Chapter 6
The Contribution of Periodontics to Prosthodontics: Treatment Planning of Patients Requiring Combined Periodontal and Prosthodontic Care
Treatment planning for patients with complex dental needs involves multidisciplinary collaboration with the prosthodontist, periodontist/oral surgeon, orthodontist, endodontist, and patient. It is a carefully sequenced process and is designed to eliminate or control etiologic factors, repair existing damage, and create a functional, maintainable oral environment. Successful treatment depends on a thorough evaluation of all available information, a definitive diagnosis, and a thorough integration of all necessary procedures prescribed for the patient. The treatment process is composed of a series of phases: a diagnostic phase, a treatment-planning phase, a treatment phase, and a maintenance phase.
DIAGNOSTIC PHASE (DATA COLLECTION)
Diagnosis involves the collection of data obtained from a comprehensive patient history (medical and dental), a patient interview (chief complaint), a clinical examination (inspection, palpation and percussion), a critical evaluation of mounted diagnostic casts, and a radiologic interpretation.
Patient History
Patient’s Social and Environmental History
The patient’s social and environmental history are important adjuncts to diagnosis and treatment planning and can often determine the entire course of treatment. Examples include a patient’s age, gender, occupation, alcohol intake, tobacco use, and illicit drug use.
Medical History
The importance of an accurate comprehensive medical history cannot be overstated. The medical history reveals systemic conditions that could be contributing factors related to the existing dental disease or that could affect the prognosis of dental treatment. A thorough medical history and interview should reveal any previous systemic diseases, injuries, surgical procedures, allergies, adverse drug reactions, and medications. An example of a systemic disease affecting oral health is diabetes mellitus. Patients with diabetes mellitus are more likely to develop periodontal disease compared with patients without diabetes, and periodontal disease is often considered the sixth complication of diabetes mellitus. Patients with uncontrolled diabetes are especially at risk (Mealey and Oates 2006).
The medical history can also alert the dentist to other disorders, such as a prosthetic cardiac valve that require antibiotic prophylaxis (Davies 1993). The presence of a pacemaker contraindicates the use of electrosurgery (Flocken 1980). Previous radiation therapy for neoplastic diseases of the head and neck region can have a profound effect on the oral cavity (AAP position paper, 1997). Medications causing xerostomia can lead to cervical dental caries and periodontal disease, and can contribute to early failure of fixed restorations (Thomson et al. 2006). Osteonecrosis of the jaw has been observed in cancer patients who have undergone invasive dental procedures, such as dental implant surgery or tooth extractions, while receiving treatment with intravenous bisphosphonates. Invasive dental procedures should be avoided for these patients whenever possible (Soileau 2006, Wooltorton 2005).
Dental History
The dental history serves as a companion to the medical history. It establishes information on the patient’s involvement in previous dental treatment, when and why missing teeth were removed, previous problems with dental treatment, parafunctional habits, and oral hygiene habits.
Chief Complaint
The chief complaint can establish the need for additional diagnostic tests to assist in determining the cause of the dental problems. It is important that any recommended treatment addresses this chief complaint and that the patient’s expectations with regard to the outcome of treatment are realistic.
Clinical Examination
Extraoral Examination
A thorough examination should include an evaluation of the size, shape, and symmetry of the head and neck including the patient’s profile (retrognathic, mesiognathic, prognathic). Normal and abnormal clinical findings should be noted in detail as a permanent component of the patient’s record.
The intraoral examination includes screening for malignancies, an evaluation of the patient’s overall caries activity, a general overview of the periodontal status, and the quality and quantity of saliva. The dentist should then thoroughly examine the existing restorations and their status, the presence of dental caries, and missing teeth. A complete periodontal assessment is an important component of a comprehensive oral examination. It includes an evaluation of the oral hygiene, a description of the color, form, and texture of the gingiva, a recording of probing depths, an assessment of bleeding on probing, a determination of tooth mobility, a mucogingival evaluation, and an evaluation of furcations.
Occlusal Examination and Analysis
One of the most critical factors with regard to treatment planning is an evaluation of the patient’s occlusion. Alterations and deviations in the occlusal plane can result in a dysfunctional maximal intercuspal position (MIP), attrition, bruxism, widened periodontal ligament spaces (trauma from occlusion), and impaired mastication. Mounted diagnostic casts represent an important diagnostic aid for the thorough evaluation of a patient’s occlusion (Morgano et al. 1989).
Radiographic Examination
Basic knowledge of normal radiographic appearances is essential. The minimal examination requirements for a comprehensive treatment plan include a panoramic radiograph and a complete-mouth radiographic series. The presence of dental caries, loss of tooth-supporting bone, furcation invasions, and any other abnormalities should be carefully noted and recorded in the patient’s record.
Diagnostic Casts and Diagnostic Waxing
Diagnostic casts are made from impressions of the dental arches. Irreversible hydrocolloid (alginate) material is usually used in stock metal trays. The trays should allow a uniform thickness of 3 to 5 mm of impression material. These trays should be large enough to cover the retromolar pads in the mandible and the hamular (pterygomaxillary) notches in the maxillary arch. The impressions should be poured immediately with cast (Type III) stone. Once the casts are retrieved, small nodules are removed. The casts are mounted in a semiadjustable articulator with a face-bow transfer. Duplicate diagnostic casts are also made and mounted. A diagnostic waxing of the proposed treatment plan is then made. Diagnostic casts and the diagnostic waxing represent the guide or “blueprint” for the restorative plan that assists the dentist and laboratory technician in coordinating the reconstruction of aesthetics, phonetics, and function (Morgano et al. 1989).
Prognosis
The prognosis is a forecast of the probable course and outcome of a disorder. The overall prognosis is concerned with the entire dentition. Criteria used to assign a prognosis to individual teeth are subjective and are usually based on clinical and radiographic findings. A favorable, questionable (guarded), unfavorable (poor) or hopeless prognosis is assigned to each tooth depending on available bone support, probing depths, furcation exposure, mobility, crown-to-root ratio, root proximity, occlusal relationships, extent of tooth damage, abutment status, endodontic status, remaining tooth structure (restorability), caries susceptibility, quality and quantity of saliva, and parafunctional habits.
Making the decision to retain or extract a compromised tooth requires a thorough evaluation of all factors, including the expense and discomfort involved in maintaining the tooth, the overall strategic value of the tooth, available literature from clinical studies on the probability of success of the treatment required to retain the tooth, the prognosis of an artificial replacement for the tooth, and the patient’s desires, expectations and needs. Extraction of one or more teeth may be prescribed based on the presence of one or more of the following factors: greater than 75% bone loss, Miller Class III mobility (greater than 1-mm buccolingually, or a vertical mobility) (Miller 1950), Glickman advanced Grade II or Grade III/IV (through-and-through defect) furcation invasion (Glickman 1958), recalcitrant probing depth(s) greater than 8 mm, unfavorable crown-to-root ratio, and a history of recurrent periodontal abscesses. A tooth can also be extracted for aesthetic reasons or to improve the results of orthodontic treatment. When a surgical crown-lengthening procedure will lead to compromised esthetics, furcation invasion, and/or poor crown-to-root ratio, extraction is commonly advised (Becker et al. 1984, Chase and Low 1993).
Diagnosis
Diagnosis is a determination of any variations from what is considered normal. The dentist should be sensitive to the signs and symptoms presented and note any variations from normal. The dental diagnosis commonly includes a determination of the periodontal health, occlusal relationships, function of the temporomandibular joints (TMJs) and muscles of mastication, condition of edentulous areas, anatomic abnormalities, serviceability of existing prostheses and restorations, and status the of the remaining dentition.
Sequencing of the treatment plan involves the process of scheduling the necessary procedures into a time-frame. Effective sequencing is critical to the success of any treatment plan. Some treatment procedures must follow others in a logical order, while other treatment procedures can or must occur concurrently. Thus, thoughtful coordination is mandatory. Complex treatment plans are commonly sequenced into phases, including a control phase, an evaluative phase, a definitive phase, and a maintenance phase.
Control Phase
The control phase is divided into two parts: an initial periodontal phase and a provisional phase. This phase is intended to remove the etiologic factors, stabilize the patient’s oral health, eliminate any active periodontal disease, and resolve inflammation. In this phase, often only a tentative treatment plan can be presented to the patient. Changes commonly occur relative to the prognosis of individual teeth at the termination of this phase. The initial periodontal phase includes extraction of hopeless teeth, periodontal debridement and scaling, oral hygiene instructions, and any indicated occlusal adjustments. The provisional phase then strives to remove conditions preventing effective maintenance, beginning the preventive dentistry component of the treatment. This phase includes caries control to determine restorability of teeth, replacement or repair of defective restorations, minor tooth changes, and an endodontic evaluation of all remaining teeth.
Evaluative Phase
The evaluative phase occurs between the control and the definitive phase. It allows for resolution of inflammation and time for healing. Home-care habits are reinforced, motivation for further treatment is assessed, and all preliminary treatment is reevaluated before definitive care is initiated.
Definitive Phase
After completing the control and the evaluative phase, the patient can enter the definitive phase. This phase begins with presenting the definitive treatment plan to the patient, including a wax replica of the proposed treatment plan. This phase is also divided into two parts: a preprosthetic phase and a prosthetic phase. The preprosthetic phase includes preprosthetic periodontal, oral surgical, endodontic, or orthodontic procedures. If implant surgery is proposed, then a computed tomographic (CT) scan is prescribed to evaluate the width and height of available bone as well as the location of vital structures, such as the inferior alveolar nerve, artery, and vein (inferior alveolar canal and mental foramen). The definitive phase is completed with the prosthetic phase for the fabrication and delivery of prostheses.
Some of the considerations and suggestions a dentist should follow when providing fixed prosthodontic treatment include the following (Morgano et al. 1989):
- A physiologic plane of occlusion
- A physiologic vertical dimension of occlusion (VDO)
- Simultaneous contacts of all anterior and posterior teeth in MIP
- A functional anterior guidance free of posterior interceptive occlusal contacts
- An unlocked arrangement of cusps and fossae that will allow comfortable jaw function
- Axial loading of posterior teeth
- The use of a material that will not unduly abrade the opposing dentition
- Narrowed occlusal tables, especially with implant-supported restorations, to minimize unfavorable leverage and bending moments
Maintenance Phase
This phase includes regular recall examinations that may reveal the need for adjustments to prevent future breakdown and provides an opportunity to reinforce home care. The frequency of this phase depends on the patient’s risk for developing new dental disease. Maintenance visits are usually at 3- to 6-month intervals.
The prognosis can be divided into a short- and long-term prediction, based on an educated forecast of the response to the planned treatment. It must take into account existing dental and periodontal support, vulnerability to expected disease, host resistance, the patient’s adaptability, the dentist’s capabilities, and expectations with regard to the patient’s compliance with prescribed measures. When determining a prognosis, it should be tailored to the specific clinical situations. The prognosis can be (1) favorable, (2) guarded (questionable), (3) unfavorable (poor), or (4) hopeless. The dentist should provide a treatment plan that offers a favorable prognosis (McGuire 1991).
A favorable prognosis implies a high probability of success based on the best available evidence. A guarded or questionable prognosis suggests that one or more mitigating factors are present that are known to adversely affect the outcome of care. As an example, an endodontically treated tooth restored with a post-and-core and crown but lacking a ferrule would have a questionable prognosis (Morgano and Brackett 1999). An unfavorable (poor) prognosis implies a high probability of failure. A molar with a Glickman Grade III or IV furcation invasion will usually have a poor prognosis. Teeth with a hopeless prognosis cannot be treated with current materials and methods and must be extracted. An example is a pulpless tooth with a longitudinal root fracture that extends deeply into the alveolar bone.
Patients
Throughout this chapter, the Universal Numbering System has been used to designate individual teeth. Figure 6.1 summarizes and illustrates this numbering system.
Fig. 6.1. Numbering system used in this chapter.

Patient I
A 43-year-old woman presented to the clinic with a chief complaint of, “I don’t like my smile.” (Figs. 6.2 and 6.3).
Fig. 6.2.Full-face frontal view of patient.

Fig. 6.3. Smile line.

Diagnostic Phase
The patient’s medical history was noncontributory. She did not have any known drug or food allergies. She did not smoke and drank alcohol only occasionally. Her dental history included orthodontic treatment that was performed many years previously to move the maxillary canines into the positions of the lateral incisors. She brushed twice per day and did not use dental floss. Extraoral examination revealed no cervical or submandibular lymphadenopathy and no signs of temporomandibular disorders (TMD) or reports of muscle pain.
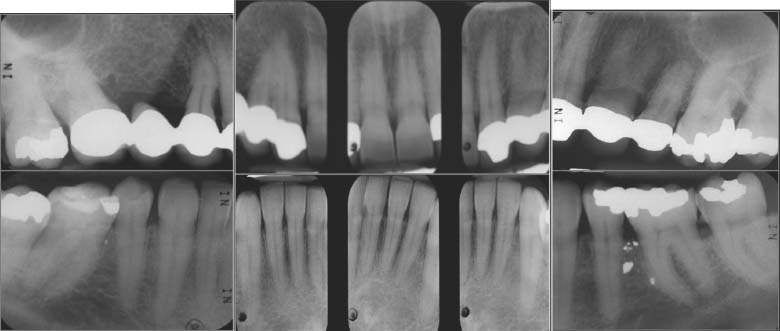
The intraoral and radiographic examinations noted the following (Figs. 6.4 and 6.5):
Fig. 6.4. Intraoral view.

Fig. 6.5. Complete-mouth radiographs.
- Missing Nos. 1, 5, 16, 17, and 32 and congenitally missing Nos. 7, 10, 20, and 19
- Maxillary canines in the position of the lateral incisors and restored with metal-ceramic crowns to mimic lateral incisors
- MO silver amalgam restorations, Nos. 2, 15, 30, and 31
- Metal-ceramic fixed partial dentures (FPDs), Nos. 3-x-5-6, and splinted crowns, Nos. 12-13-14
- MOD silver amalgam restoration, No. 16
- Defective MO silver amalgam restoration, No. 18
- DO silver amalgam restoration, No. 20
- Occlusal silver amalgam restoration, No. 30
- Generalized inflammation with supragingival calculus in the mandibular anterior
- Bony defect, site No. 4 (extraction site)
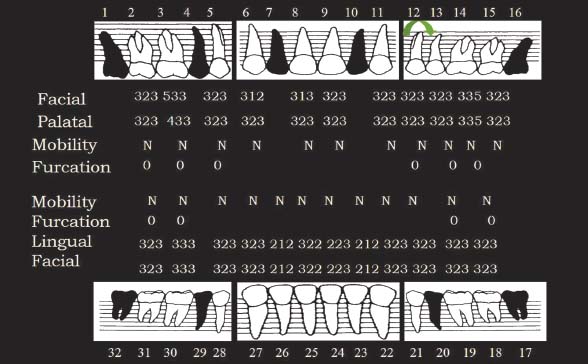
- Probing depths within normal range for most teeth with the exception of teeth No. 3 (distal 5 mm) and No. 14 (distal 5 mm) (Fig. 6.6)
- Rotated tooth, No. 12
- Absence of hypermobility or furcation invasion
Fig. 6.6. Periodontal charting.
The diagnosis for this patient was as follows:
- Generalized chronic mild gingivitis
- Localized chronic moderate periodontitis
- Partial edentulism
- Multiple defective dental restorations
Treatment Planning Phases
The objectives of therapy for this patient were elimination of the etiologic factors (open margins and defective restorations), control and resolution of periodontal inflammation, and restoration of esthetics and function. Initially, only a tentative treatment plan was presented to the patient. This plan included the removal of artificial crowns, evaluation of the restorability of teeth, and plaque control measures.
Initial Periodontal Phase
This phase included scaling and root planing on the distal surfaces of Nos. 3 and 14, oral hygiene instructions, and reevaluation of any pocket reduction and oral hygiene.
Provisional Phase
In the provisional phase, the defective fixed restorations were removed (Figs. 6.7 and 6.8) and replaced with physiologically and aesthetically acceptable provisional restorations.
Fig. 6.7.A, Teeth Nos. 3, 5, and 6 after removal of defective restorations. B, Teeth after repreparation

Fig. 6.8.A, Teeth Nos. 11, 12, and 13 after removal of defective restorations. B, Teeth after repreparation

In evaluating the gingival line in the maxillae, a gingival line discrepancy was noted that was caused by the pontic in the area of No. 4. This discrepancy compromised the overall aesthetic appearance and contributed to plaque accumulation. There was also a gingival line discrepancy between the central incisors and the lateral incisors because the lateral incisors were originally canines that were orthodontically repositioned.
In addition, there was a gingival line discrepancy between Nos. 11, 12, and 13 (Fig. 6.9). Based on these findings, a definitive treatment plan was presented to the patient. This plan was (Fig. 6.10) as follows:
Fig. 6.9. Provisional restorations, Nos. 3-x-5, 6, 11, 12, and 13. Note the gingival line discrepancies at sites Nos. 3-x-5, 8-9, and 11-12-13.

Fig. 6.10. Preprosthetic treatment plan: A, Soft tissue augmentation, area No. 4. B, Microsurgical crown-lengthening procedure, Nos. 8 and 9, for aesthetic purposes. C, Crown-lengthening procedure, No. 13, for aesthetic purposes.

- Soft tissue augmentation, area No. 4
- Microsurgical crown lengthening procedure, Nos. 8 and 9 for aesthetic purposes
- Surgical crown-lengthening procedure, No. 13 for aesthetic purposes
- Metal-ceramic FPD, No. 3-x-5
- Ceramic crowns, Nos. 6 and 11
- Porcelain laminate veneers, Nos. 8 and 9
- Metal-ceramic crowns, Nos. 12 and 13
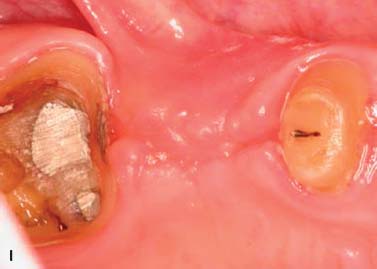
Preprosthetic Periodontal Phase
Soft tissue inlay graft, site No. 4. A split-thickness flap was elevated. Soft tissue augmentation for site No. 4 was accomplished by using an autogenous connective tissue inlay graft obtained from the patient’s palate. The graft was sutured and secured to the periosteum. The flap was positioned and sutured without tension. The tissue surface of the pontic was relieved in the area of the surgical site to prevent tissue impingement. The pontic was relined 8 weeks after surgery with autopolymerizing acrylic resin (Coldpac; the Motloid Co., Chicago, IL, USA) to allow gentle pressure on the graft to contour the soft tissue at the pontic site and develop an esthetic gingival line. The pontic was relined again 1 week later to allow for additional contouring of the gingival line (Fig. 6.11).
Fig. 6.11. A, B, Soft tissue inlay graft site No. 4, preoperative view. C, Split-thickness flap site No. 4. D, Connective tissue graft obtained from the patient’s palate. E, Graft sutured to the periosteum with chromic gut sutures. F, G, Flap sutured without tension. H, One week after surgery. I, Two months after surgery.


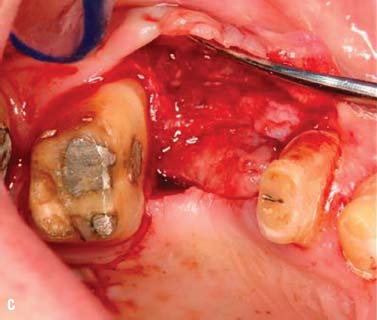

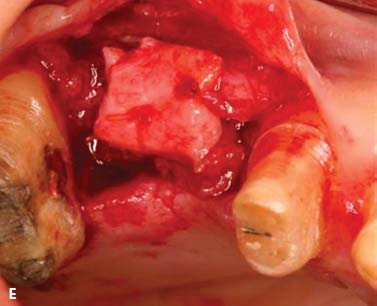
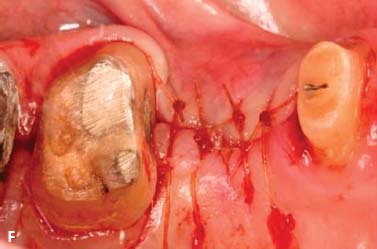


Surgical crown lengthening, No. 13. A submarginal incision was made at the anticipated gingival line and a full-thickness flap was elevated. Ostectomy was performed to allow a 3-mm distance between the anticipated gingival line and the crest of the alveolar bone (Rosenberg et al. 1980).
The flap was repositioned and sutured with 4-0 chromic gut sutures (Fig. 6.12).
Fig. 6.12. Surgical crown lengthening procedure tooth No. 13. A, Preoperative view. B, 3-mm distance allowed between anticipated finish line of crown preparation and alveolar crest. C, Site sutured with vertical mattress technique and 4-0 chromic gut sutures. D, Two weeks after surgery.




Surgical crown lengthening, Nos. 8 and 9. Surgical crown lengthening was required for aesthetic reasons on the facial surfaces of Nos. 8 and 9 only (Fig. 6.13).
Fig. 6.13. Microsurgical crown-lengthening procedure for the facial surfaces of Nos. 8 and 9 to correct gingival line discrepancy. A, Preoperative view. B, Vertical incisions at the line angles of Nos. 8 and 9 by using a microsurgical blade. C, Full-thickness flap elevated. D, Ostectomy completed. E, Flaps sutured with 7-0 Vicryl sutures. F, One week after surgery. G, Two weeks after surgery.







To preserve the papillae and the soft tissue around Nos. 7 and 10, a microsurgical crown-lengthening procedure was performed. There are many advantages of this technique when compared with conventional surgical crown lengthening procedures (Dibart and Karima 2006). This procedure
- Is less invasive
- Requires smaller incisions
- Allows greater precision when closing wounds
- Is less traumatic
- Is less painful postoperatively
- Allows faster healing and vascularization
- Produces more predictable results in areas with very thin gingiva or in the “aesthetic zone”
Prosthetic Phase
Figure 6.14 is a wax replica of the proposed treatment plan.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


