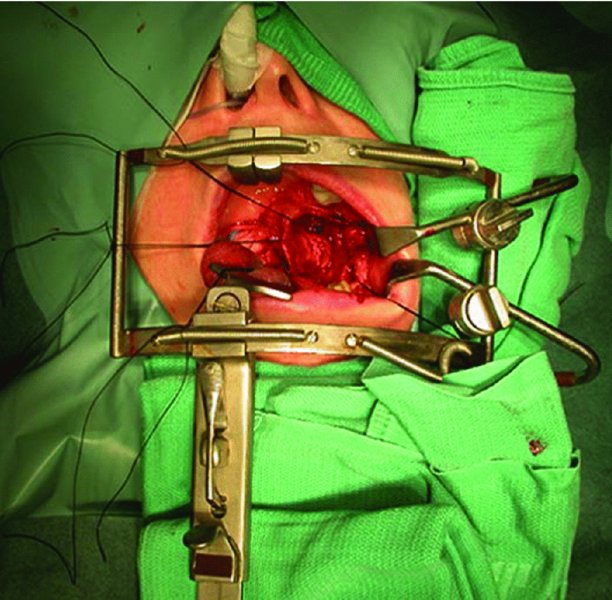
Figure 62.1. Access to the left lingual nerve using a modified Dingman–Zuniga mouth gag.
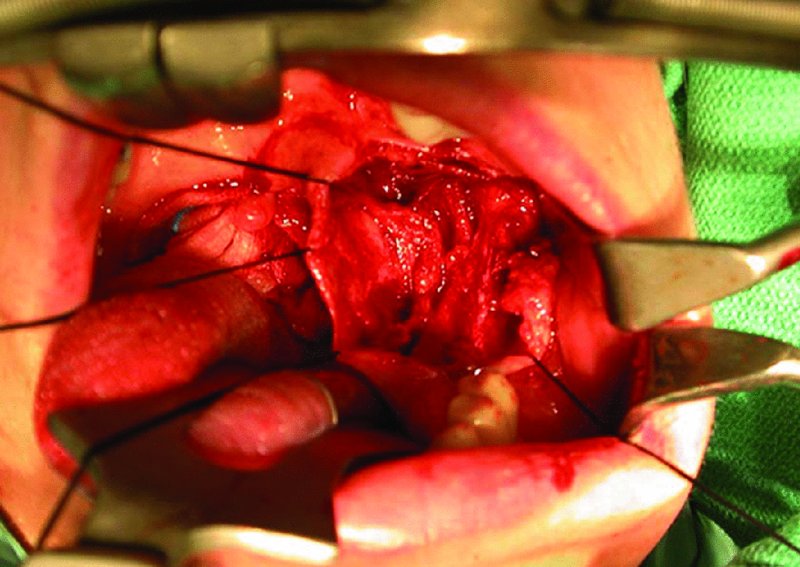
Figure 62.2. Buccal and lingual supraperiosteal flaps are raised and secured to the modified Dingman–Zuniga frame with 3-0 black silk sutures.
Preparation Phase
- The operating microscope is positioned over the operative field.
- The LN is exposed beginning at the healthy nerve proximal and distal to the injury site. Identification of the LN may be aided by locating its surrounding pouch of fat.
- The proximal and distal nerve segments are carefully retracted with a vessel loop at each segment.
-
The nerve is released from the injury site (Figures 62.3 and 62.9), which is usually adherent to the lingual surface of the mandible, with careful microdissection using curved microscissors.
- A modified background (1 × 1 inch neuropatty with the tubing of a small-gauge butterfly venipuncture system inserted and secured with silk sutures; the venipuncture needle is inserted into the lumen of an active suction tubing) is placed beneath the nerve injury site.
- The nerve injury is examined under microscopic magnification (25×). The nerve injury may be a complete transection with a neuroma at each end of the nerve stump or a partial transection with a neuroma in continuity.
- Excision of the neuroma is carefully performed with straight microscissors. The nerve ends are trimmed to expose the fascicular surfaces (Figure 62.4). The nerve site is irrigated with heparin–saline periodically.
- The nerve segments are reapproximated using 6-0 or 7-0 monofilament sutures (Figure 62.5) passed through the epineurium of each segment to the adjacent muscle, so as to facilitate nerve repair without undue tension. A nerve gap of approximately 1 cm or more usually cannot be coapted without tension and will require a nerve graft (Figure 62.10).
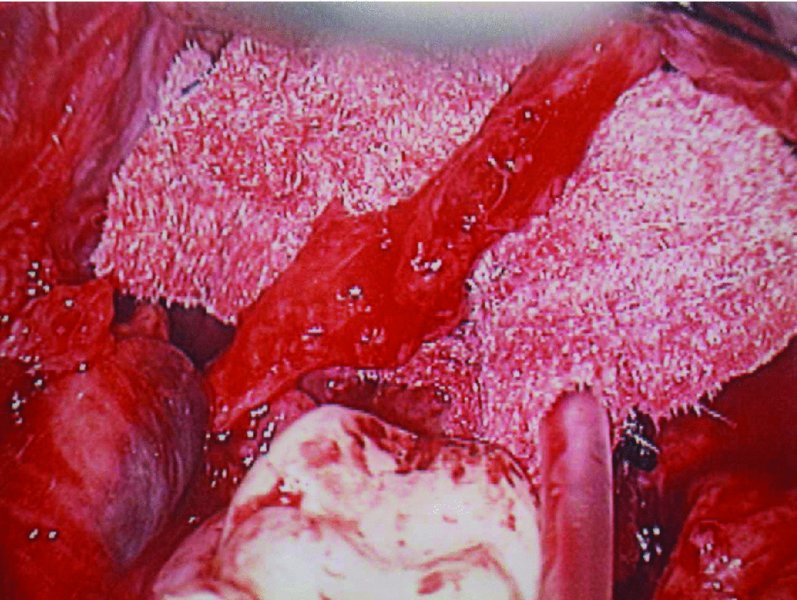
Figure 62.3. The lingual nerve is released from its position adherent to the lingual surface of the mandible and isolated with a neuropatty as background. A neuroma-in-continuity is visible as a bulge along the lingual nerve.
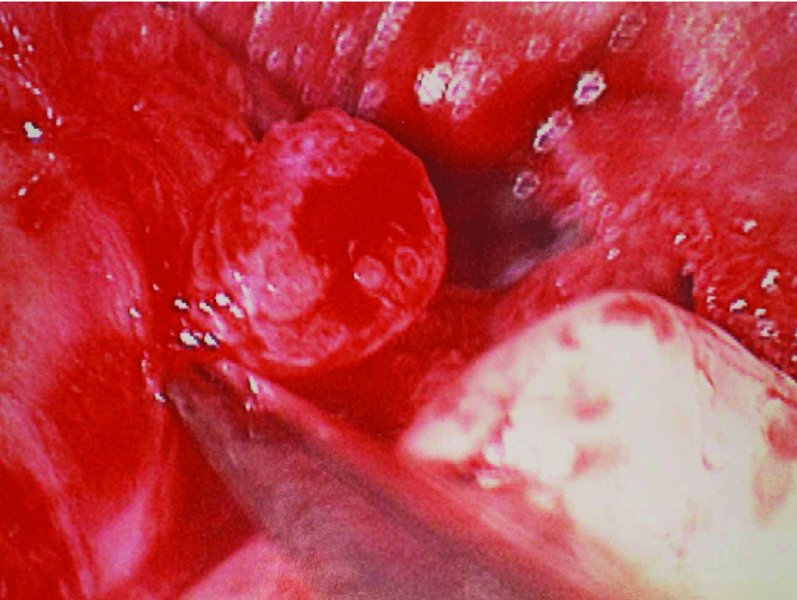
Figure 62.4. The neuroma is resected, and the cut end of the nerve stump with its fasicles is visible.
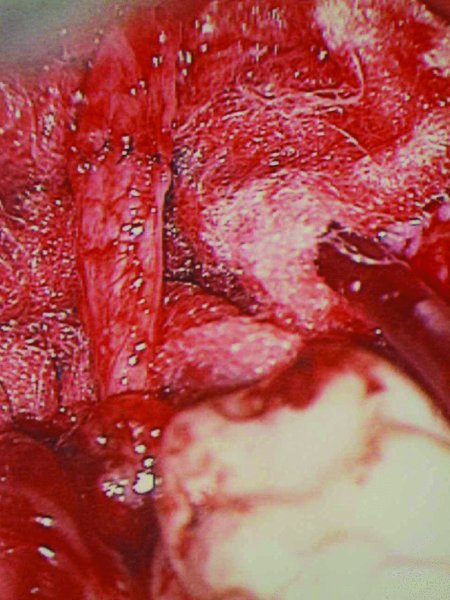
Figure 62.5. The stumps of the lingual nerve are approximated with 7-0 Ethilon sutures and coapted with eight 8-0 Ethilon microsutures.
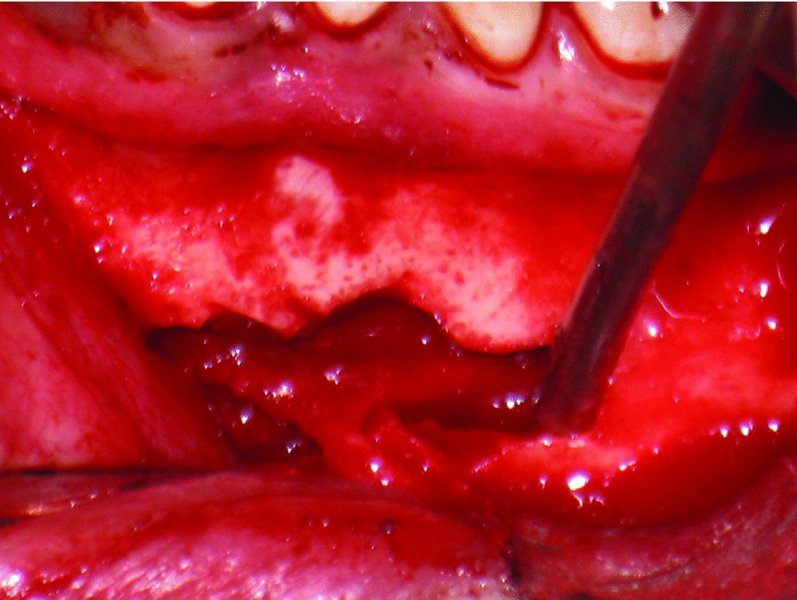
Figure 62.6. Removal of bone around the left mental foramen to expose the distal part of the left inferior alveolar nerve and the incisive branch.
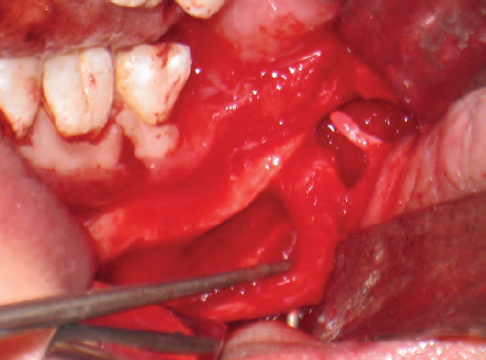
Figure 62.7. Site of neuroma-in-continuity within the left inferior alveolar nerve.
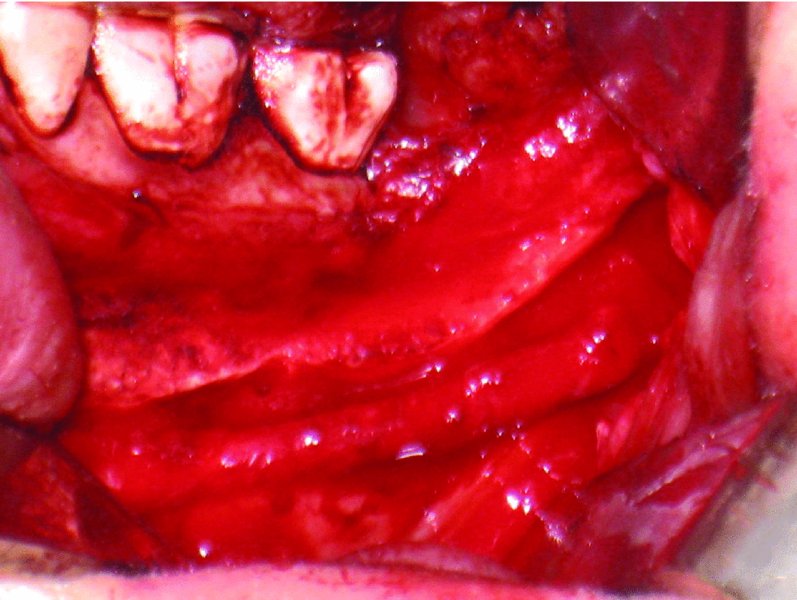
Figure 62.8. Left inferior alveolar nerve neuroma resected and neurorrhaphy completed.

Figure 62.9. Left lingual nerve isolated showing a neuroma-in- continuity.

Figure 62.10. Left lingual nerve neuroma resected, leaving a 9 mm gap that could not be approximated without excessive tension.
Microsuture Phase
- The trimmed nerve endings are coapted using the vasa nervorum as a guide to align the nerve segments. 8-0 or 9-0 monofilament sutures on a cutting needle are used to place sutures through the epineurium, including a little perineurium. The first suture is placed at the 12 o’clock position, leaving a longer strand. A second suture is placed at the 4 o’clock position. The suture strands are held in position with microforceps and “flip” the nerve over for access to the other side of the nerve. A similar suture is placed at the 8 o’clock position.
- Sutures are placed within the intervening gaps at regular intervals in the coaptation site circumferentially. Typically, 6–8 sutures are required.
- The repair site is examined, and excess suture length is trimmed.
- Once nerve repair has been completed, the approximating suture and background are carefully removed. Gelfoam may be wrapped around the repaired nerve, and the nerve is placed carefully into its bed.
Wound Closure
- The operating microscope is moved from the operative field.
- The black silk sutures retracting the buccal and lingual mucosal flaps are released and removed.
- The operative si/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


