Oral Health Programs in the Community
Sherry R. Jenkins, RDH, BS, Kathy Voigt Geurink, RDH, MA and Linda M. Altenhoff, DDS
Upon completion of this chapter, the student will be able to:
• Identify oral health programs at the national, state, and local level.
• Discuss the essential public health services for oral health.
• Describe the four phases of organizing an effective community oral health program.
• Define goals and objectives.
• Explain how program goals and objectives are used in program planning, implementation, and evaluation.
• Discuss the benefits of primary prevention programs, including fluoride, sealants, and oral health education.
• Describe the importance of community water fluoridation as a public health measure.
• Identify the different funding streams and structures for obtaining dental services through public health systems.
Opening Statements
• Dental caries is a transmissible, chronic disease that can be prevented.
• School-based pit and fissure sealant programs reduce dental caries as much as 60%.
• Community water fluoridation decreases tooth decay by 29% to 51% in children and adolescents.
• Fluoride varnish applied every 6 months is effective in preventing caries in the primary and permanent teeth of children and adolescents.
• Integration of oral health into coordinated school health programs becomes a reality.
• Association of State & Territorial Dental Directors (ASTDD) develops a Basic Screening Survey (BSS) to assess the oral health of older adults.
General Health and Oral Health
The mission of public health is to “fulfill society’s interest in assuring conditions in which people can be healthy.”1 Without public health, including community oral health, society as a whole suffers because of lost productivity, decreased learning among school-age children as a result of health-related absences, and increased health care costs. Surgeon General David Thatcher, in the May 2000 Surgeon General’s Report,2 refers to dental disease as a “silent epidemic that restricts activities in school, work, and home, and often significantly diminishes the quality of life.” He further states:
National, State, and Local Programs: Role of the Health Department
National Level
• National Institutes of Health (NIH)
• Food and Drug Administration (FDA)
Essential Public Health Services for Oral Health
The core public health functions of assessment, policy development, and assurance shape the basic practice of public health at state and local levels. These core public health functions and the essential public health services (see Chapter 1) provided input into the Essential Public Health Services for Oral Health developed by the Association of State & Territorial Dental Directors (ASTDD) (Box 6-1).3 These guidelines describe the roles of state oral health programs and have been used in the development and evaluation of public health activities at the state level.
The Washington State Oral Health Coalition has proved to be an excellent means of bringing dedicated professionals together to resolve oral health issues through policy development. This coalition is also involved in continual assessment of oral health and in the assurance of oral health solutions. More than 20 different locations in Washington have established oral health coalitions, with representation from consumers, schools, community clinics, health care and dental providers, health departments, and agencies that come in contact with low-income and minority populations. Anyone interested in achieving the goal of optimal oral health for Washington residents is invited to join. The strength and unity of a coalition make this goal attainable. The Washington Department of Health and the DHHS have developed a document, Community Roots for Oral Health: Guidelines for Successful Coalitions, that is available to people interested in forming an oral health coalition to improve the oral health of residents in their community (Box 6-2).4
Assessment, Planning, Implementation, and Evaluation
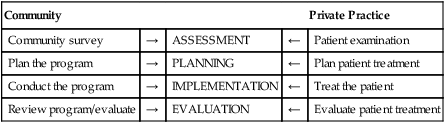
In this setting, the community is viewed as the patient. The community survey is comparable to the patient’s examination for assessment. The program plan and implementation are similar to the treatment plan and treatment of the patient. Evaluation and review of the program can be compared to the evaluation of the patient’s treatment (Box 6-3).
Definitions of the components of initiating an oral health program are as follows5:
1. Assessment is an organized and systematic approach to identify a target group and to define the extent and severity of oral health needs present.
2. Planning is an organized response to reduce or eliminate one or more problems.
3. Implementation includes the process of putting the plan into action and monitoring the plan’s activities, personnel, equipment, resources, and supplies. This step should include feedback from personnel and participants as well as ongoing evaluation mechanisms.
4. Evaluation is the method of measuring results of the program against objectives developed during the early planning stages. This process is ongoing and should identify problems and solutions to assist in revising the program as needed.
a. Formative evaluation, or the internal evaluation of a program, is an examination of the processes or activities of a program as they are taking place.
b. Summative evaluation involves judging the merit or worth of a program after it has been in operation. This step is an attempt to determine whether a fully operational program is meeting the goals for which it was developed.
These components are portrayed in the planning cycle model in Figure 3-4. The model provides a continuous cycle of steps to assess, plan, implement, and evaluate.6
Assessment
Compounding the problem of establishing the priorities of health needs is the fact that each community is unique, with its own values and ideas. If a community’s basic need for food and security are not being met, dental needs assume a low priority. An issue that often arises is the idea that if a community’s perception of needs is adhered to exclusively, actual clinical health problems may go untreated because the people are not knowledgeable about many areas of health care. The solution to this dilemma involves striking a delicate balance between negligence and overzealousness. Although it is unethical to impose one’s own perceptions on a community, it is the professional’s responsibility to inform people of existing problems and their consequences.7
Another possibility is to investigate dental surveys that have been done by other organizations. Dental surveys are conducted by professionals at dental schools, local and state health departments, and community health centers. Coordination with other agencies and organizations to know what has been done and what needs to be accomplished can prevent duplication of services.8 Data can be obtained and analyzed by various methods (see Chapter 3). After the needs assessment is performed, developing the appropriate goals and objectives is the next step.
Planning
Objectives
The performance verb is the key to a measurable objective (Box 6-4); it is an action word, such as “write,” “demonstrate,” or “recite.” Other elements of the objective are the condition, which tells under what circumstance the activity occurs, and the criterion, which tells how well the activity must be performed. The performance verb is essential in writing a measurable objective. The inclusion of a condition and a criterion makes the objective more specific and useful to the learner. In summary, the objectives should include the following:
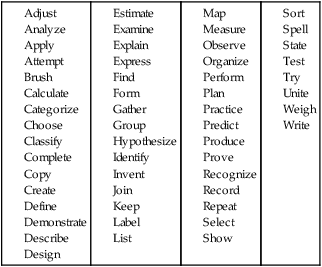
1. A performance verb tells the activity and outcome.
2. A condition tells under what circumstance the outcome will occur.
3. A criterion tells how well the action and outcome must be accomplished to be effective.
Implementation
The process of putting the plan into action, the implementation phase, is ongoing and should be supervised and evaluated to ensure program effectiveness. Implementation, like planning, involves individuals, agencies, and the community working together. The strategy should answer the following questions8:
Evaluation
Inherent in this approach is the possibility of attaining a negative outcome, that is, the conclusion that the objectives have not been met. At the same time, however, this does not mean that the program has been a failure. If a program is evaluated properly so that negative outcomes become learning experiences and indicators of future programming and research, in some sense it has been a success.7 Formative evaluation during the implementation process can point out problems and identify opportunities to correct program deficiencies early on. With ongoing evaluation and change, the summative evaluation (end result) may in fact measure a program with initial problems as successful.
Program evaluation is an example of applied research. Basic (clinical) research (see Chapter 7) involves inquiry into the truth about facts, behaviors, relationships, and principles. Applied research is concerned with these same concepts but emphasizes the application of the knowledge and developing solutions to problems. For example, a basic researcher would be concerned with the effectiveness of the fluoride mouthrinse on the teeth and which concentration to use. A program evaluator would be concerned with the effect of the program operation and its ability to meet the program objectives. The fundamental purpose of program evaluation is to assist in decision making on the effectiveness of the program in its entirety and to reassess the program and make necessary changes to make the program more effective.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses