6
What can be achieved with lasers: possible guided-tissue regeneration
In traditional hygiene, calculus and plaque biofilm present in any diseased periodontal pockets can be destroyed as much as possible. However, the goal is to get a long junctional epithelium for healing and inactivate any pocket so the gum is no longer diseased. Additionally, maintaining any diseased pockets after inactivating the disease and halting the pocket from getting worse would be ideal. For example, some treatments mean keeping a 6-mm pocket from getting worse; getting some attachment to create a shallower pocket; or maintaining this 6-mm pocket at a 6 mm by seeing the patient after scaling and root planing (SRP) have been performed and maintaining these pockets every 3 months to prevent them from getting worse.
But what is the normal healthy state after periodontal therapy? Healthy tissue has 3-mm (or less) pockets. It is important to note that once a patient has periodontal disease that they come in at least every 3 months. Failure to continue with maintenance after therapy will allow the condition to reoccur or even worsen.
USING LASERS
Soft-tissue lasers allow an epithelial tissue turnover rate 4 to 6 days in the junctional epithelium. Connective tissue heals after therapy with fibroblasts moving into wound site; synthesis becomes significant at approximately 7 days and peaks at 3 weeks. It may continue for months until tensile strength of tissue is restored (Wilson and Kornman 1996).
Periodontal tissue healing is a cellular race because epithelial tissue grows at 500 (0.5 mm) microns/day, and osteoblasts/fibroblasts grow at 80–100 (0.08 mm) microns/day. The connective tissue made up of fibroblasts accounts for 65% of the connective tissue-forming cells and osteoblasts are the bone-forming cells.
Hygienists can only destroy epithelium, not the connective tissue. This is why it is recommended to treat the sulcus by guiding the tissue back 1 mm at a time. In this way, the inflammation is stopped from the top down and the connective tissues is regenerated from the bottom up, which allows for a stronger attachment. Furthermore, the stronger attachment creates a stronger foundation for the teeth and allows for the likelihood of actual periodontal therapy maintenance as opposed to retreating the gum disease by doing traditional hygiene every year or two because the disease reactivates. The laser is now used as one of the tools to zip up any unresolved pockets during the maintenance phase after the initial therapy has taken place.
Epithelial tissue grows at a faster rate than does connective tissue. This is why it is recommended to disrupt the lateral epithelial attachment of junctional epithelium by retreating using the laser every 7 to 10 days. Please note these are guidelines for protocol when using soft tissue diode lasers, however, it is up to your office to determine the best protocol for your hygiene department.
Guided-tissue regeneration
Guided-tissue regeneration (GTR) refers to the procedures attempting to regenerate lost periodontal structures through differential tissue response. GTR alters wound healing by influencing cell proliferation and migration using fibroblasts and osteoblasts, hence receiving a stronger attachment.
The first principle evolved from periodontal wound-healing studies found that gingival epithelium migrates rapidly into most types of periodontal wounds. This forms a long junctional epithelium and prevents regeneration. Most periodontal wounds heal in this manner. This form of healing is considered a repair and not regeneration because of the original architecture and function of the periodontium is not restored (Wilson and Kornman 1996).
GTR is what the laser could accomplish with laser-assisted periodontal therapy.
Laser-assisted periodontal therapy
Laser-assisted periodontal therapy (LAPT) accomplishes these four things:
- Laser de-epithelialization (elimination of diseased tissue while leaving healthy tissue alone)
- Laser bacterial reduction (LBR)
- Biostimulation (low-level laser therapy [LLLT])
- GTR
Figure 6.1 An 8-month difference. Images courtesty of Kim Cardoza.

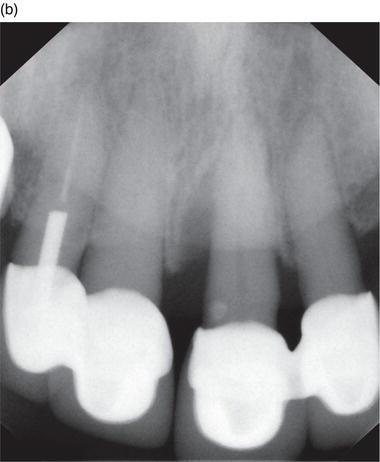
Figure 6.2 (a) Before laser therapy and (b) after laser therapy. Courtesy of Kim Stevens, RDH.


Biostimulation
Biostimulation increases four things:
- Collagen formation
- Circulation
- Osteoblastic formation
- Fibroblastic formation
Figure 6.3 (a)–(b) 1-year difference.

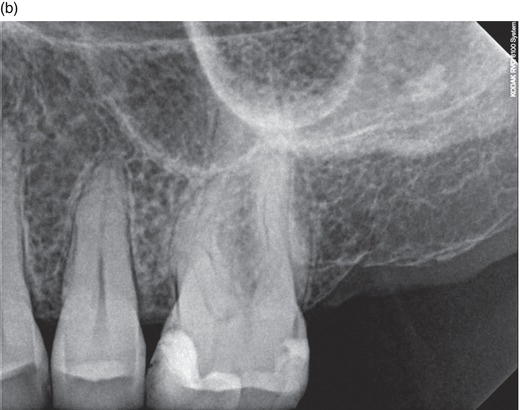
Figure 6.4 Traditional X-ray, starting to see the lamina dura forming, showing the signs of healing and possible bone regrowth.
Biostimulation with a diode laser at 3 J/cm2 can increase fibroblast proliferation six-fold. Low-intensity laser irradiation influences endothelial cell proliferation and might thereby contribute to the increase in angiogenesis and the acceleration of wound healing in vivo (Dortbudak, Haas, and Mallath-Pokorny 2000).
Other abilities that occur with the soft-tissue diode laser are the photobiological effects, which include:
- Photochemical effects
- Chemical reactions
- Chemical bonds
- Initiation of healing
- Elimination of infected or diseased sulcular epithelium and attachment from bottom up
- Biostimulation
- Pain relief
- Wound h/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


