6
Diagnosis and prevention of dental caries
C. Deery and K.J. Toumba
Chapter contents
6.1 Development of dental caries
6.2 The epidemiology of dental caries
6.3 Caries detection and diagnosis
6.4 Prevention of dental caries
6.4.1 Plaque control and toothbrushing
6.4.2 Nutrition and diet in caries control
6.4.3 Fluoride and caries control
6.5 Treatment planning for caries prevention
6.1 Development of dental caries
Almost all research on the process of dental caries supports the chemo-parasitic theory proposed by W.D. Miller in 1890. This is now more commonly known as the acidogenic theory of caries aetiology. The main features of the caries process are as follows.
1. Fermentation of carbohydrate to organic acids by micro-organisms in plaque on the tooth surface;
2. Rapid acid formation, which lowers the pH at the enamel surface below the level (the critical pH) at which enamel will dissolve;
3. When carbohydrate is no longer available to the plaque microorganisms, the pH within plaque will rise because of the outward diffusion of acids and their metabolism and neutralization in plaque, so that remineralization of enamel can occur;
4. Dental caries progresses only when demineralization is greater than remineralization. The realization that demineralization and remineralization are in equilibrium is key to understanding the dynamics of the carious lesion and its prevention.
One of the interesting features of an early carious lesion of the enamel is that the lesion is subsurface, i.e. most of the mineral loss occurs beneath a relatively intact enamel surface. This contrasts strongly with the histological appearance of enamel after a clean tooth surface has been exposed to acid, where the surface is etched and there is no subsurface lesion. This dissolution of the surface of enamel, or etching, is a feature of enamel erosion caused, among other things, by dietary acids. The explanation for the intact surface layer in enamel caries seems to lie in diffusion dynamics: the layer of dental plaque on the tooth surface acts as a partial barrier to diffusion. Further erosion occurs at much lower pH values (pH <4) than caries.
Dental plaque forms on uncleaned tooth surfaces and is readily apparent if toothbrushing is stopped for 2–3 days. Contrary to popular opinion, plaque does not consist of food debris; 70% is comprised of micro-organisms—about 100 million organisms per milligram of plaque. When plaque is young cocci predominate, but as plaque ages the proportions of filamentous organisms and veillonellae increase. Diet influences the composition of the plaque flora considerably, with Mutans streptococci much more numerous when the diet is rich in sugar and other carbohydrates. These organisms are particularly good at metabolizing sugars to acids.
Knowledge of the dental caries process increased considerably with the development of pH electrodes, particularly microelectrodes which could be inserted into plaque before, during, and after the ingestion of various foods. The pioneer in this area of research was Robert Stephan, and the plot of plaque pH against time (Fig. 6.1) has become known as the Stephan curve. Within 2–3 minutes of eating sugar or rinsing with a sugar solution, plaque pH falls from an average of about 6.8 to near pH 5, and takes about 40 minutes to return to its original value. Demineralization of the enamel occurs below pH 5.5, which is known as the critical pH.
The clinical appearance of these early lesions is now well recognized (Figs 6.2–6.5). They appear as a white area that coincides with the distribution of plaque. This might be around the gingival margin, as in Fig. 6.2, or between the teeth, as in Fig. 6.3. A histological section through a lesion such as that shown in Fig. 6.3 would look like Fig. 6.4 and a microradiograph would look like Fig. 6.5—the subsurface body of the lesion and surface zone can be seen clearly in both. If the process of dental caries continues, support for the surface layer will become so weak that it will crumble like an eggshell, creating a cavity. Once a cavity is formed, the process of dental caries continues in a more sheltered environment, and the protein matrix of enamel and then dentine is removed by proteolytic enzymes produced by plaque organisms.
The progression of caries is traditionally described as enamel caries progressing through to the amelodentine junction at which the enamel breaks down and a cavity forms. However, it is now understood that the process is not this simple and cavitation can occur at an earlier stage (the enamel cavity) and frequently at a much later stage when the caries has progressed significantly into dentine. Figure 6.6 shows the labial surface of a maxillary canine with a variety of stages of carious lesion ranging from white spot enamel caries to dentine cavity.
The ability of early carious lesions (‘pre-cavitation carious lesions’) to remineralize is now well understood. Periods of demineralization are interspersed with periods of remineralization, and the outcome—health or disease—is the result of a push in one direction or the other on this dynamic equilibrium. The shorter the time during which plaque-covered teeth are exposed to acid attack and the longer the time remineralization can occur, the greater is the opportunity for a carious lesion to heal. Satisfactory healing of the carious lesion can only occur if the surface layer is unbroken, and this is why the ‘pre-cavitation’ stage in the process of dental caries is so relevant to preventive dentistry. Once the surface has been broken and a cavity has formed, it is usually necessary to restore the tooth surface with a filling. The carious process is driven by the plaque on the surface and therefore it is possible to arrest the caries by effective removal of plaque even after cavitation has occurred. However, the lost tissue cannot be replaced.
Figure 6.1 Plot of the pH of dental plaque against time. This is commonly known as a Stephan curve. The curve was produced by rinsing with a 10% glucose solution. The dotted line represents a typical pH value below which enamel will dissolve (the critical pH). (Reproduced with permission from Jenkins 1978.)
Figure 6.2 Clinical appearance of pre-cavitation carious lesions on the buccal surfaces of maxillary incisor teeth (white spot lesion).
Figure 6.3 Clinical appearance of a pre-cavitation carious lesion on the mesial surface of a maxillary first molar tooth (brown spot lesion).
Figure 6.4 Longitudinal ground section through a carious lesion of the type shown in Fig. 6.3 examined in water by polarized light (magnification: 50×). (Reproduced from Soames and Southam, Oral Pathology, by permission of Oxford University Press.)
Figure 6.5 Microradiograph of a longitudinal ground section through a lesion of the type shown in Figs 6.3 and 6.4. The body of the lesion shows marked radiolucency (loss of mineral) in contrast with sound enamel and the surface layer (magnification: 70×). (Reproduced from Soames and Southam, Oral Pathology, by permission of Oxford University Press.)
Figure 6.6 Maxillary permanent canine tooth showing a variety of carious lesions ranging from white spot enamel caries to cavitated dentine caries.
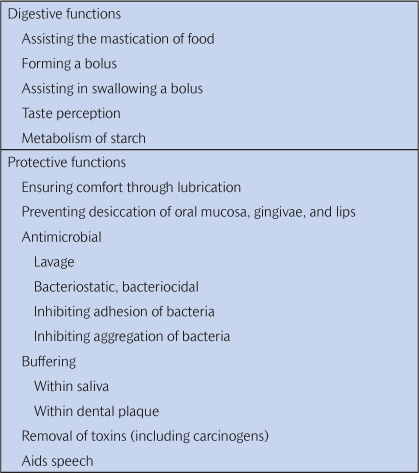
The most important of the natural defences against dental caries is saliva. If salivary flow is impaired, dental caries can progress very rapidly. Saliva has many functions, which are listed in Table 6.1. The presence of food in the mouth is a powerful stimulus to salivation, with strong-tasting acid foods being the best stimulants. Saliva not only physically removes dietary substrates and acids produced by plaque from the mouth, but also has a most important role in buffering the pH in saliva and within plaque. Fast-flowing saliva is alkaline, reaching pH values of 7.5–8.0, and is vitally important in raising the pH of dental plaque previously lowered by exposure to sugar and carbohydrates. Because teeth consist largely of calcium and phosphate, the concentration of calcium and phosphate in saliva and plaque is thought to be important in determining the progression or regression of caries. Also, it is well known that fluoride aids the remineralization process. Although it may seem sensible to try to maximize the availability of calcium, phosphate, and fluoride in the environs of the tooth, in practice fluoride is much the most important. (See Key Points 6.1.)
Table 6.1 The general functions of saliva
6.2 The epidemiology of dental caries
Dental caries is one of our most prevalent diseases and yet there is considerable variation in its occurrence between countries, between regions within countries, between areas within regions, and between social and ethnic groups. One of the tasks of epidemiology is to record the level of disease and the variation between groups. A second task is to record changes in the levels of dental caries in populations over time, and a third task is to try to explain these variations.
The UK has one of the best series of national statistics on dental caries. The dental health of adults and children has been recorded every 10 years, beginning with the Adult Dental Health Survey of 1968 (Table 6.2).
The advantages of this series of surveys are as follows:
1. They are national, using sound sampling methods to obtain representative samples of the populations.
2. They include both clinical and sociological data, giving the interaction between knowledge, attitude, behaviour, and disease.
3. The methods are well described and carefully standardized, resulting in meaningful longitudinal information.
Data on children at the ages of 5, 12, and 14 years are also available through the annual studies conducted under the auspices of the British Association for the Study of Community Dentistry and the UK National Health Service.
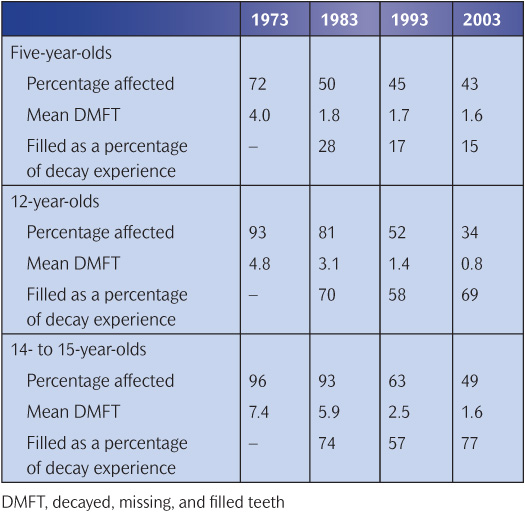
The ravages of dental caries were so severe in the past that the extent of disease in a population was measured by the proportion of the population with no natural teeth or edentulousness. A marked decrease in the percentage who were edentulous was recorded between 1968 and 2009, especially in adults aged 35–54 years. For younger people, it is common to record the prevalence (the proportion of people affected) and the severity (number of teeth affected per person) of dental caries and the percentage of carious teeth restored (Care Index). The drastic improvement in these parameters in the UK between 1973 and 2003 is shown in Table 6.3. About half of all children are now clinically ‘caries free’. What is of concern is the opinion that the improvement is not continuing in the youngest age groups, and indeed there are signs that caries experience is increasing in some areas. This is compounded by a decline in the Care Index in the UK.
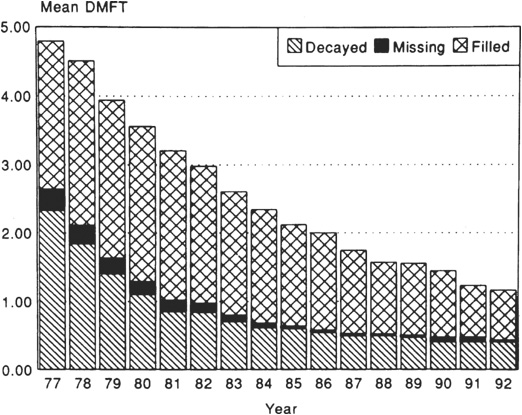
Table 6.2 National surveys of the dental health of children and adults in the UK

A decline in caries, first noticed during the 1970s, has been recorded in a large number of industrialized countries. The dental health of older children continued to improve in the 1980s, but caries experience in primary teeth, measured at age 5 or 6 years, stayed fairly constant. The Nordic countries used to have very high caries experience and the dramatic improvement in all five Nordic countries can be seen in Fig. 6.7, although it occurred somewhat later in Iceland. One of the most dramatic improvements has been recorded in Switzerland where the mean DMFT (decayed, missing, and filled teeth) in 12-year-olds fell from 8.0 in 1964 to 5.1 in 1972, 3.0 in 1980, and 1.1 in 1992. DMFT in 15-year-olds fell from 13.9 in 1964 to 2.2 in 1992. Caries experience in Australian children has been well recorded and indicates a dramatic improvement in dental health (Fig. 6.8). Reports from North America indicate that caries prevalence and severity in the permanent dentition have continued to decline since 1982 in Canada and the USA, but that caries experience in the primary dentition may have stabilized since about 1986–1987.
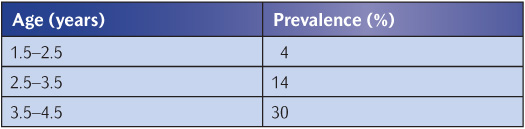
While dental surveys of schoolchildren have been quite common, there is much less information on the dental health of preschool children mainly because access to them is more difficult (Table 6.4). The prevalence and severity of dental caries in British preschool children were reviewed by Holt (1990) and in preschool children around the world by Holm (1990). In most European countries, North America, and Australia, caries experience has declined in parallel with the increasing use of fluoride toothpastes, although this decline appears to have stopped in the UK. The ChildSmile Programme in Scotland is showing promising results in terms of caries control in preschool children (McMahon et al. 2010). This programme provides more up-to-date data drawn from the West of Scotland, a region with high level of caries. In 2007–2008, 25% of 3-year-olds had obvious dental caries, with a much higher level of 32% in children from deprived areas. Caries experience in preschool children in Southeast Asia, Central America, and parts of Africa is high, and there are discernible trends of increasing prevalence in parallel with the rise in availability of sugar-containing snacks and drinks.
Figure 6.7 Caries experience (DMFT) for 12-year-old children in Nordic countries. (Reproduced from von der Fehr (1994) with kind permission of the International Dental Journal.)
Figure 6.8 Caries experience in Australian 12-year-olds. (Reproduced from Spencer et al. (1994) with kind permission of the International Dental Journal.)
While the state of the permanent dentition in children has improved dramatically in many countries, caries in primary teeth is still a considerable problem in preschool and school-aged children. In industrialized countries, caries experience is highest in the more deprived groups of society and often in ethnic minority groups. In developing countries, the reverse social trend is observed, with the well-off urban children having the most caries experience. Most of these variations in children’s dental health can be explained in terms of the preventive role of fluoride and the caries-inducing role of sugary snacks. In adults, provision of dental services and patient preference for treatments can have a major effect on the state of the dentition, in addition to the aetiological and preventive roles of sugar, fermentable carbohydrates, and fluoride. (See Key Points 6.2.)
Table 6.4 Caries prevalence in UK preschool children in 1992–1993
6.3 Caries detection and diagnosis
The presentation of caries has been described as resembling an iceberg with the dentine lesions (those traditionally described as requiring restoration) being above the waterline. Below the waterline lie enamel lesions, the most amenable to preventive intervention. Some form of additional aid is required to detect and diagnose many carious lesions. This can range from radiographs in the clinical situation to histopathology in the in vitro setting.
Caries detection and diagnosis is difficult—it is a multistage process. Unfortunately, current training of undergraduate dental students and remuneration systems frequently lead dentists just to think of the diagnostic process as a treatment, i.e. a dentinal carious lesion on the distal surface of a premolar is recorded as a DO (distal–occlusal) amalgam.
The identification of caries depends on a systematic examination of clean dry teeth. The basic equipment consists of adequate lighting, compressed air for drying, a dental mirror, and a blunt or ball-ended probe. The emphasis is on a visual examination, rather than a visual–tactile examination. The sharp probes which were traditionally used to aid diagnoses are contraindicated for a number of reasons.
• The probe does not improve diagnosis—all a ‘sticky’ fissure means is that the probe fits the fissure.
• Probing a demineralized lesion will break the enamel matrix, making remineralization impossible and thus creating an iatrogenic cavity.
• The probe may transfer cariogenic bacteria from one site to another—in effect inoculate caries-free sites with cariogenic bacteria.
A ball-ended or blunt probe can be used gently to confirm the presence of cavitation, sealants, and restorations.
The first visible sign of caries is the white spot lesion, which at first can only be seen when the surface is dried (Fig. 6.9). This is because when demineralized enamel becomes porous, the pores contain water; if dried, the water in the pores is replaced with air and the lesion becomes more obvious. As the caries progresses the lesion will become obvious even when wet.
Unfortunately, active carious lesions are not the only causes of white areas on teeth. Hypoplasia, fluorosis, and arrested hypermineralized carious lesions, to name but a few, can all mimic a white spot carious lesion. The decision as to the aetiology depends on factors such as site and surface characteristics. Caries tends to occur at predilection sites; therefore a white area at the gingival margin is much more likely to be caries than one of similar appearance at the incisal edge. Active carious lesions are matt white with a rough surface, while arrested lesions tend to be glossy with a smooth surface. A similar process is conducted for brown spot lesions.
Figure 6.9 Clinical appearance of white spot lesions on the labial and approximal surfaces of the upper permanent incisors.
Although large cavities are relatively easily identified, dentine caries presents its own problems. On occlusal surfaces there may be no visible break in the surface, the evidence of caries being shadowing under the enamel. A similar picture is seen for approximal lesions.
Therefore, as even the most thorough visual clinical examination will detect only some of the enamel and dentine carious lesions present, the clinician needs to be helped by diagnostic aids. The most commonly used are radiographs. The views which are of value for caries diagnosis are:
• bitewings
• orthopantomograms (OPTs)
• bimolars
• periapicals.
Bitewings are the first choice view for caries diagnosis. These provide information on both occlusal dentine caries and approximal enamel and dentine caries. OPTs can detect the presence of an occlusal dentine carious lesion with a high degree of accuracy. OPTs and bitewings taken in OPT machines are of much less value in the detection of approximal lesions.
Bimolars are not as useful a view as bitewings because there is often overlap of structures. However, they are of use in the pre-cooperative child who will not cope with bitewings or an OPT. Periapicals are as accurate as bitewings for caries diagnosis, but obviously less information is available on any one film.
As with the visual examination, it is vital that the radiographs are viewed in a systematic way with appropriate illumination and ideal magnification.
Although not all children will tolerate them, bitewing radiographs should be considered for all children from the age of 4 years and above who are at risk of caries. The clinician should ask the question ‘Why not take bitewings?’ rather than ‘Why take bitewings?’
The decision to take radiographs and the frequency of further radio-graphic examinations need to be based on a thorough carious risk assessment, with the dentist having to balance the benefits of the additional diagnostic yield with the risks of exposure to ionizing radiation. Current guidelines from the Faculty of General Dental Practice UK (2004) suggest radiographic examinations every 6 months for the carious-active child and views every 12–18 months for the child with controlled caries in primary or mixed dentitions (Table 6.5).
An interesting clinical phenomenon which may help the clinician decide whether radiographs are warranted is the presence of a bleeding papilla, which suggests the presence of an approximal cavity (Ekstrand et al. 1998). This occurs because the cavity is full of plaque which, together with driving the carious process, will cause gingivitis and thus the bleeding papilla.
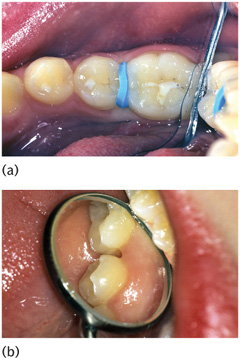
Other diagnostic aids which may assist with approximal caries diagnosis include fibre-optic transillumination (FOTI) and temporary tooth separation. FOTI consists of the placement of a 0.5mm light source in the embrasure (Fig. 6.10). If a carious lesion is present, it will show as a dark shadow. Some studies have suggested that FOTI is as accurate as radiographs, but the situation is confused by other studies which question its benefit. Certainly, if it is used, FOTI provides the clinician with more information on which to base a decision. Temporary tooth separation consists of the placement of an orthodontic elastomeric separator between the teeth (Fig. 6.11). The patient returns after 3–4 days, the teeth having separated allowing direct access for examination.
Three adjuncts have been developed to assist with the diagnosis of occlusal carious lesions: FOTI as discussed above, laser fluorescence devices, and electronic caries meters.
Laser fluorescence devices measure the fluorescence of the tooth and, of particular importance, the fluorescence of bacterial by-products in the carious lesion (Fig. 6.12). This provides a digital reading indicating the status of the surface. Research on these devices is very promising, but false readings are generated by staining, calculus, and hyperplasia. When used appropriately these devices provide a standardized reproducible measure which not only helps with the diagnostic decision but also allows the possibility of monitoring over time.
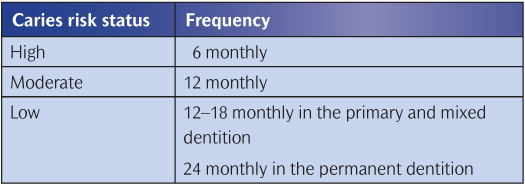
Figure 6.10 A portable FOTI light source with a 0.5mm diameter tip. As dental headpieces contain fibre-optics these are often incorporated into the dental unit.
Electronic caries meters measure the decrease in the resistance of carious lesions compared with sound surfaces. When used meticulously these meters have shown good accuracy in clinical trials. However, the readings of electronic caries meters are confounded by areas of hyperplasia, immature teeth, and particularly moisture.
The research on caries diagnosis has focused on two approaches: developing adjuncts, as discussed above, and improving the information provided by the visual examination. The use of a meticulous visual examination actually dates back to the 1950s. Currently, the International Caries Diagnosis and Assessment System (ICDAS II) delivers a diagnostic method which, with relatively little training, can provide a valid and reproducible examination that permits staging of caries from white spot to pulpal involvement.
Figure 6.11 (a) Temporary tooth separation: an elastomeric separator between a lower second premolar and first permanent molar. (b) The appearance after separation, showing access for examination of the approximal surfaces.
Figure 6.12 The tip of a laser fluorescence device in place on the occlusal surface of a maxillary first permanent molar.
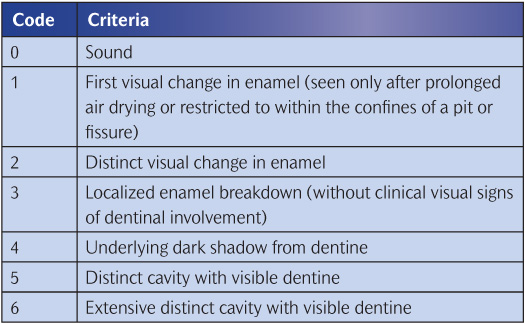
Table 6.6 outlines the ICDAS II codes and criteria, but to gain a full understanding visit the ICDAS website (www.icdas.org) which provides more in-depth information.
At present the highest-quality examination is delivered using a meticulous visual examination supported by appropriate radiographs. (See Key Point 6.3.)
Table 6.6 The ICDAS II codes and criteria
6.4 Prevention of dental caries
The dramatic improvement in dental health, especially in children, in many developed countries during the past 20 years is proof that prevention works. Dental caries is not inevitable; the causes are well known, and discouraging caries development and encouraging caries healing are realities to be grasped. Failure to do so is, at least, to provide second-class dental care.
There are four practical pillars to the prevention of dental caries: plaque control/toothbrushing, diet, fluoride, and fissure sealing. Each of these will be considered in turn before being brought together in treatment planning and in relation to c/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses








 Key Points 6.1
Key Points 6.1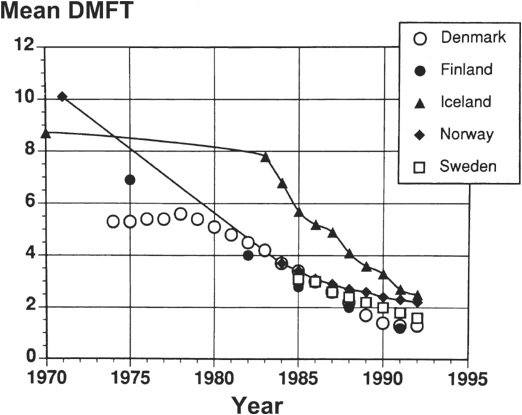
 Key Points 6.2
Key Points 6.2


 Key Point 6.3
Key Point 6.3