Chapter 6
Tooth Wear in Older Adults
Aim
The aim of this chapter is to discuss the cause of pathological tooth wear in older adults, its consequences and possible treatment options.
Outcome
At the end of this chapter, the practitioner should be familiar with the presenting signs of tooth wear and be able to diagnose the aetiological factors from the presenting signs. The practitioner should also recognise that, in older adults, intervention strategies should be as minimal as possible to reduce maintenance requirements.
Aetiology and Diagnosis
As older patients retain more teeth for life than ever before, a common finding is that of a worn dentition. The aetiology of tooth wear in this age group can be pathological or advanced physiological in origin. Tooth wear may not be problematic until the patient becomes concerned about:
-
appearance
-
function
-
long-term prognosis for the remaining teeth
-
comfort.
Tooth wear has a multifactorial aetiology. The causes of tooth surface loss are:
-
Attrition – which can be defined as tooth wear caused by excessive tooth to tooth contact. A typical attritional pattern of tooth wear is shown in Fig 6-1. In this patient tooth wear of attritional aetiology is shared between the maxillary and mandibular teeth. This pattern of tooth wear is common in bruxists. Attrition may be suspected if the patient admits to grinding their teeth. A relative may also confirm that the patient may grind their teeth when asleep. The incisal and occlusal surfaces are flattened, and the maxillary and mandibular teeth coincide during excursive movements.

Fig 6-1 Typical pattern of tooth wear associated with attrition. Note the even contacts on the incisal edges of the anterior teeth.
-
Erosion – which can be defined as tooth wear caused by acid attack of the teeth not due to caries. Sources of the acid causing erosive lesions can be intrinsic (gastric origin) or extrinsic (e.g. of dietary origin or exposure to industrial acidic chemicals). A typical presentation of erosive tooth wear is shown in Fig 6-2. Erosion is characterised by a saucerised (“cupped-out”) appearance of palatal and occlusal surfaces. The remaining enamel around the wear lesions is thin and often irregular. The teeth have a shiny appearance, but may appear stained if the wear process is not active. Amalgam restorations stand proud of the teeth. In severe cases, the labial and buccal aspects of the teeth may also be affected. Mandibular incisor teeth may be unaffected, and this is believed to be due to the tongue protecting these teeth. The distribution of the worn surfaces gives an indication of the aetiology of erosion. If erosion is caused by dietary factors alone, the palatal surfaces of maxillary anterior teeth are the most affected surfaces. Common causes of this type of erosion are carbonated drinks, citrus fruits and fruit juices consumed on a frequent basis. A dietary history should elicit these factors. Should lesions of an erosive aetiology be noticed on the molar teeth, the clinician should suspect that acid from the stomach is getting into the oral cavity. This type of tooth wear is seen in patients with:

Fig 6-2 The dentition of a patient with erosive tooth wear of dietary origin. This patient consumed two litres of carbonated lemonade per day.
-
alcohol abuse behaviour
-
hiatus hernia
-
bulimia
-
duodenal ulceration
-
taking certain medications (e.g. ibuprofen).
In these situations, the dentist should consult with the patient’s general medical practitioner. The diagnosis of tooth wear of erosive aetiology should be outlined to the medical practitioner. The dental practitioner should indicate that gastric reflux is the suspected cause, and enlist the aid of the medical practitioner in establishing a firm diagnosis. This may warrant referral to a gastroenterologist for further investigation.
-
-
Abrasion – which can be defined as tooth wear caused by physical contact with an agent other than tooth (e.g. toothbrush abrasion) (Fig 6-3). Abrasion is characterised by a pattern of wear consistent with the tooth being abraded by an object such as a toothbrush. The affected surfaces, usually on the buccal and labial surfaces, will have irregular wear patterns.

Fig 6-3 Abrasion of the buccal surfaces of teeth. This patient brushed with baking soda on a daily basis in an attempt to brighten the colour of her teeth.
-
Abfraction – non-carious cervical tooth-surface loss caused by flexure of cusps. These present as wedge-shaped cavities on cervical margins of teeth and are typically found on maxillary canine and premolar teeth (Fig 6-4). It is difficult to envisage how this could be due to an abrasive agent such as a toothbrush, or why it is confined to a small number of teeth. The proposed mechanism for this is that occlusal stresses on teeth with steep cusps are transmitted to the cervical margin. The enamel in this region is thin, and consequently fractures.

Fig 6-4 Tooth wear caused by heavy occlusal contacts (abfraction). Note the heavy contact between the buccal cusps of the premolar teeth. (Courtesy of Dr F Burke)
Key Decisions
Tooth wear frequently has a multifactorial aetiology and management of tooth wear is complex. It can be difficult to decide whether tooth wear should be monitored once diagnosed or whether intervention is required. The key points in the management of tooth wear are summarised in Fig 6-5. Examine the pattern of wear on the tooth surfaces to diagnose the aetiology of tooth wear. The clinician should remember that it is not uncommon for more than one than one type of tooth wear to occur simultaneously.
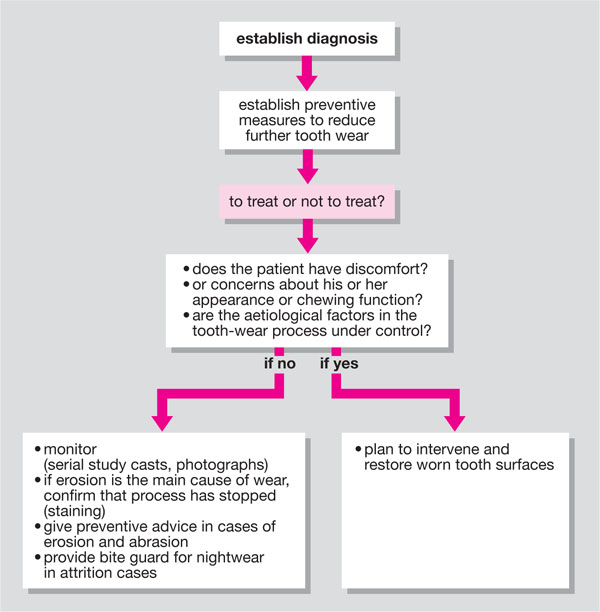
Fig 6-5 Key points in the management of tooth wear.
The decision to intervene in tooth wear cases should be undertaken with care. If the patient is not in pain and has no functional or aesthetic complaints, then a preventive strategy and monitoring is advisable. In cases of attrition, an occlusal acrylic splint can be used for night-time wear to reduce tooth wear. When erosion is suspected, the precise cause should be investigated. A dietary history should be recorded, and possible erosive agents identified. The patient should be advised to modify the intake of erosive agents, specifically to reduce frequency of intake. If a gastric cause is suspected, then the patient’s medical history should be reviewed and causes of gastric acid reflux identified. Occasionally, erosive tooth wear may be the first clue as to an underlying gastrointestinal disease. A further cause may be bulimia, although this is unusual in older adults. Appropriate medication and advice should be provided via the patient’s physician. When abrasion is suspected, then the patient must be advised to modify their habits such as use of abrasive tooth cleaning agents. Where abfraction lesions are diagnosed, modification/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


