6 Vascular, Neural, and Muscle Tumors
Vascular Lesions
Pyogenic Granuloma
Clinical Findings
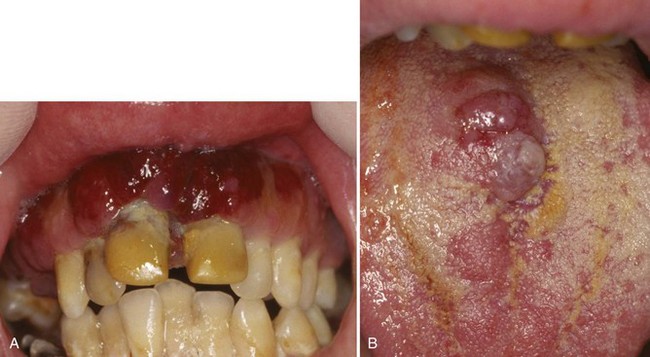
• Purple-to-red nodule or papule, sessile or pedunculated; common on the gingiva (75% of cases [see Chapter 5]), upper lip, and buccal mucosa; there may be a history of bleeding (Fig. 6-1, A and B).
• Patients on cyclosporine after stem cell transplantation develop pyogenic granuloma–like lesions on the buccal mucosa or tongue rather than the gingiva (see Fig. 6-1, C).
Etiopathogenesis and Histopathologic Features
Pyogenic granuloma represents a reactive proliferation of endothelial cells and blood vessels.
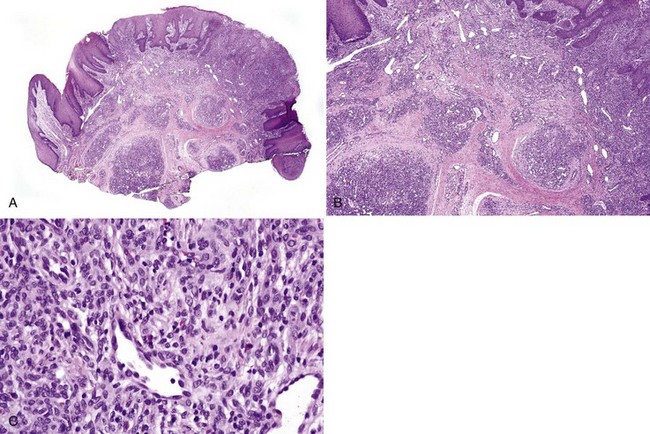
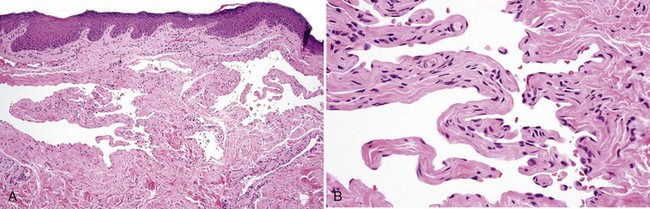
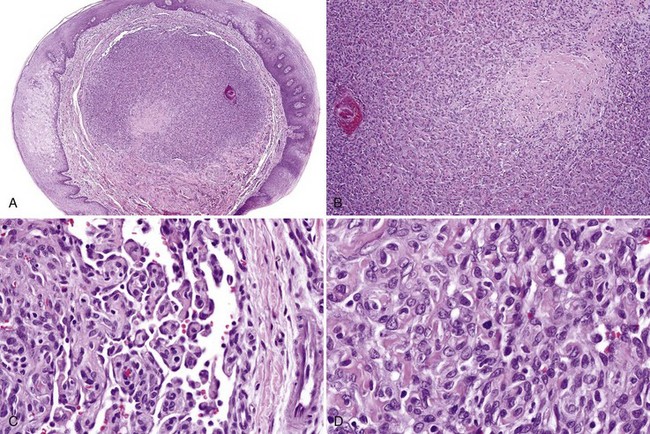
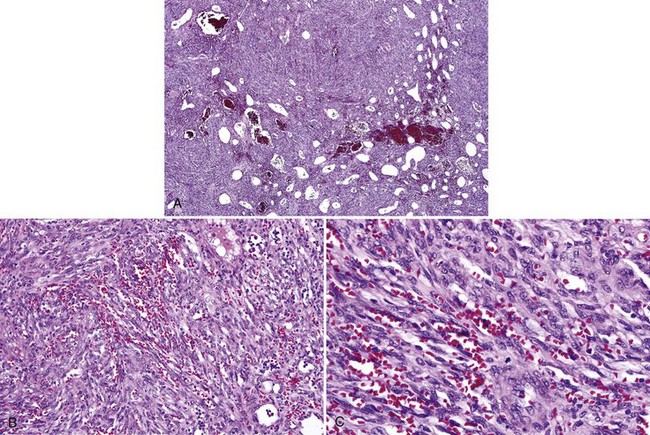
• Proliferation of endothelial cells and capillaries (often dilated)—sometimes in a lobular pattern, often with overlying ulceration—and acute and chronic inflammation are seen; mitoses are not uncommon (Figs. 6-2 and 6-3).
• Some lesions may show significant reactive atypia with hyperchromatic and pleomorphic nuclei (Fig. 6-4).
• Fibrous ingress signals organization, and lesions may convert to fibromas—especially gingival lesions (Fig. 6-5).
Fishman SJ, Mulliken JB. Hemangiomas and vascular malformations of infancy and childhood. Pediatr Clin North Am. 1993;40:1177-2200.
Johann AC, Salla JT, Gomez RS, et al. GLUT-1 in oral benign vascular lesions. Oral Dis. 2007;13:51-55.
North PE, Waner M, Mizeracki A, Mihm MCJr. GLUT1: a newly discovered immunohistochemical marker for juvenile hemangiomas. Hum Pathol. 2000;31:11-22.
Renshaw AA, Rosai J. Benign atypical vascular lesions of the lip. A study of 12 cases. Am J Surg Pathol. 1993;17:557-565.
Woo SB, Allen CM, Orden A, et al. Nongingival soft tissue growths after allogeneic marrow transplantation. Bone Marrow Transplant. 1996;17:1127-1132.
Varix (Venous Lake) and Venous Malformation (Venous Anomaly)
Clinical Findings
• Usually bluish blebs are less than 1 cm and found on the lips, tongue, or buccal mucosa, which may bleed; seen in middle-aged and older adults (Fig. 6-6, A-C).
• Bilateral ingual varices of the ventral tongue are common in older adults (see Fig. 6-6, D).
• Venous malformations are larger, often several centimeters in size, and usually are located on the tongue or lips (see Fig. 6-6, E).
Etiopathogenesis and Histopathologic Features
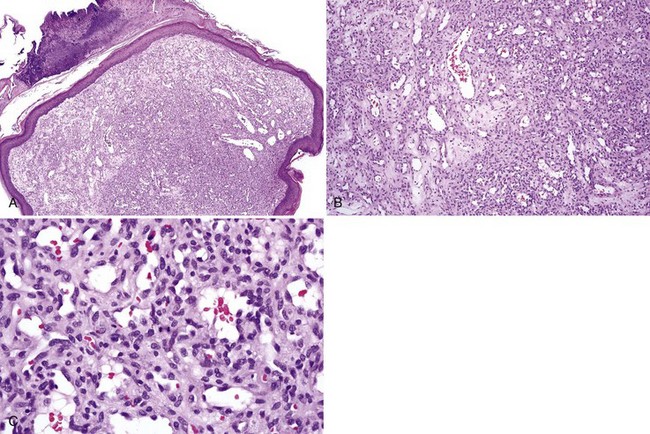
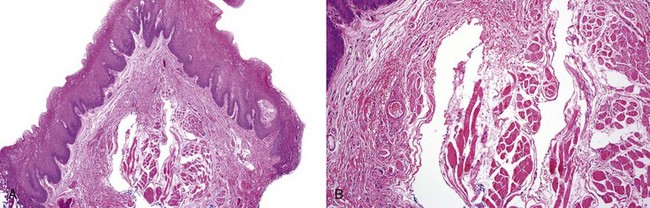
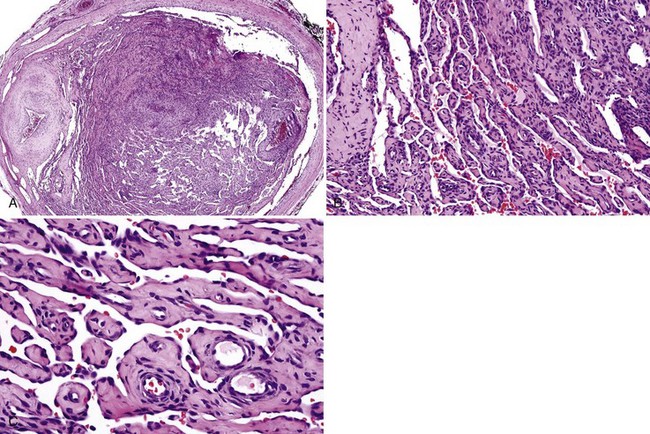
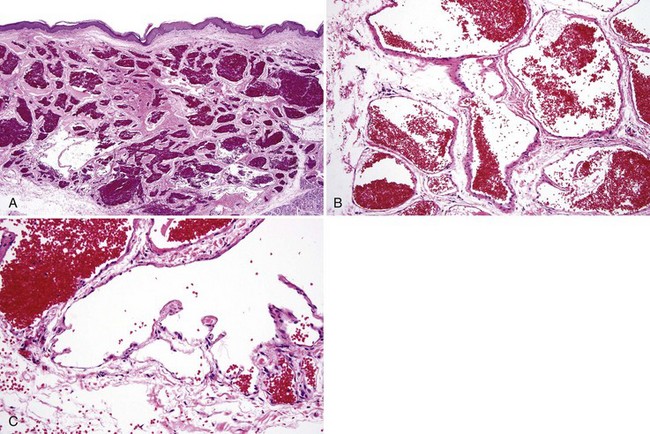
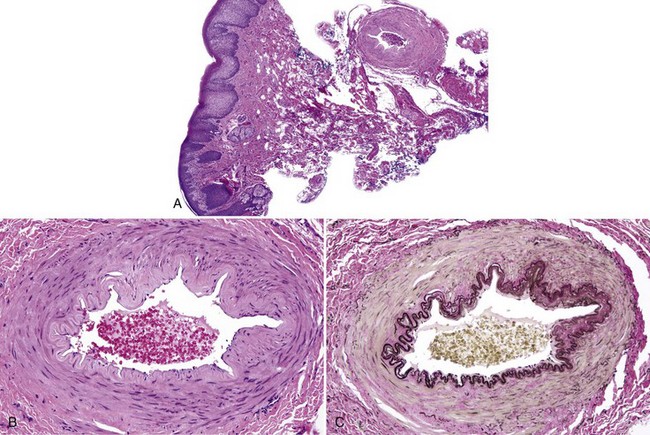
• Varix: dilated, tortuous, thin-walled vessels with a thin muscular coat; valve leaflets may be present (Figs. 6-7 and 6-8); thrombi in various stages of organization often noted with high cellularity or hyalinization; Masson tumor (intravascular papillary endothelial hyperplasia) sometimes seen (Figs. 6-9 to 6-11)
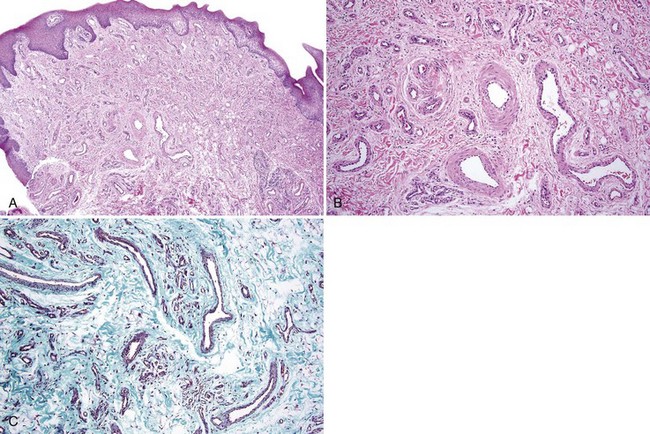
• Venous malformation: proliferation of venules of varying sizes, sometimes intramuscular in location without proliferation of endothelial cells (Figs. 6-12 and 6-13)
Differential Diagnosis
• Arteriovenous malformations show the presence of both arterioles and arteries and veins and venules; these lesions have high flow, and biopsy may lead to a severe bleeding episode.
• Hereditary hemorrhagic telangiectasia shows the presence of numerous small capillaries and venules in the lamina propria.
Buckmiller LM, Richter GT, Suen JY. Diagnosis and management of hemangiomas and vascular malformations of the head and neck. Oral Dis. 2010;16:405-418.
Hedstrom L, Bergh H. Sublingual varices in relation to smoking and cardiovascular diseases. Br J Oral Maxillofac Surg. 2010;48:136-138.
Hong SK, Lee HJ, Seo JK, et al. Reactive vascular lesions treated using ethanolamine oleate sclerotherapy. Dermatol Surg. 2010;36:1148-1152.
Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants and children: a classification based on endothelial characteristics. Plast Reconstr Surg. 1982;69:412-422.
Neville BW, Damm DD, Allen CM, Bouquot J. Oral and Maxillofacial Pathology, 5th ed. Philadelphia: Saunders; 2009.
Soares AB, Altemani A, Furuse C, et al. Intravascular papillary endothelial hyperplasia: report of 2 cases and immunohistochemical study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:708-711.
Caliber-Persistent Labial Artery
Jaspers MT. Oral caliber-persistent artery. Unusual presentations of unusual lesions. Oral Surg Oral Med Oral Pathol. 1992;74:631-633.
Lovas JG, Rodu B, Hammond HL, et al. Caliber-persistent labial artery. A common vascular anomaly. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86:308-312.
Piccione MJ, Manganaro AM, Almony JS. Caliber-persistent labial artery: diagnosis and treatment—case report. J Oral Maxillofac Surg. 2010;68:1987-1989.
Kaposi Sarcoma
Clinical Findings
• There are four clinical presentations: (1) classic type involves the skin of lower legs in older men; (2) African endemic type is disseminated and involves viscera; (3) iatrogenic type is associated with immunosuppression (especially renal and lung transplantation); and (4) epidemic type is found in patients with HIV/AIDS and involves multiple sites, especially the skin and the mouth (this coexists with the endemic form in Africa).
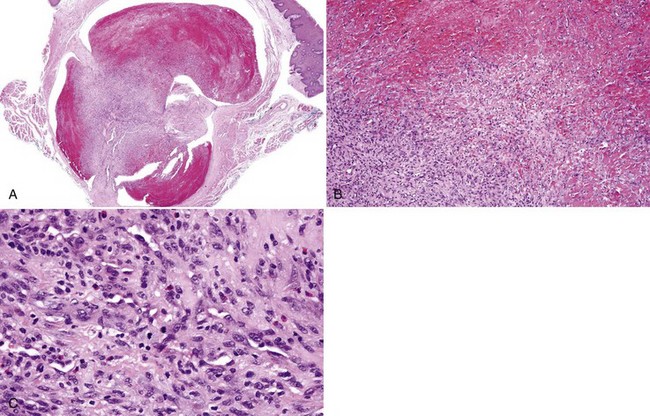
• Dusky red or purple macule (early lesion), plaque, or mass (late lesion) is usually on the maxillary gingiva, palate, or tongue (Fig. 6-15); oral involvement is seen in only 2% to 5% of nonepidemic cases and in 60% to 70% of patients with HIV/AIDS.
• Worsening of Kaposi sarcoma is one of the features of patients on highly active antiretroviral therapy who develop immune reconstitution inflammatory syndrome.
Etiopathogenesis and Histopathologic Features
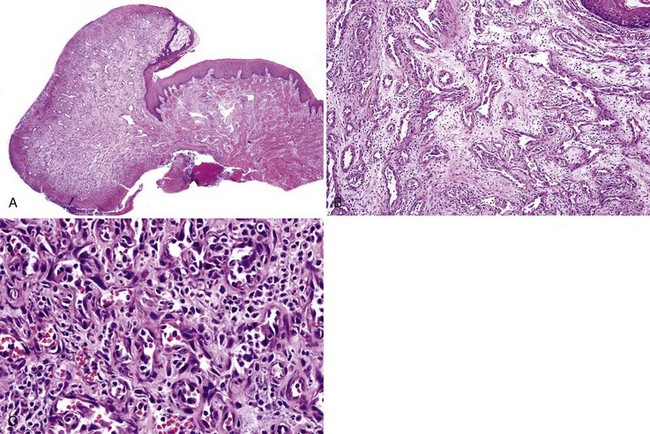
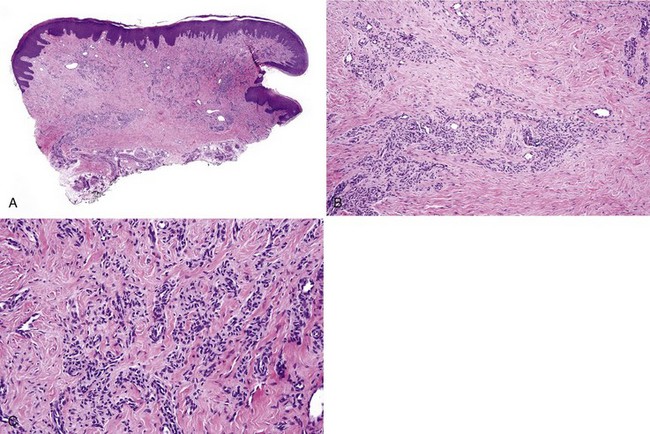
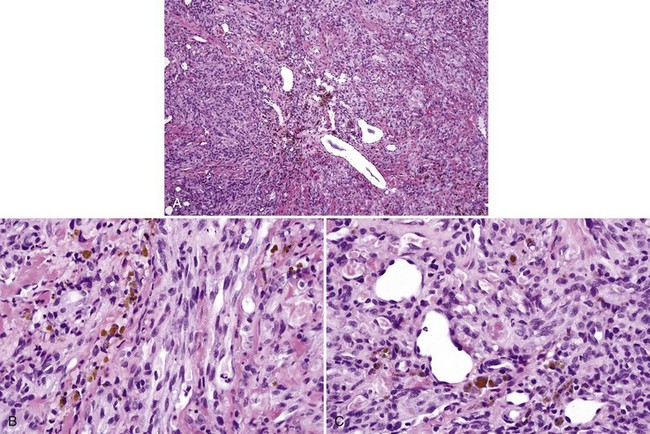
• Cellular proliferation of spindle cells in small whorls or fascicles with abundant extravascular erythrocytes, hemosiderin and globular eosinophilic deposits, and some intracytoplasmic granules; mitotic activity may be noted (Figs. 6-16 and 6-17).
• Studies for endothelial markers such as CD31, CD34, FLI-1, and Kaposi sarcoma–associated herpesvirus (especially LANA-1) are positive; studies for D2-40 may also be positive.
Management and Prognosis
• Patients newly diagnosed with HIV/AIDS require highly active antiretroviral therapy. Oral lesions are successfully treated with excision, laser ablation, intralesional vinblastine therapy, and radiation.
• Systemic therapy includes pegylated liposomal doxorubicin or daunorubicin.
• Reduction in immunosuppressive therapy in posttransplantation patients often leads to regression of tumors.
Bagni R, Whitby D. Kaposi’s sarcoma-associated herpesvirus transmission and primary infection. Curr Opin HIV AIDS. 2009;4:22-26.
Fletcher CD. The evolving classification of soft tissue tumours: an update based on the new WHO classification. Histopathology. 2006;48:3-12.
Folpe AL, Chand EM, Goldblum JR, Weiss SW. Expression of Fli-1, a nuclear transcription factor, distinguishes vascular neoplasms from potential mimics. Am J Surg Pathol. 2001;25:1061-1066.
Lamovec J, Knuutila S. Kaposi’s sarcoma. In: Fletcher C, Unni K, Mertens F, editors. World Health Organization Classification of Tumours: Pathology and Genetics of Tumours of Soft Tissue and Bone. Lyon: IARC Press; 2002:170-172.
Leidner RS, Aboulafia DM. Recrudescent Kaposi’s sarcoma after initiation of HAART: a manifestation of immune reconstitution syndrome. AIDS Patient Care STDS. 2005;19:635-644.
Patrikidou A, Vahtsevanos K, Charalambidou M, et al. Non-AIDS Kaposi’s sarcoma in the head and neck area. Head Neck. 2009;31:260-268.
Pantanowitz L, Otis CN, Dezube BJ. Immunohistochemistry in Kaposi’s sarcoma. Clin Exp Dermatol. 2010;35:68-72.
Pauk J, Huang ML, Brodie SJ, et al. Mucosal shedding of human herpesvirus 8 in men. N Engl J Med. 2000;343:1369-1377.
Ramirez-Amador V, Anaya-Saavedra G, Martinez-Mata G. Kaposi’s sarcoma of the head and neck: a review. Oral Oncol. 2010;46:135-145.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses