chapter 6 Radiographic Modalities for Dental Implants
Successful oral implantation is highly dependent on proper preoperative treatment planning, in which appropriate radiographic evaluation of the edentulous ridge and potential implant site(s) plays a key role.1,2 The American Academy of Oral and Maxillofacial Radiology recommended in 2000 that clinicians employ cross-sectional imaging when planning implant cases; additionally, the Academy noted that conventional cross-sectional tomography should be the preferred method for obtaining this information for most implant patients.3 Modern imaging techniques are facilitating the trend toward nonspecialist placement of implants in the dental office; the dentist can choose the appropriate radiographic modality—digital or film—that enables him or her to plan treatment, place the implants, perform restoration and proper postoperative treatment, and use intraoral and panoramic images—both linear and complex motion tomography, as well as computed tomography.4,5 A thorough radiograph examination should enable the surgeon to assess the quantity and quality of the bone present and to visualize the locations and relationships between critical internal anatomical structures.6–9
Intraoral Films
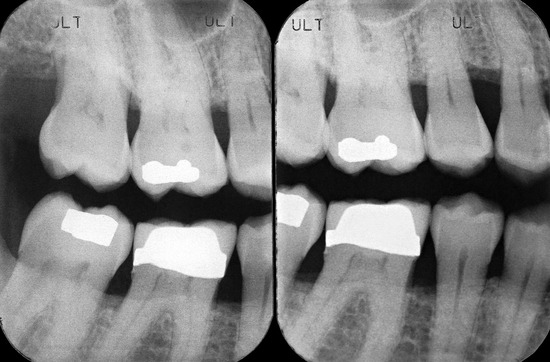
Periapical radiographs provide excellent images of whole teeth, bone trabeculae, and surrounding dental structures and gums; such radiographs also supply detailed information on small sections of the buccolingual width and the occlusoapical height, so that the available bone can be observed and measured with minimal distortion (Figure 6-1).
Radiographic film in a protective casing is placed in the patient’s mouth and normally is held in position behind the teeth to be x-rayed. This procedure can present certain difficulties if the patient has a very sensitive gagging reflex. Correct positioning of the film is more difficult in edentulous regions of the mandible, where the floor of the patient’s mouth can be very shallow and not deep enough to give room for placement of the film other than above the edentulous mandibular ridge. In addition, the presence of anatomical variations (such as mandibular tori) makes this procedure difficult. If the implant position has not been determined, the film should be placed parallel to the lingual cortical plate bone, because angulation of the implant osteotomy is sometimes dependent on this structure.10 The specific needs and treatment objectives of the patient, as the literature notes, determine the radiographic imaging choices made by the clinician for the planning of implant placement in this and similar cases,11 including general dental practice (diagnostic and preventative services)12 and dental habilitation surgery.13 Biological risks to the dental patient (i.e., dose measurements) should also be a concern for the clinician in radiographic decision planning.14
Periapical radiographs, however, have a number of limitations because of the small size of the film, which restricts the view to specific sections of the dental arch. It is difficult to interpret the anatomical details that are out of the scope of this small film, and it is impossible to ensure adequate width of the bone. The restricted field of view also makes orientation difficult in completely edentulous spans.6 In addition, the location of the mandibular canal is often difficult to determine, and the mental foramen is visible in only 50% of periapical films of that region (Figure 6-2).
An occlusal radiograph can be used to visualize the mandible and maxilla in an axial view. After the film is placed intraorally parallel to the plane of occlusion, the beam is directed perpendicular to the film, above it for the maxilla or below it for the mandible. The patient’s head is oriented so that the film is taken at a right angle (90 degrees) to the mandibular dental arch.7 This view provides substantive information on the buccolingual width of the mandible, which is depicted on the film as the distance between the points located on the extreme boundaries of the buccal and lingual cortical plates. However, the three-dimensional structure of the bone, particularly in the exterior and interior areas of the mandible, is not always easy to evaluate with this type of film. The inclinations and curvatures that the mandible presents, especially in its inner aspect, will not be apparent on an occlusal film. In addition, the maxilla is often distorted on occlusal films; superimposition of structures between the nasal bones and the maxilla will be apparent on the film, and the view may be less helpful for determining the width of the arch.
Because of the stated disadvantages of periapical and occlusal radiographs, they are of limited use in implant treatment planning and are recommended as an additional evaluation tool, primarily in cases of single implant placement.15 Even for a single implant site, the periapical and occlusal films should be complements to a panoramic film. For a single site, several periapical views and at least one properly positioned occlusal radiograph should be taken to provide optimal image detail of the implant site with minimal geometric distortion. Intraoral radiographs can help the clinician estimate the approximate height of the bone, as well as the location of the proposed site relative to critical anatomic structures.16
Panoramic Radiographs
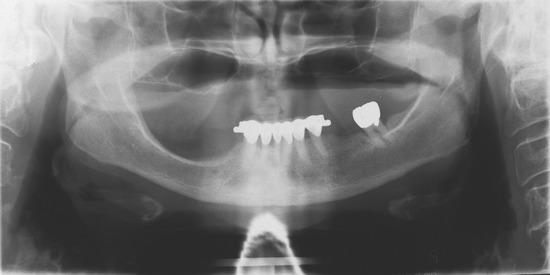
The panoramic radiograph, currently the most used radiographic modality in implant dentistry, produces a single two-dimensional image of the maxilla and mandible and their supporting anatomical structures in a frontal plane7,17 (Figure 6-3). A panoramic image is very helpful when one is planning multiple implant sites, and, when properly positioned, can provide useful information for single implant site selection; the literature suggests that limited site radiography may best be performed with intraoral radiography.18 The panoramic radiograph provides a wide-field view, whereby the gross anatomy of the maxilla and mandible, the opposing structures within the jaw, and related pathologic findings are easily identified and evaluated. Comparisons can be made to contralateral landmarks, and existing conditions (e.g., odontogenic lesions, condylar changes) that might interfere with implant placement or jeopardize the success of the procedure can be visualized.7 In addition, the vertical height of the bone can be readily assessed, and the procedure can be performed conveniently and rapidly, with minimal exposure of the patient to radiation. When a patient presents with a highly atrophic mandible, particularly with unfavorable imaging conditions, rotational panoramic radiographs can yield results more useful to the clinician than those of limited intraoral radiographs for peri-implant bone loss evaluation.19 The clinician should note that manufacturers’ instructions for positioning dentate patients during panoramic radiography may yield errors in positioning on the panoramic radiographs of edentulous patients, unless modifications are made. As with all radiographic treatment, appropriate training of dental staff is essential, as is the use of proper technique when panoramic films are exposed and developed for proper diagnosis and planning of implants for edentulous patients.20,21
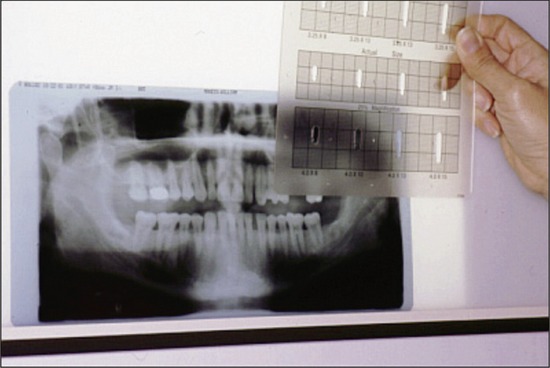
Several disadvantages are associated with the use of panoramic radiographs with regard to implantology. The image does not produce the fine anatomical resolution seen with other types of radiographs. In addition, no information is provided in terms of bone thickness, and the use of a panoramic image alone can lead to errors in estimating or determining bone width.7 Superimposition or overlapping of structures can result in poor image quality. The presence of metallic restorations, metal frameworks, or base metal implants can cause metallic artifacts and streaking to appear on the image. Nonuniform magnification is an inherent problem with panoramic films (Figure 6-4).6,22,23
The major disadvantage associated with the use of panoramic radiographs is their extreme sensitivity to errors in patient position,24–26 which can result in significant geometric distortion of the image. This distortion can be divided into vertical and horizontal components. The dimensions of the vertical image are dependent on the x-ray source as the focus, with the degree of distortion determined by the distance from the patient’s arch to the film. The horizontal dimensions are affected by the rotation center of the beam as the focus, and they change dramatically in relation to object-film distance.27 It has been reported that panoramic images can produce a 50% to 70% horizontal distortion and a 10% to 32% vertical distortion.17,28–30 This distortion factor and the inconsistency in enlargement make accurate assessment and determination of implant length based on longitudinal measurements from the panoramic radiograph extremely difficult.6
Before the advent of newer, more sophisticated imaging modalities (e.g., plain tomography, CT), surgeons had to rely solely on clinical assessment of bone width, and it was not unusual to discover during surgery that bone for implant placement was inadequate. Because of the limitations of panoramic films and the availability of adjunctive radiographic procedures, panoramic radiography should no longer be the only imaging modality used during the preoperative treatment planning phase for oral implants. Although not always commercially available when developed during the early 1990s, new technologies were being developed to create digital images from conventional panoramic radiography.31–35 Over time, these innovations helped to decrease the procedure’s sensitivity and reduce the problems associated with patient positioning. Recent literature has shown the equivalency, in most cases, of digital panoramic radiographs and film-based images.36
Various commercially available implant systems provided templates that could be placed over the panoramic x-ray to help calculate the area that the implant would occupy in a particular site (Figure 6-5). These templates came with the implants depicted with an estimate of the magnification expected in a panoramic film. To help determine proper placement of the implants, the clinician obtained the panoramic radiograph with a surgical stent in place. A stent is a clear resin duplicate of the diagnostic wax-up of the patient’s denture, which provides information regarding optimum implant sites and desired angulation of the prosthesis.17,37 Guiding grooves or holes are placed in conjunction with cutouts or flat plane surfaces in potential implant sites, with radiopaque metallic ball bearings of known diameter luted over placement sites on the stent. On the panoramic image, the metallic spheres will appear “suspended” over potential implant sites. The distortion factor at each site can be determined by dividing the actual diameter of the sphere by its diameter on the radiographic image. The true height of the residual ridge at the site can be calculated on the radiograph by measuring the distance from the ridge crest to the superior aspect of the mandibular canal (or to the inferior border of the mandible in the symphysis region, or the inferior aspect of the maxillary sinus in the maxilla) and multiplying this result by the distortion factor.17 This information can be of considerable help in selecting the correct implant length. When the radiographic treatment planning has been completed, the ball bearings are removed and the stent is cut out and grooved for implant surgery.
Lateral Cephalometric Radiographs
Generally, lateral cephalometric radiographs are not very useful when one is planning for implant placement because of the number of superimposed images that will make visualization of the anatomical area of interest very difficult. Nevertheless, a lateral cephalometric radiograph can be used in treatment planning of implants for or near the midsagittal region of the maxilla and mandible, where the trajectory and angulation of the residual bone are well visualized.6,38 Magnification ranges from 6% to 15%, providing a more accurate representation than the panoramic radiographs of vertical height, width, and angulation at the bone at the midline. In addition, a lateral projection of the skull can help in evaluating factors such as loss of bone in the vertical dimension, skeletal arch interrelationships, anterior crown-to-implant ratio, and anterior tooth position in the prosthesis.
One technique for evaluating bony changes in the anterior edentulous maxilla involves a modification of the traditional cephalometric analysis. A comparison is made of the measurements of the patient’s initial (baseline) analysis versus the patient’s follow-up radiographic analysis; results can be used to identify bone loss amounts occurring between examinations.39 Oblique lateral cephalometric radiographs have been found to be effective for measuring mandibular height in longitudinal studies of patients with and without implants.40
This technique can be enhanced by soft tissue projection correction, which can significantly reduce the variation between radiographs caused by soft tissue positions.41 Other studies have concluded that superimposition of oblique cephalometric radiographs can be used effectively to determine tooth movement in implant cases.42
Plain (Conventional) Tomography
For implant site selection, plain tomograms provide an image focused on a selected parasagittal plane. The procedure was used initially to obtain cross-sectional views of the maxilla and mandible. Valuable information on the quality and quantity of bone at the implant site can be obtained, and the layers of cortical bone and trabecular bone and anatomical structures at the location can be accurately evaluated.43–45 The presence of adequate bone at the precise implant site can be directly measured from the tomogram.30 Some have advocated plain tomograms as the most cost-effective radiographic modality for assessing implant site.46 However, this technique has certain limitations in the treatment planning of oral implants because the distance between cross-cuts is large, the images are blurry, and the contrast is poor. Unfamiliarity of the dentist with reading conventional tomograms made of dental implant sites has been noted in the literature, and the dentist often needs aid in identifying normal anatomical landmarks on cross-sectional slices for correlation with sagittal slices.47,48 Tomograms can have as much as a 40% enlargement factor, and superimposition of structures out of the plane of focus (although not as much of a problem as with other radiographic procedures) can result in a “smearing” of the image under study.6 Plain tomography is very labor intensive when used to evaluate multiple implant sites.7
Computed Tomography
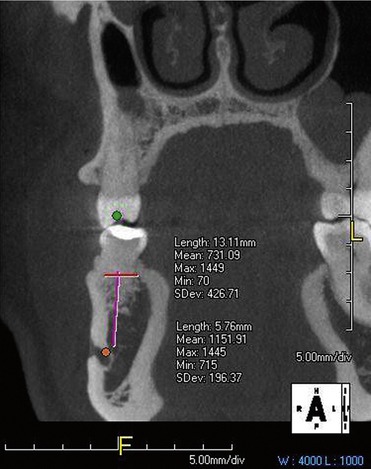
The CT scanner, first introduced to the medical field in 1972, exemplifies the significance of the computer’s contribution to medical imaging. In CT scanning, multiple beams of x-rays are passed through the body part being examined, and their degree of absorption is recorded by sensors. The scanner moves around the patient, emitting and recording x-ray beams from every point of the circle; in this way, data on the density characteristics of the object under study are obtained. Using information produced by the scanner, a computer constructs cross-sectional images of the object. These images are the visual equivalent of bloodless slices of anatomy, with each scan being a single slice. Images can be manipulated electronically to obtain the best view of the area of interest. Adjacent two-dimensional slices can be reconstructed to produce three-dimensional representations, as well as images in different planes. In this way, a CT scan can provide coronal or frontal views, lateral or sagittal views, and axial or horizontal views (Figure 6-6).
Numerous advantages have been attributed to the use of CT scans in oral implantology.49–51 Computed tomography images are rapidly processed and highly detailed, and reconstruction of the image is possible. No superimposition or overlapping of images occurs, and no distortion is seen, as with other radiographic procedures (e.g., panoramic radiographs). Automatic calculation of bone height and width and precise estimation of available bone are possible. Information pertaining to the quality of the cancellous bone and the thickness of the cortical plates is available (Figure 6-7).
Commercially available, specialized software, in conjunction with CT scans in the early 1990s, became one of the newest tools in radiographic planning in oral implantology.52–
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses