Chapter 6
Minimising the Effects of Further Operative Intervention. Replace, Repair or Refurbish Failing Restorations?
Aim
Managing a failing restoration is a common clinical situation. The dilemma is often to decide which restorations require replacement and which would benefit from repair or refurbishment procedures. The aim of this section is to outline objective criteria to assist the practitioner in making these decisions. A further aim is for the practitioner to understand why restorations fail and so prevent future failures and improve outcomes.
Outcome
At the end of this section practitioners will be able to diagnose the reason that a restoration is failing and recognise restorations that can be repaired, refurbished or require replacement, and be familiar with the operative techniques associated with these procedures.
Introduction
Dental schools have, until recently, taught that restorations which did not meet certain specific criteria should be completely replaced along with any associated base and/or liner. This “drill-and-fill” philosophy, based on a mechanistic rather than a scientific approach to the operative management of dental caries, is flawed and can no longer be justified. The criteria used to assess the need to replace a restoration have not been based on evidence but upon the erroneous assumption that all marginal and interfacial defects, however small, are associated with the percolation of oral fluids along the tooth restoration interface, and that this leads inevitably to secondary caries. Consequently, practitioners in the UK spend about 50% of their chairside time replacing direct restorations that are deemed to have failed in clinical service. The reasons most commonly cited for replacing a direct restoration are as follows:
-
secondary caries as diagnosed clinically
-
marginal defects
-
bulk fracture of the restoration
-
fracture of adjacent tooth tissue
-
marginal staining or restoration discolouration
-
marginal excesses or overhangs
-
wear.
Whilst some restorations will inevitably require replacement, it is suggested that many restorations – and not least the patient – would benefit from repair and/or refurbishment procedures. It is likely that many restorations in low-caries-risk individuals have needlessly been replaced when a less interventive approach could have been applied.
Each time restorations are replaced more tooth tissue is inevitably lost as preparations increase in size and progressively become more invasive. This has an adverse effect on the dental pulp and ultimately the restored unit if the restorative staircase is followed to its ultimate conclusion. It is clearly preferable, therefore, to repair, refurbish and maintain restorations wherever possible.
Until recently, repair and refurbishment of restorations has been thought of as substandard or less than optimal care. Anecdotally, there is evidence that practitioners repair and maintain restorations on a regular basis. There is, however, little information to assist practitioners in identifying restorations that would benefit from repair or refurbishment and very little about the operative procedures associated with these techniques, let alone information about the longevity of restorations repaired in this way.
Criteria for Repair and/or Refurbishment
The selection of restorations that would benefit from repair and/or refurbishment as opposed to complete restoration replacement is based on an assessment of patient-centred and tooth-specific criteria (Fig 6-1).
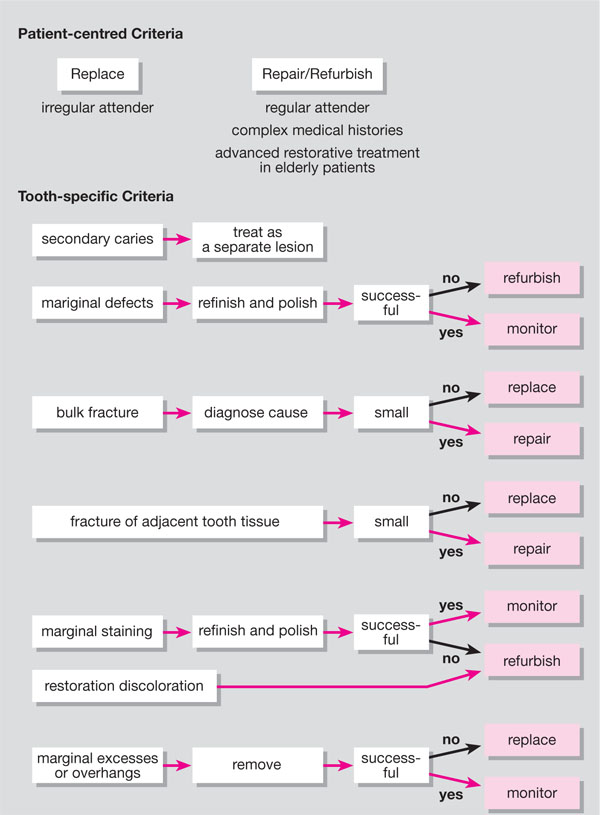
Fig 6-1 Algorithm for repairing, refurbishing and replacing restorations.
Patient-centred Criteria
Motivated and informed patients who attend on a regular basis, and in whom restorations can be monitored regularly, are good candidates for restoration repair and/or refurbishment procedures. Patients, who have complex medical histories or limited cooperation owing to learning difficulties, where treatment times and the nature of such interventions should be limited in terms of time and complexity, are especially suitable for repair and/or refurbishment procedures. Refurbishment procedures (for example, those applied to stained and/or discoloured resin-composite restorations in anterior teeth) can be accomplished in short treatment times frequently obviating the need for local anaesthesia. This can be particularly advantageous for all patients, but especially those with complex medical histories.
The management of failing advanced restorative dentistry in elderly patients is particularly problematic. Replacement of extensive reconstructions in these patients can lead to management difficulties, not least the possibility of not being able to remake the restorations or prejudicing the vitality of strategic abutment teeth. Repair, particularly of extensive reconstructions, should be encouraged in these patients wherever possible.
It is essential that patients understand the nature of repair and/or refurbishment procedures and how these procedures differ from restoration replacement procedures. In obtaining informed consent for repair and/or refurbishment procedures it is necessary to outline the disadvantages of replacement strategies in terms of their effect on the longevity of the restored unit. Similarly, the advantages of repair and refurbishment strategies in terms of the preservation of tooth tissue and their minimally interventive nature should be outlined. Further research into the prognosis and longevity of repaired and refurbished restorations is needed further to inform consent to repair and refurbishment procedures.
Patients who opt for repair and refurbishment procedures will in essence have a different pattern of care compared with those who opt for restoration replacement: regular visits for short, minimally interventive procedures, with occasional replacement procedures, as opposed to fewer, more infrequent visits, where interventions are limited to replacement procedures. It is sensible, therefore, to limit repair and refurbishment procedures to patients who attend on a regular basis.
Tooth-specific Criteria
It is important to accept that not all marginal defects in restorations require repair. Similarly, not all discoloured resin-composite restorations will require refurbishment. It is prudent to monitor such defects and not intervene until the patient is concerned, for example, about the aesthetics of an anterior tooth or where a marginal defect is causing food packing, sensitivity, soft tissue trauma, or caries is suspected.
The clinical presentations usually cited for replacing a restoration, along with how to prevent these failures and alternative management strategies, will be discussed in the next section.
Secondary caries
Caries (secondary) adjacent to the margin of a restoration should be treated as a primary lesion in its own right. As with all patients who present with a new lesion, preventive measures should be initiated primarily followed by operative intervention as and when the lesion is shown to be active and progressing into dentine and/or cavitation has occurred. Operative intervention should be limited to managing the lesion as minimally as possible, coupled with removal of the adjacent restoration only when its presence hinders successful management of the primary lesion in terms of access for effective caries removal. The need to remove all deep caries in modern-day operative dentistry has, however, been questioned, particularly when a restorative material is placed that adequately seals the preparation margins. It is suggested that the inability of amalgam to seal the margins of a preparation limits its use in this and other situations. New lesions suggest that the patient:
-
is not complying with prescribed preventive regimes.
-
has changed his/her consumption and frequency of consumption of fermentable carbohydrates (i.e. the diet is more cariogenic).
It is prudent to address these issues before proceeding to definitive treatment of caries.
Marginal defects
Visible marginal defects, which must not b/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


