CHAPTER 6 ORAL HEALTH AND THE AGING POPULATION (GERIATRIC ORAL HEALTH)
The aging phenomenon emerges as the most significant health issue of the twenty-first century. In the coming years, the nation’s social and health institutions will continue to be challenged by changing demands for social and health services because of the anticipated growth in the elderly American population. This demographic imperative is expected to have a major impact on the dental profession and the delivery of oral health services to the older adult population, whose oral health needs differ from those of younger adults. The oral and general health status and needs of the older adult reflect a complex interaction of age-related physiologic changes, their psychosocial concomitants, and the various pathologic processes that occur with increasing frequency in aging. This chapter reviews some of the social and economic issues, as well as the biologic and psychologic considerations, that affect the oral health of the elderly. It considers what is currently known about the oral health of older adults and what the profession might expect in the future. Emphasizing the concept of the interdisciplinary team approach to care, the chapter also provides a framework for managing the oral health needs of older adults in various settings.
DEMOGRAPHIC AND SOCIOECONOMIC TRENDS1–3
Significant changes in the demographic characteristics of the older population have occurred in the past century. The size of the geriatric population, persons 65 years of age and older, increased dramatically during the twentieth century and is expected to continue to increase at a rapid pace well into the first half of the twenty-first century. The percentage of Americans age 65 and older has more than tripled, from 4% in 1900 to 13% in the year 2000; the number has increased nearly 11 times, from 3 million to 35 million individuals. As Fig. 6-1 demonstrates, the older population will continue to grow in the future. The most rapid increase is expected between 2010 and 2030 when the “baby boom” generation, persons born between 1946 and 1964, reaches age 65. By 2030 approximately 70 million older persons will represent 20% of the population.
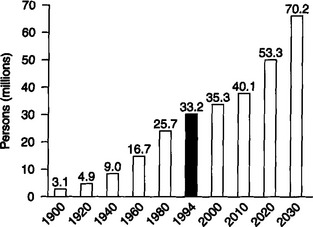
Fig. 6-1 Number of persons age 65 and older (in millions): United States 1900—2030.
(Data from U.S. Bureau of the Census.)
Longevity varies considerably with the gender of the person and is greater for American women than men. As the population ages, the distribution by sex also changes. The elderly population is composed of many more women than men. In 2000 women accounted for 58% of the population age 65 and older and 70% of the population age 85 and older. At age 65 there are 122 women for every 100 men. The sex ratio increases with age; at 85 there are 257 women for every 100 men. Of the women over age 65, 47% are widows, and 43% are married. Of the older men, only 10% are widowers, and 77% are married. In 1998 approximately 7% of the older population was divorced, and only a small percentage, less than 5%, had never married. Marital status is a major variable that strongly affects a person’s emotional and economic well-being. It influences living arrangements and availability of caregivers among older adults with declining health and function.
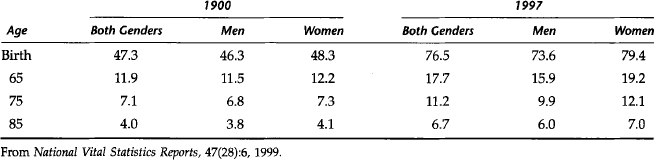
The increase in the number and proportion of the elderly in the population has been attributed to three basic phenomena: (1) the decline in the birth rate, (2) the aging of the “baby boomers,” and (3) the substantial increase in life expectancy during the twentieth century. As Table 6-1 demonstrates, the overall decline in age-specific death rates has led to increases in life expectancy at birth and also at 65, 75, and 85 years of age. The decline in mortality rate among the very old has been greater than that for any other age group. An important issue for health care professionals is the relationship between changes in the mortality experience of the elderly population and coincident changes in the underlying morbidity and disability experiences. Will future increases in longevity be associated with prolongation of dependency? Or will active life expectancy increase as health promotion and disease prevention strategies for the elderly become increasingly more effective?4 Currently, an argument can be presented for either view.
AGING, FUNCTION, AND DEPENDENCY
Aging can best be viewed as a biopsychosocial process in which changes occur at various levels in all three components of the biopsychosocial system.5 From the biologic perspective, gradual declines in the physiologic reserves of most major organ systems begin during the fourth decade.6 An increasing probability of specific age-related diseases also contributes to the loss of physiologic reserves. Within the psychologic component, age-associated alterations in perceptual and cognitive capabilities also occur.7,8 From the social perspective, the elderly are faced with different societal attitudes and are confronted by a higher likelihood of losses within their support network because of retirement or the deaths of family and friends.9 From a clinical standpoint these changes become most significant when they break through the clinical threshold and begin to impair the functional status of the individual.5 Because of the great variability in functional status among people age 65 and older, addressing the health needs of older adults according to their level of function is more appropriate.
The most common way of assessing functional capacity is evaluating limitation in activities of daily living (ADLs) and instrumental activities of daily living (IADLs), which generally indicate an inability to live independently.10 ADLs include bathing, dressing, eating, transferring from bed or chair, walking, getting outside, and toileting. IADLs include preparing meals, shopping, managing money, using a telephone, and doing housework. It is apparent that ADL and IADL levels affect the older adult’s ability to access and maintain oral health care.
Several scales are used to determine the level of orientation, memory, and cognitive ability.11 The most commonly used scales are the Short Portable Mental Status Questionnaire (SPMSQ) by Pfeiffer, the Mini-Mental State by Folstein, and the Mental Status Questionnaire by Kahn.12–14 These brief mental status screening tests can be administered in a dental setting as part of the mental assessment of potentially impaired patients. Poor scores usually indicate an increased probability that a cognitive or dementing disorder is present. Although screening test scores alone do not measure presence of a disorder, they will alert the dental practitioner to request a comprehensive medical evaluation.
The conditions that most frequently cause disability among the elderly are of two kinds: those that are also the leading causes of death, such as heart disease, cancer, and cerebrovascular disease; and chronic conditions that are generally nonfatal, such as dementia, arthritis, orthopedic impairment, visual impairment, and hearing impairment.15
Although more than four out of five people age 65 or older have at least one chronic health condition, their disability ranges from minimal problems to total dependence.10 Table 6-2 lists the prevalence of selected major chronic conditions among older adults. Based on their functional status and level of dependence, older adults have been described as being either independent, frail, or functionally dependent.16 Independent older adults are those who reside in the community and require no assistance in their necessary ADLs. These individuals make up 80% of the elderly population and are able to access dental care as would younger individuals. The frail elderly have chronic debilitating physical, medical, and emotional problems and are able to maintain some independence in the community only with assistance. Approximately 10% to 15% of the elderly are frail and dependent on various support services. Most of these individuals reside in the community; a small percentage are institutionalized. The functionally dependent are those who are seriously impaired and unable to maintain themselves. Approximately 5% to 10% of the elderly are unable to function independently and are either homebound or institutionalized. Based on the functional status and level of dependence, oral health status, dental needs, utilization of services, and mode of delivery vary from group to group. The present dental care delivery system is least effective in caring for the homebound and institutionalized segment of the elderly population, and they remain the least served.
Table 6-2 Prevalence of Selected Major Chronic Conditions among Older Adults—United States, 1995
| Condition | % Older Adults |
|---|---|
| Arthritis | 48.9 |
| Hypertension | 40.3 |
| Hearing impairment | 33.2 |
| Heart disease | 30.8 |
| Visual impairment | 18.1 |
| Cancers | 17.9 |
| Selected respiratory diseases (chronic bronchitis, asthma, emphysema) | 13.8 |
| Diabetes | 12.6 |
| Cerebrovascular diseases | 7.1 |
From CDC/National Center for Health Statistics, 1995 National Health Interview Survey.
The elderly can also be characterized according to the historical, cultural, and social events in their lives, as well as their past experiences with the dental care system.17 Accordingly, the “young old,” individuals between 65 and 79 years of age, are better educated, more politically aware, and more demanding of health services. Having somewhat benefited from the availability of fluoride and prevention, they have retained more of their teeth and have been using dental care services at a higher rate than their older cohorts. Characteristically, the “old old,” individuals age 80 and older, have experienced dentistry in an era of mass extractions. Consequently the majority of this cohort is edentulous and still believes that losing one’s teeth is an inevitable consequence of aging. They are more likely to suffer from medical conditions and to be on medications that affect their oral health. They have grown up with the notion that dentistry is a luxury and therefore tend to be infrequent users of dental services. In addition, the second decade of the twenty-first century will witness the emergence of a yet more vigorous young old cohort—the aging baby boomers of today. Being better educated, having benefited from the availability of fluoride and prevention throughout their entire lives, and having experienced less tooth loss than their parents, they are expected to be more frequent users of oral health care services and more aggressive and demanding of sophisticated care.
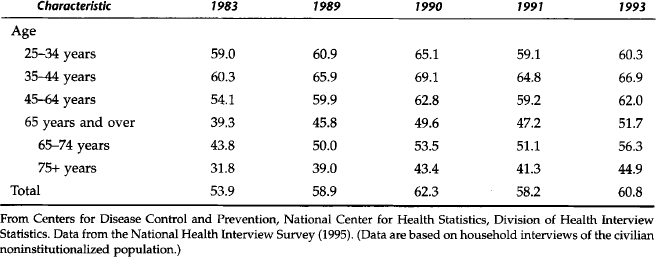
USE OF DENTAL SERVICES
Table 6-3 demonstrates the steady increase in the use of dental services by the general population over the past two decades. The percentage of the general adult population reporting use of dental care during the previous year increased from approximately 53.9% in 1983 to 60.8% in 1993.3,18 Similarly, in 1993 approximately 51.7% of persons 65 years of age and older reported using dental care compared with 39.3% in 1983. However, this proportion is still below the Healthy People 2000 target of 60%. The mean numbers of visits per person per year for all individuals age 65 years and older have also increased, from 0.8 to 2.1 visits between 1957 and 1989.19,20 The increase in the utilization of dental services by the older population has not been attributed to changes in the dental delivery system, but is more indicative of changes in the socioeconomic status and dental profile of the younger cohort of older adults.
Table 6-3 Persons (%) with a Dental Visit within the Past Year among Persons 25 Years of Age and Over, according to Selected Age Groups: United States
However, with the possible exception of children under age 6, the elderly, as a group, still have the lowest utilization rate of dental services.21 Studies also indicate that reported dental care use among minority elders has not increased parallel with elders of all races and ethnic origins.22 Given the expected future growth in minority elders, attempts should be made by the profession to identify and alleviate barriers to care and to improve access to necessary dental services.
The low utilization of dental services cannot be explained solely by conventional sociodemographic variables such as age, gender, ethnicity, residence, education, and income. They tend to interact in a complex pattern with other factors, particularly attitudinal factors.23 Schou23 divided the factors reported to directly and indirectly influence older persons’ utilization of dental services into four main categories: (1) factors related to ill health, (2) sociodemographic factors, (3) service-related factors, and (4) attitudinal or subjective factors. The variables most frequently found within these four categories are listed in Box 6-1.
BOX 6-1 Factors Influencing Older Persons’ Demand for and Utilization of Dental Services
From Schou L: Oral health, oral health care, and oral health promotion among older adults: social and behavioral dimensions. In Cohen LK, Gift HC, editors: Disease prevention-sociodental sciences in action, Copenhagen, 1995, Munksgaard.
Munksgaard
Studies comparing users and nonusers of dental services often report the dentate status of the elderly as one of the most significant factors related to utilization of dental care.24–28 The 1985—1986 National Institute for Dental Research (NIDR) survey discovered that among 5000 well elderly, approximately 55% of the dentate elderly had visited a dentist within the past 12 months. Only 13% of the edentate elderly had seen a dentist over the same period. The well dentate elderly used the services of a dentist at approximately the same rate as working adults and the population as a whole.29 Use of dental services seems to be highly related to presence of teeth. When dentate status is controlled, visit rates are similar between older and younger persons.
Poor general health and functional limitation have been reported as barriers to seeking oral health care by institutionalized and frail homebound elderly.30,31 Other studies, however, have shown that variables such as functional impairment and the presence of health problems are not as conclusive in predicting or explaining utilization behavior in the elderly; presence or absence of teeth remains the key factor in utilization of dental care.32,33
The traditional barrier, cost for services, was found by Kiyak34 to have only a slight influence on the utilization rate of care in the elderly. The same investigator suggested that lack of perceived need is the primary reason for not seeking dental care.35 This was confirmed in a study by Tennstedt and colleagues,28 who reported that one fourth of nonrecent dentate users and only 5% of all dentate subjects cited treatment cost or lack of dental insurance as a problem. Although these elders, consistent with other findings, cited a lack of need as the most frequent reason for nonuse of dental care, clinical examinations provided objective evidence of the need for treatment in the dentate subjects. These investigators concluded that lack of importance attributed to oral health and perceived need for oral health care are significant barriers to utilization. This finding underscores the importance of oral health promotion and education in the older adult population.
Because perception of treatment needs affects utilization of services, the discrepancy between actual and perceived need for treatment is a major concern. Treatment needs are generally described in terms of professionally established clinical criteria. The elderly, however, have different standards in evaluating their oral health status and tend to have different expectations for the outcomes of therapy. Because oral health status is influenced by clinical, socioeconomic, and behavioral factors, need assessment cannot be based solely on clinical measures. To improve assessment of needs in older persons, a better understanding of the role of social and behavioral factors is needed.23
The use of dental services by the elderly is also partly determined by the education and attitudes of dental professionals. Surveys of dental professionals indicate that many have little or no training in geriatrics and most accept popularly held aging myths.36,37 Surveys on dental education reveal continuing efforts at both the predoctoral and postdoctoral levels to remedy this situation. The lack of geriatric sophistication by dental professionals often results in dental offices that are poorly located or poorly designed for the purpose of accommodating the needs of the elderly. Adequate nearby parking is often missing. Ramps to assist those who are physically disabled or hallways of sufficient width for the passage of wheelchairs may not be provided.38,39 Many professionals believe that the elderly or the chronically ill cause discomfort for other patients. Treatment of the elderly is perceived as being more difficult and more time-consuming than treatment of other groups. The enactment of the Americans with Disabilities Act is expected to lessen some of these barriers to care encountered by the functionally disabled elderly.40 The law requires that private dental offices serve persons with disabilities and that dentists make reasonable modifications to facilitate access to dental offices.
DENTAL DISEASE AND ORAL HEALTH STATUS
The pattern of dental disease in the older population has changed over the past 40 years. However, the epidemiologic literature describing the oral health status of older Americans is limited, especially regarding the oldest old (age 85 and older). Although older adults were sampled in national surveys such as the 1960—1962 National Health Examination Survey (NHES) and the 1971—1974 National Health and Nutrition Examination Survey (NHANES), individuals over age 79 were not included in NHES, and NHANES III was the first NHANES to include persons age 75 years and older.41–43 The 1985—1986 NIDR survey included a sample of adults between 65 and 99 years of age who attended senior centers, but the sample was not representative of the entire older adult population.29 Regional studies among rural elderly Iowans, elderly in North Carolina, and the New England Elders Dental Study have contributed to knowledge of the epidemiology of dental disease in the elderly and further documented the change in oral disease pattern.44–48
Tooth Loss
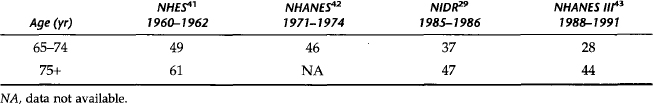
Despite the general decline in edentulism over the last four decades, 10.5% in the total adult population, the prevalence of edentulism is still high in the older population.43 Approximately 30% of noninstitutionalized persons age 65 and older are edentulous.3 Table 6-4 demonstrates the consistent decline in edentulism in this age group; however, rates of total tooth loss still exceed the Healthy People 2000 target that no more than 20% of the population age 65 and older will be edentulous. Edentulism tends to increase with age and is associated with low income, less education, and minority group status. A substantial decline in edentulism is projected by 2024 for the age 65 to 74 cohort, which is the age 15 to 24 cohort in the 1974 survey, a group that has benefited from preventive activities and advances in dental treatment.49
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses