6
Odontogenic Infections, Antibiotics, and Infection Management Protocols
ODONTOGENIC INFECTION OVERVIEW AND MANAGEMENT FACTS
Odontogenic infection, when presenting as an abscess, is typically treated, when possible, with incision and drainage (I&D) of the abscess. Antibiotics, pain and fever relief using appropriate analgesics, and removal of the source of infection once the patient has stabilized (e.g., extraction of an infected tooth), are additional steps in the management of odontogenic infections.
FACTORS ASSESSED PRIOR TO ANTIBIOTIC USE
The following factors should be considered, assessed, and evaluated prior to prescribing antibiotics:
- Infection presentation: Determine if the infection is localized or generalized.
- Know the specific organism(s) involved.
- Find out how long the patient has been symptomatic.
- Specific antibiotic facts: Know the half-life, therapeutic window, spectrum of activity, and mechanism of action of the antibiotic. Know if the antibiotic is bactericidal or bacteriostatic. Know where the antibiotic is metabolized and cleared. Know the appropriate dosage and duration of the antibiotic you plan on prescribing. Know the drug-drug interactions (DDIs) between the patient’s medications and the antibiotic prescribed, along with the antibiotic side effects, and the immune system status of the patient.
- Know the patient’s current liver and kidney status.
- Have in place the mechanisms to maintain the intestinal flora during the antibiotic intake.
- Advice on the water or fluid consumption needed or required with the antibiotic intake. Know if the antibiotic will be affected with food intake.
- Consider what negative effect an antibiotic prescription causing severe, persistent vomiting, and/or diarrhea will have in the presence of combined oral contraceptive pill (COCP) intake by the patient.
- Know which antibiotic to use during pregnancy or during breast-feeding.
ODONTOGENIC INFECTIONS: ORGANISMS AND DURATION OF INFECTION
Odontogenic infections usually have a mixed aerobic and anaerobic flora. The most common isolates are gram-positive aerobes, particularly alpha-hemolytic streptococcus. Other isolates include some gram-negative aerobes and a variety of gram-positive and gram-negative anaerobes. Aerobic bacteria are the main isolates in cellulitis-associated infections. The main isolates from abscesses are anaerobic bacteria, particularly bacteroides. In early infections or infections symptomatic for less than three days, the bacteria are predominantly aerobic and gram-positive streptococcus viridans or alpha-hemolytic streptococcus. These organisms respond extremely well to penicillin, clindamycin (the choice for penicillin allergic patients), or cephalosporins. Penicillin VK is the first drug of choice for early infections in the non-penicillin allergic patient. Clindamycin or cephalexin (Keflex), are alternate first-choice, early infection drugs, in a severe and mild-moderate penicillin-allergic patient, respectively. As the infection lingers, the patient’s defenses take over and the flora changes from being aerobic to becoming anaerobic. Anaerobes are therefore associated with late infections or infections symptomatic for more than three days. Staphylococcus aureus predominates in late infections. However, occasional isolates in early oral infections can also show the presence of staphylococcus aureus. Patients with staphylococcus aureus infection respond extremely well to clindamycin and poorly to penicillin. Clindamycin is the treatment of choice for late odontogenic infections. Clindamycin has also replaced erythromycin as the drug of choice for patients allergic to penicillin, due to increased bacterial resistance to erythromycin and the increased frequency of CYP3A4 associated DDIs with erythromycin, especially in the medically complex patient that is taking multiple medications.
Periodontal infections are often polymicrobial and anaerobic bacteria predominate. Peri-implant disease is mostly plaque-induced, and bacteria, when isolated, are similar to those associated with periodontal infection. An aerobic flora comprising streptococcus viridans or alpha-hemolytic streptococcus is most commonly associated with dental caries. Dental pulp involvement is associated with a more anaerobic flora. Gram-negative bacilli are more likely to be associated with periapical infections.
Odontogenic Infection and Associated Antibiotic Management Protocol
Infection symptomatic for fewer than three days:
- Immune-competent patients: Start with pen VK/clindamycin (for the penicillin-allergic patient). Use amoxicillin instead of pen VK in the immune-compromised patient.
- Switch to clindamycin (first choice), azithromycin, clarithromycin, penicillin VK, and metronidazole (in the immune-competent patient), or amoxicillin and metronidazole (in the immune-compromised patient), if there is no response in 24–48 hours. Clarithromycin is also associated with CYP3A4-related DDIs, similar to erythromycin, so my recommendation is to restrict the use of clarithromycin at all times in the medically complex patient who is taking multiple medications.
Infection symptomatic for more than three days:
- Start with clindamycin (first choice).
- Azithromycin, clarithromycin, or pen VK, and metronidazole (in the immune-competent patient); amoxicillin and metronidazole (in the immune-compromised patient) are alternate drugs if clindamycin cannot be used.
Periodontal infections:
- Amoxicillin, clindamycin, metronidazole, doxycycline, and tetracycline are antibiotics commonly used for treatment of periodontal infections.
Odontogenic Infection Types
Odontogenic infections can be localized or generalized. Localized infections can present as a dry socket causing pain, swelling, and redness, or as an abscess/localized pusforming process that can cause fever, malaise, mild prostration, and localized lymphadenopathy.
Generalized/spreading infections can spread into anatomic sites causing cellulitis and septicemia. The patient presents with rapidly progressing fever, chills, malaise, and tachycardia; diffuse swelling at the site of infection; moderate-to-severe prostration; and lymphadenopathy. Always assess the mental status of the patient and patient interactiveness. A spreading infection can be associated with a non-interactive patient status. Also assess the respiratory status in the presence of a generalized infection. Ludwig’s angina compromising the sublingual and submandibular spaces should be considered if the patient is experiencing breathing difficulty. Swelling around the eyes or a generalized swelling of the face is localized cellulitis that has the potential for spreading.
Symptoms, Signs, Patient Immunity, and Vital Organ Status
Oral infections cause pain, fever, malaise, minimal-to-significant swelling, and erythema. If the infection is localized and the patient’s immunity is adequate, incision and drainage (I&D) and pain medications are all that is needed. Avoid antibiotic use in the absence of fever and facial swelling, as the patient’s immune system is very capable of eradicating the infection, following I&D. This practice also reduces the potential for future antimicrobial resistance. I&D of an abscess improves circulation to the infected tissues and improves the delivery of the minimum inhibitory concentration of the antibiotic to the area, when prescribed. Antibiotics are definitely needed to treat an infection when adequate drainage cannot be achieved, the patient is significantly symptomatic, the infection is spreading (cellulitis) and/or compromising the airways, there is significant lymphadenopathy, and/or the patient is immune compromised. The antibiotic selected should match the organisms that need to be targeted. The practitioner must focus on the patient’s immunity and implement the absolute neutrophil count (ANC) guidelines in patients presenting with leucopenia.< ?pgbrk?> You can prescribe either bactericidal or bacteriostatic antibiotics to patients with mild or moderate leucopenia-associated ANC values. However, only bactericidal antibiotics can be used if the patient is presenting with ANC <500 cells/mm. The patient’s vital organ status or functioning capacity of the liver and the kidneys must also be assessed when prescribing an antibiotic. The liver could affect antibiotic metabolism and the kidney could affect drug elimination.
The liver is the major site of drug metabolism, and knowing how drugs are processed by the liver helps the practitioner make better prescription choices when treating a patient presenting with hepatitis or cirrhosis. Hepatic drug metabolism can be broadly classified into Phase I and Phase II metabolisms. These phases are dependent on two factors: hepatic blood flow and metabolic capacity of the liver. Most of the Phase I metabolism occurs in the cytochromes and involves a number of transformations, including oxidation and methylation, so the parent drug becomes more water soluble to facilitate renal excretion. Fluoroquinolones and flucloxacillin are antibiotics metabolized via this route, as are acetaminophen and corticosteroids. The capacity of the liver to metabolize drugs by the Phase I enzyme systems is compromised when the liver is in failure. The metabolic capacity of the liver has to be decreased by more than 90% before drug metabolism is significantly affected. Phase II metabolism includes glucuronidation and glutathione conjugation. Phase II occurs after Phase I metabolism, or it can occur on its own. Phase II metabolism can still occur even in end-stage liver failure. Drugs with first-pass metabolism in patients with decompensated liver cirrhosis require reduction in oral dosages. It is important to note that drug-induced hepatotoxicity is often poorly tolerated by patients with cirrhosis. Consequently, drugs that are metabolized by the liver and/or have potential hepatotoxicity should be avoided and are usually contraindicated in patients with chronic liver disease.
It is important to note that sometimes potentially hepatotoxic drugs may have to be used in patients with liver cirrhosis based on the clinical needs and when no other alternatives are available. The drug dosing is then individualized depending on factors like the patient’s nutritional status, renal function, and DDIs. Therefore, it is very important to frequently monitor the liver function as well.
Hydrophilic and lipophilic solubility characteristics of antibiotics (more details follow) can alter drug pharmacokinetics caused by pathophysiological changes common to critical illness. Many hydrophilic antibiotics are excreted unchanged by the kidney, and therefore elimination is limited in renal failure and dosing has to be altered. Many lipophilic antibiotics produce metabolites that require renal elimination, and these metabolites can accumulate in the presence of kidney disease. As such, it is best to be safe and use an antibiotic that clears through the kidney without involving the liver if the patient has hepatitis or cirrhosis, and vice versa, if the patient has underlying kidney disease.
The response to infection(s) largely depends on the patient’s medical status and his/her ability to ward off or fight the infection. Diabetes, chemotherapy, radiotherapy, neutropenia, status post splenectomy, chronic steroid use, systemic lupus erythematosus (SLE), HIV/AIDS, compromised hepatic/renal status, leukemia, or severe anemias, are some of the disease states where the patient may respond poorly to an infection. These systemic conditions must be simultaneously addressed and controlled with the help of the patient’s physician as you manage the odontogenic infection.
ANTIBIOTIC PHARMACOTHERAPEUTIC CONSIDERATIONS AND FACTS FOR ODONTOGENIC INFECTIONS
Antibiotics and Dose-Selection Criteria
The patient’s weight or physical characteristics should always be considered when making a decision about what antibiotic dose to prescribe. There is strong evidence that the metabolism and clearance of antibiotics can be affected by the patient’s body mass. According to current adult antibiotic dosing practices, an obese patient gets the same antibiotic dose as a very lean patient, even though the body sizes are significantly different. Just as pediatric dosing has always been guided by the patient’s body weight, adult dosing should also, for optimal efficacy, take body mass into consideration. Obesity can affect the distribution, protein binding, metabolism, and clearance of antibiotics. This issue is now gaining even more attention because of the increasing prevalence of obesity and antibiotic resistance the world over, making broad standards for antibiotic dosing no longer optimal for all body types. Significantly obese patients may actually need larger doses for an antibiotic to be effective, and underweight patients may actually need lower doses, to decrease the incidence of opportunistic infections, particularly yeast overgrowth in female patients and intestinal flora washout, which can occur with larger-than-required antibiotic doses or when antibiotics are prescribed for longer duration than necessary. When selecting the antibiotic dose, it is my suggestion that you use 140lb as a cutoff. As an example, prescribe 250mg pen VK qid/four times per day, for a patient under 140lb and 500mg qid for a patient over 140lb. Be vigilant when treating a significantly obese patient, as one such patient may not respond adequately to the >140lb dosing and may need to have a further increase in dose, as previously discussed.
Occasionally, a patient can be prescribed a loading dose of the antibiotic to achieve an effective dose in the bloodstream quickly before dropping down to a maintenance dose. This becomes particularly important when treating the patient who has a significant septic infection and/or inflammation. Loading dose is a function of volume of distribution of a drug and the desired drug plasma concentration achieved. Inflammatory mediators associated with sepsis cause damage to vascular endothelium, and fluid leaks out into the extravascular space. Loading doses of hydrophilic antibiotics such as β-lactams (penicillins and cephalosporins), glycopeptides (vancomycin), and aminoglycosides (Gentamycin) are required in presence of increased sepsis-associated extravascular space, smaller volume of distribution, and increased clearance occurring in severe sepsis. Lipophilic antibiotics have greater affinity for fatty tissue, greater volume of distribution, greater protein binding, deeper tissue penetration, and are more likely to be metabolized in the liver. With lipophilic antibiotics such as macrolides, linelozid, fluoroquinolones, and rifampicin, the inflammatory process is less important compared to underlying obesity. Thus, the obese patient will require higher than predicted macrolide dosing for targeted plasma concentration in the initial stages of sepsis. Hydrophilic antibiotics have a much lower protein binding and are more likely to be excreted unchanged by the kidneys.
Minimum Inhibitory Concentration
The minimum inhibitory concentration (MIC) is the smallest concentration of an antimicrobial needed to stop bacterial growth. The MIC needs to be maintained for a period of time to completely eradicate the bacterial infection, and, in turn, this correlates with the duration for which an antibiotic is prescribed. Most infections respond in about two days when treated with an appropriately selected antibiotic. Once the patient responds, the antibiotic should be continued for an additional two to three days to prevent rebounding of the infection. It is more common now to prescribe antibiotics for five days instead of the typical seven days, as this decrease in the duration of antibiotic intake helps preserve the normal balance and ecosystem of the intestinal flora.
Antibiotic Half-Life
The half-life of a drug determines the dosage length or time period for which the drug is prescribed. Penicillin has a shorter half-life when compared with amoxicillin or azithromycin (Zithromax). Penicillin is prescribed qid (four times/day) or q6h (every six hours), as opposed to amoxicillin, which is prescribed tid (three times per day) or q8h (every eight hours). Azithromycin (Zithromax) is taken once a day for three to five days, depending on pill strength. The effect of azithromycin (Zithromax) lasts for about seven days.
Therapeutic Window
For any drug to be effective there is a desired therapeutic concentration range at which the drug needs to be maintained. Above this range the drug becomes toxic, and below this range the drug is not effective.
Antibiotic Spectrum of Activity
Antibiotics may be classified as “narrow spectrum,” “broad spectrum,” or “extended spectrum,” based upon their range of effectiveness.
Narrow-spectrum antibiotics: Narrow-spectrum antibiotics are active against a limited group of microbes and exhibit lower toxicity to the host. The spectrum of activity includes mostly gram-positive bacteria and few, if any, gram-negative bacteria. Penicillin is a narrow-spectrum antibiotic with just these properties.
Narrow-spectrum antibiotics are used for the treatment of a specific infection when the causative organism is known. In doing so, the narrow-spectrum antibiotic does not kill as many of the normal microorganisms in the body as the broad-spectrum antibiotic would. Thus, a narrow spectrum antibiotic has the advantage of causing less superinfection and less bacterial resistance, as it deals with only the specific bacteria it targets. The disadvantages of narrow spectrum antibiotics are that they can be used only if the causative organism is identified. So if the drug is not chosen very carefully, the antibiotic may not actually kill the microorganism causing the infection. Narrow spectrum antibiotics should always be the first choice when treating oral infections that may be early/simple/infections of less than three days’ duration or late/complex/infections of more than three days’ duration, as the bacterial spectrum is frequently easy to establish by knowing the location, duration, and severity of infection. Narrow spectrum members include penicillin VK, azithromycin, clarithromycin, clindamycin, erythromycin, and vancomycin.
Broad-spectrum antibiotics: Broad-spectrum antibiotics successfully treat a wider range of both gram-positive and gram-negative systemic, enteric, and urinary tract pathogens. They tend to have higher toxicity to the host, and may be used to treat a variety of bacterial infections. They are of importance in the treatment of potentially serious illnesses where the patient can become significantly ill and/or succumb if the broad-spectrum antibiotic is not initiated quickly. Broad-spectrum antibiotics are also useful for drug-resistant bacteria that do not respond to other, narrower-spectrum antibiotics. In superinfections where there are multiple types of bacteria causing illness, this warrants either a broad-spectrum antibiotic or combination antibiotic therapy.
A clear advantage to the use of broad-spectrum antibiotics, when compared with narrow spectrum antibiotics, is that there is less of a need to identify the infecting pathogen with real certainty before starting treatment. On the other hand, a broad-spectrum antibiotic will have a more profound effect on the normal intestinal flora; there is potential for drug resistance and an increased risk of developing childhood asthma if a child has received broad-spectrum antibiotics during the first year of life.
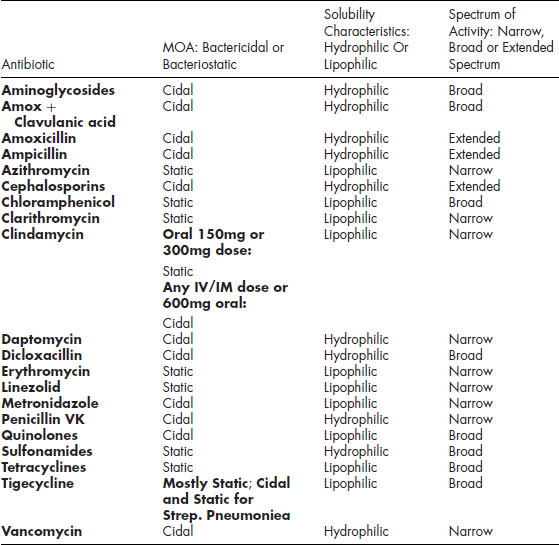
An ideal antimicrobial medication should be highly toxic to the microbe, nontoxic to the host, not interfere with the ability of the host to fight other diseases, and not lead to the development of drug resistance. Broad-spectrum members include aminoglycosides, amoxicillin + clavulanate potassium (Augmentin), amoxicillin, ampicillin, carbenicillin, cephalosporins, chloramphenicol, ciproflaxacin, dicloxacillin, levofloxacin, streptomycin, sulfonamides, and tetracyclines. Broad-spectrum members amoxicillin and ampicillin are also sometimes labeled “extended spectrum” penicillins because they are effective against almost all gram-positive organisms and some gram-negative bacteria, thus falling short compared to the other broad spectrum members, but with a wider spectrum compared to the narrow spectrum antibiotics. See Table 6.2.
Table 6.1 Antibiotics Summary
| Antibiotic: | Antibiotic Doses: Normal/Modified |
| Penicillin VK: Pregnancy Category B Strength: 250/500mg/tab |
1. Normal Dose: 250–500mg PO q6h/qid. Liver Disease: No dose alteration. Renal Dose determined using serum creatinine (S.Cr) or creatinine clearance (CrCl).
2. S.Cr. <2.0mg/dL or CrCl >50mL/min: Dispense normal dose.
3. S.Cr 2.0mg/dL to Predialysis or CrCl 10–50mL/min: 250–500mg q8-12h.
4. Dialysis: 250–500 q12-16h.
|
| Liquid Pen VK: | Liquid Pen VK is available as 125mg/5mL or 250mg/5mL strengths. Either strength can be dispensed as 5mL unit dose, available in 100mL or 200mL size bottles. Adult Rx: 250–500mg (1–2tsp, 250mg/5mL), q6h/qid x 5 days. |
| Penicillin G: Pregnancy Category B Strength: 1.2 MU/injection |
1. Normal Dose: 1.2 million units Penicillin G, IM q12h.
2. Patient with Both Liver and Kidney Disease: Use half the normal dose.
|
| Amoxicillin (Amoxyl): Pregnancy Category B Strengths: 250/500/ 875mg/capsule |
1. Normal Dose:
a. 250–500mg PO q8h or 500–875mg PO q12h x 5days.
b. Amoxicillin Oral Suspension: Powder for oral suspension is available as trihydrate in 125mg/5mL or 250mg/5mL strengths. Either strength can be dispensed as 5mL unit dose and is available in 80mL, 100mL, 150mL or 200mL size bottles.
Adult Rx: 250/500mg (1–2tsp, 250mg/5mL), q8h x 5 days. c. One-day Rx for severe acute infection: 3g or 6, 500mg capsules twice in 8 hours.
2. Premedication: 2g PO 1h prior to Rx.
3. Kidney Disease:
a. CrCl >30mL/min or a S.Cr <3.3mg/dL:< ?brk fill?> Dispense the normal dose.
b. CrCl 10–30mL/min or S.Cr >3.3mg/dL to Pre-dialysis: Prolong the interval and avoid the 875mg tablet: Give 250–500mg PO q12h.
c. CrCl <10mL/min or Dialysis: Prolong the interval and give 250–500mg PO q24h after dialysis.
4. Amoxicillin and Liver Disease: Use normal Amoxicillin dose till compensated cirrhosis. Avoid Amoxicillin use in the presence of decompensated cirrhosis.
5. Liver and Kidney Disease: Can be used. Use renal dose guidelines.< ?vsp -10pt?>
|
| Augmentin: Pregnancy Category B Strength: 250/500mg/capsule |
1. Normal Dose: 250/500mg q8h.
2. Kidney Disease: Decrease total daily dose by 50% with kidney disease.
|
| Ampicillin: Pregnancy Category B Strength: 250/500mg/capsule |
1. Normal Dose: 250–500mg q6h x 5 days.
2. Ampicillin Oral Suspension: Powder for Ampicillin oral suspension is available as trihydrate: 125mg/5mL or 250mg/5mL. Either strength is dispensed as 5mL unit dose in 80mL, 100mL, 150mL, or 200mL size bottles. Ampicillin oral suspension is also dispensed as 500mg/5mL; 5mL unit dose, in 100mL size.
3. Premedication Dose: 2g IV/IM 30 minutes prior to procedure.
|
| Dicloxacillin: Pregnancy Category B Strength: 250/500mg/capsule |
1. Normal Dose: 250–500mg qid x 5 days.
2. Kidney Disease: Use 50% of the normal daily dose.
|
| Cephalosporins: Cephalexin (Keflex): Strength: 250/500mg/capsule All Cephalosporins are Pregnancy Category B Cefadroxil (Duricef): Strength 250/500mg/capsule Ceftriaxone (Rocephin): Injection |
1. Cephalexin (Keflex):
a. Normal Dose: 250–1,000mg q6h/qid x 5 days, maximum 4g/day.
b. Cephalexin Oral Suspension: Powder for Cephalexin oral suspension is available as monohydrate: 125mg/5mL or 250mg/5mL, 5mL unit dose, available in 100mL and 200mL size bottles. Adult Rx: 250–1,000mg liquid, q6h/qid x 5 days, maximum 4g/day.
c. Kidney Disease Dose: q12h or q24h.
2. Cefadroxil (Duricef):
a. Normal Dose: 1–2g/day in 2 divided doses x 5days.
b. Cephadroxil Oral Suspension: Cephadroxil oral suspension is dispensed as monohydrate: 125mg/5mL, 250mg/5mL, or 500mg/5mL, available in 50mL and 100mL size bottles. Adult Rx: Typically, 1–2g/day liquid, in two divided doses x 5 days.
3. Premedication Prophylaxis with Cephalexin or Cefadroxil: 2g PO 1h prior to procedure.
4. Cefazolin (Ancef): 1g IV/IM 30 minutes prior procedure.
5. Ceftriaxone (Rocephin): 1g IV/IM 30 minutes prior to the procedure.
6. Kidney and Liver Disease: All Cephalosporins can be used with 50% total daily dose reduction.< ?vsp -6pt?>
|
| Clindamycin (Cleocin): Pregnancy Category B Strengths: 150/300mg/tablet Note: 150/300mg PO is a static dose; 150/300mg IV/IM is a cidal dose; 600mg PO or IV/IM is a cidal dose |
1. Normal Dose: 150–450mg q6-8h/qid PO x 5 days. Best to prescribe the lower dose, 150mg tid or q8h to minimize adverse side effects.
2. Clindamycin Oral Suspension: Clindamycin as granules for oral suspension is dispensed as palmitate: 75mg/5mL in 100mL size bottle.
2.1. Adult Rx: 2–4tsp/dose, tid x 5 days; best to dispense 2tsp/dose, to minimize adverse side effects.
3. Refractory Cases of Periodontal Infection: 600mg/day x 7 days.
4. Premedication Prophylaxis:
a. 600mg PO 1h prior to treatment.
b. 600mg, IV 30 min before procedure.
5. Hepatitis: No dose change.
6. Cirrhosis: Decrease total daily dose by 50%.
7. Kidney Disease: No dose change with kidney disease or renal failure.
8. Kidney and Liver Disease: Can be used with a 50% total daily dose reduction.
|
| Azithromycin (Zithromax/Z-pak): Pregnancy Category B Strength: 250/500/ 600mg/ immediate release tablet< ?vsp 6pt?> Clarithromycin (Biaxin): Pregnancy Category C Strength: 250/500mg/immediate release tablet; 500mg extended-release tablets, and 125/250mg/5mL granules for oral suspension. |
Azithromycin:
1. Azithromycin Normal 5-day Dose: 250mg bid or 500mg HS on day one, then 250mg/day for the next 4 days.
2. Azithromycin Normal 3-day Dose: 500mg/day x 3 days.
3. Azithromycin and Kidney Disease: No dose change.
4. Azithromycin and Liver Disease: No dose adjustments with mild or moderate liver disease and either reduce daily dose or better yet, avoid with severe liver disease.
5. Azithromycin extended-release suspension (Zmax): Dispensed as 2g/60mL. The entire 60mL is a onetime dose.
6. Oral suspension: Liquid Azithromycin is dispensed as 100 or 200mg/5mL liquid.
7. Intravenous preparation: Dispensed as ypholized Azithromycin 500mg/10mL vial.< ?vsp 6pt?>
Clarithromycin: 1. Clarithromycin Normal Dose: 250 or 500mg bid for 5 days.
2. Clarithromycin and Kidney Disease: Decrease the total daily dose by 50%. Best to avoid
3. Clarithromycin and Liver Disease: Can be used with normal dose in mild liver disease and dose reduction with moderate–severe liver disease, only if kidney status is normal.
Premedication Prophylaxis with Both: 1. Azithromycin or Clarithromycin, 500mg PO 1h prior to procedure.
|
| Metronidazole (Flagyl): Pregnancy Category B: Metronidazole is safe after 14 weeks gestation: Safety prior to 14 weeks has not been established. Strength: 250/500mg/capsule |
1. Normal Dose: 250mg q6h or 500mg q8h x 5 days. Best to give lower dose. (250mg) instead of the 500mg dose, to minimize dry mouth and metallic taste.
2. Alternate Rx for bacterial Infection: 7.5mg/kg BW (Max. 1g), q6h x 7 days.
3. “Poor Man’s Augmentin”: 250/500mg Pen VK/Amoxicillin + Metronidazole 250mg q6h or 500mg q8h x 5 days.
4. Pseudomembranous Colitis Treatment: 250/500mg q8h x 14 days. Repeat one more cycle if infection persists.
5. Kidney Failure/Dialysis: 500mg PO q12h, given after dialysis.
6. Mild Liver Disease: Normal dose. Moderate/severe Disease: Use 50% total daily dose.
7. Liver and Kidney Disease: 250mg q12h.< ?vsp -6pt?>
|
| Tetracycline HCL: Pregnancy Category D Strength: 250/500mg per capsule Doxycycline (Vibramycin): Pregnancy Category D Strength: 50/100mg per capsule |
Tetracycline HCL:
1. Tetracycline HCL Normal Dose: 250mg qid PO on empty stomach x 5 days.
2. Tetracycline and Liver/Kidney Disease: Avoid with liver or kidney disease or both liver and kidney disease.< ?vsp 4pt?>
Doxycycline: 1. Doxycycline, 100mg/capsule Normal Dose: 200mg PO 2 hours prior to bed on day one; 100mg, also 2 hours prior to bed/day for days 2–10.
2. Doxycycline, 50mg/capsule Normal Dose: 100mg PO 2 hours prior to bed, on day one; 50mg, also 2 hours prior to bed/day for days 2–10.
3. Doxycycline with Liver/Kidney Disease: Normal dose.
4. Kidney and Liver Disease: Normal dose.
5. Doxycycline Oral Suspension: Powder for oral suspension is dispensed as monohydrate: 25mg/5mL in 60mL size bottle in syrup form or 50mg/5mL, in 30mL or 473mL size bottles. Adult Rx: 100mg/200mg loading dose, followed by 50mg/100mg/dose liquid Doxycycline x 10 days.
|
| Vancomycin (Vancocin) HCL Pulvules: Pregnancy Category C Oral Vancomycin: 125/250mg per pulvule IV Vancomycin: Pregnancy Category C |
1. Vancomycin HCl pulvules for Pseudomembranous Colitis: 125mg 4 times/day x 10–14 days. Second recurrence is treated with oral vancomycin tapered over 4 weeks, with or without pulse dosing. Pulse dosing prescription: 125mg oral Vancomycin is given q2-3 days, for 2–8 weeks.< ?vsp 4pt?>
2. Vancomycin for Systemic Infections: 7.5mg/kg BW or 500mg–1 g IV q6-12h. Kidney Disease: Avoid. Liver Disease: No dose change.
|
| Tigecycline: Pregnancy Category D |
Tigecycline dose: Recommended dose is 50mg every 12 hours after a 100mg loading dose. If a patient has severe hepatic impairment, a dose of 25mg every 12 hours should be given after a loading dose of 100mg. Doses are given intravenously over 30–60 minutes.< ?vsp 4pt?> |
| Daptomycin: Pregnancy Category B |
Daptomycin Dose: Daptomycin is given at a dose of 4mg/kg IV, once daily and dose adjustment is necessary in the presence of renal dysfunction. |
| Linezolid: Pregnancy Category C |
Linezolid Dose: Adults: 600mg oral/IV, q12h; Pediatric: 10mg/kg oral/IV, q8h. |
Table 6.2 Antibiotics: Mechanism of Action, Solubility Characteristics, and Spectrum of Activity
It is best to target early infections (infection symptomatic less than three days), with penicillin VK in the immune-competent patient, amoxicillin in the immune-compromised patient, and clindamycin in the penicillin-allergic patient. It is best to treat late infections (infection symptomatic more than three days) with clindamycin, azithromycin, clarithromycin, or pen VK plus metronidazole or amoxicillin plus metronidazole, as previously discussed.
Bactericidal and Bacteriostatic Activity
Bactericidal drugs kill bacteria by inhibiting the bacterial cell wall synthesis, so bactericidal drugs kill cells that are actively growing. Bacteriostatic antibiotics are protein-synthesis inhibitors that prevent bacterial growth, and thus allow the patient’s immune system (host phagocytic activity) ultimately to eradicate the bacteria. Cidal and static antibiotics should never be prescribed together because with the cidal drugs needing active bacterial growth and the static drugs stopping bacterial growth, a cidal drug is made less effective in the presence of a static drug.
On occasion you may encounter an oral infection in a patient on a long-term, daily, single-dose antibiotic: for example, tetracycline or minocycline (bacteriostatic drugs) for acne management. You will need to prescribe a bacteriostatic antibiotic from another antibiotic family to treat the oral infection, such as clindamycin or azithromycin, which are also bacteriostatic. The newly prescribed static antibiotic can be taken along with the tetracycline/minocycline. However, a six-hour interval must be maintained between the static tetracycline/minocycline and a cidal antibiotic, such as single-dose amoxicillin that you might plan on using for premedication prophylaxis.
Another scenario for antibiotic selection could be that you encounter a patient taking the bactericidal drug trimethoprim-sulfamethoxazole (Bactrim), once every morning for Pneumocystis Jirovecii pneumonia (formally called PCP pneumonia). An early oral infection in a patient who is not allergic to penicillin can be treated with bactericidal antibiotic amoxicillin, as the patient is immune compromised. Late infections require clindamycin, but this will be incorrect as it is a bacteriostatic antibiotic that will need to be taken three or four times per day, and one of the doses will interfere with Bactrim. Alternatively, you could go ahead with amoxicillin + metronidazole or azithromycin, once per day, but given at least six hours apart from Bactrim. My suggestion is for the patient to take Bactrim in the morning and azithromycin in the evening, so both antibiotics work optimally for the patient.
Protein Synthesis Inhibitors
Bacteria have ribosomal subunits 30S and 50S. Specific bacteriostatic antibiotics selectively target these subunits. Tetracycline, streptomycin, and kanamycin target the 30S subunit; erythromycin, chloramphenicol, and clindamycin target the 50S subunit.
Antibiotic Resistance Mechanism
Bacterial resistance to the penicillins occurs through the production of beta-lactamase, which has the ability to break the beta-lactam ring structure of penicillin. This prevents penicillin from reaching its binding sites. Penicillin is ineffective against gram-negative infections because it cannot penetrate the multilayer gram-negative bacterial cell wall. Beta-lactamase stable antibiotics, augmentin (amoxicillin + clavulanic acid), and clindamycin are antibiotics that work against the beta-lactamase–producing bacteria. Clavulanic acid has the beta-lactam ring that acts as a decoy for the enzyme. The enzyme destroys this ring, thus letting amoxicillin target the bacteria.
Antibiotic Drug-Drug Interactions
The DDI could be with dietary items, as with tetracycline and metal cations. When tetracycline is taken with milk of magnesia, Tums, or Mylanta, it gets precipitated out in the gastrointestinal tract. The antibiotic does not get absorbed and never reaches the bacteria.
Antibiotics and Allergy
Always ask the patient about allergies to antibiotics. Determine whether the reaction was mild, moderate, or severe. Clindamycin is the antibiotic of choice for a patient allergic to penicillin VK or any other member of the penicillin family. The penicillins and the cephalosporins share a common chemical structure; consequently, patients presenting with severe or anaphylactoid-type allergy to the penicillins can have 5–15% cross-reactivity with the cephalosporins. Clindamycin, azithromycin (Zithromax), or clarithromycin (Biaxin) are alternate drugs that can be prescribed instead.
Antibiotics and Intestinal Bacterial Flora
Any antibiotic, when used in large doses or for prolonged periods, has the potential to eradicate the intestinal bacterial flora, cause diarrhea, clostridium difficile overgrowth, and pseudomembranous colitis. It is suggested that you always appropriately dose antibiotics, match antibiotic spectrum of activity to the type of organisms involved so the infection is rapidly eradicated, and recommend the use of probiotics or acidophilus-containing yogurt with the antibiotic, because this will maintain the bacterial flora and minimize or prevent this very untoward side effect.
Antibiotics and Water/Fluid Consumption
Always have the patient drink 6–8 glasses of water when taking an antibiotic. This will help flush the kidneys and prevent adverse effects caused by poor antibiotic clearance and accumulation of toxic metabolites. Always remember that dehydration impairs the renal clearance of drugs.
Oral Antibiotics and Oral Contraceptives
Routinely, oral contraceptives are absorbed into the bloodstream and delivered to the liver. They are inactivated in the liver and deliv/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


