CHAPTER 52
Closure of Oral-Antral Communications
Brent B. Ward
Department of Oral and Maxillofacial Surgery, University of Michigan Hospital, Ann Arbor, Michigan, USA
A method of obtaining closure of oral-antral communications (OAC) and oral-antral fistulae (OAF).
Indications
- OAC over 4 mm in dimension noted intraoperatively
- OACs or OAF that persist postoperatively
Contraindications
- Defects smaller than 4 mm. Defects smaller than 4 mm frequently close with conservative treatment consisting of sinus precautions, antibiotics, and decongestants
- OAC or OAF with signs and symptoms of active infection
- Obstruction of the osteomeatal complex. Evaluation of the osteomeatal complex with a sinus computed tomography (CT) is warranted, especially in the case of recurrent fistulae. If the osteomeatal complex is obstructed, functional endoscopic sinus surgery (FESS) prior to OAF closure is indicated
General Considerations for Fistulectomy
- Circumferential fistula excision is paramount to resolution of chronic fistula formation. With care, the fistula may be excised and the medial edges approximated with sutures as a first-layer sinus closure (Figure 52.1).
- Additional tissue may be advanced for an additional one or two layers of closure, based on the size of the defect and the planned reconstructive technique.
- Suture tissue into place in an interrupted fashion.
- Consider a protective splint as indicated.
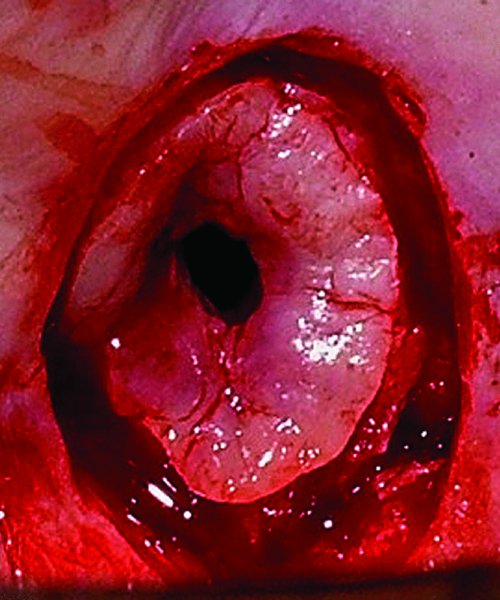
Figure 52.1. Circumferential fistula excision is performed to allow involution and closure of the fistula, and to establish closure of the nasal mucosa.
Specific Surgical Techniques for Oral-Antral Communications and Oral-Antral Fistulae
- Primary closure
- Buccal advancement flap
- Palatal rotation advancement flap
- Buccal fat pad flap
- Bone graft
- Temporalis muscle flap
- Temporoparietal galea flap
Primary Closure
Used only when tissue can be closed without tension (not specifically described).
Buccal Advancement Flap
Indication
- First-line treatment when insufficient soft tissue is available for primary closure
Contraindication
- Buccal vestibular tissue that cannot be adequately mobilized and advanced to obtain primary closure due to scarring or size of defect
Technique: Buccal Advancement Flap
- A full-thickness mucoperiosteal tissue flap is raised, and anterior and posterior releasing incisions are incorporated into the flap design (Figure 52.6). The divergent releasing incisions allow for the creation of a wide flap base and additional tissue advancement over the defect.
- Additional periosteal releasing incisions (Figure 52.7) may be incorporated as needed for enhanced flap mobility to achieve a tension-free closure.
- Adjunctive alveoplasty may be necessary to remove sharp bony ridges and to reduce the buccal plate in order to allow for additional flap advancement.
-
The buccal flap is advanced over the defect to obtain primary closure (Figure 52.10). Closure is obtained with resorbable sutures such as polyglactin (i.e., Vicryl, Ethicon Inc., Somerville, New Jersey, USA), which will maintain strength during healing.

Figure 52.2. Oro-antral communication (OAC) following posterior maxillary resection of clear cell adenocarcinoma with palatal flap outlined.
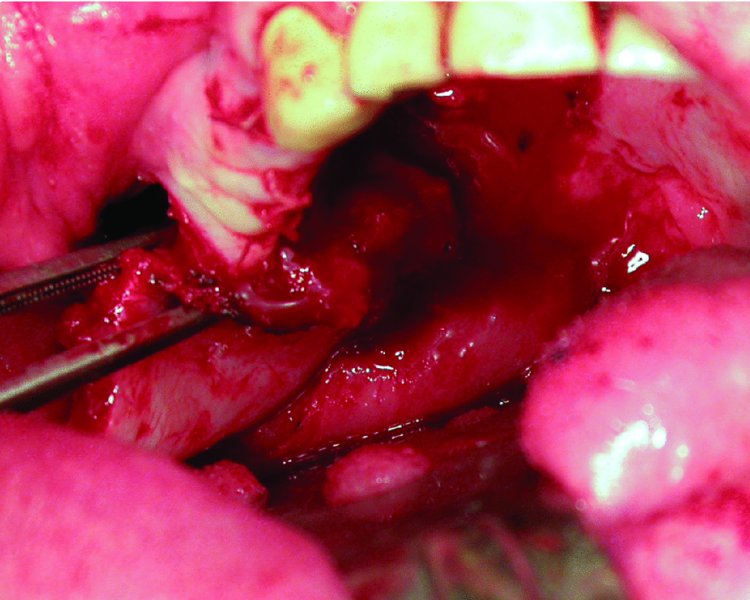
Figure 52.3. Palatal flap elevated and rotated into place.

Figure 52.4. Flap inset and closure of the recipient site with resorbable Vicryl sutures in a tension-free manner. Denuded palatal bone is visualized at the flap donor/harvest site.

Figure 52.5. Preoperative image of patient undergoing extraction of teeth #14 and #15 due to extensive decay and pain.

Figure 52.6. Oro-antral communication following extraction of teeth #14 and #15. A full-thickness mucoperiosteal tissue flap with releasing incisions is created to enable acess to the buccal fat pad and for buccal advancement flap closure.
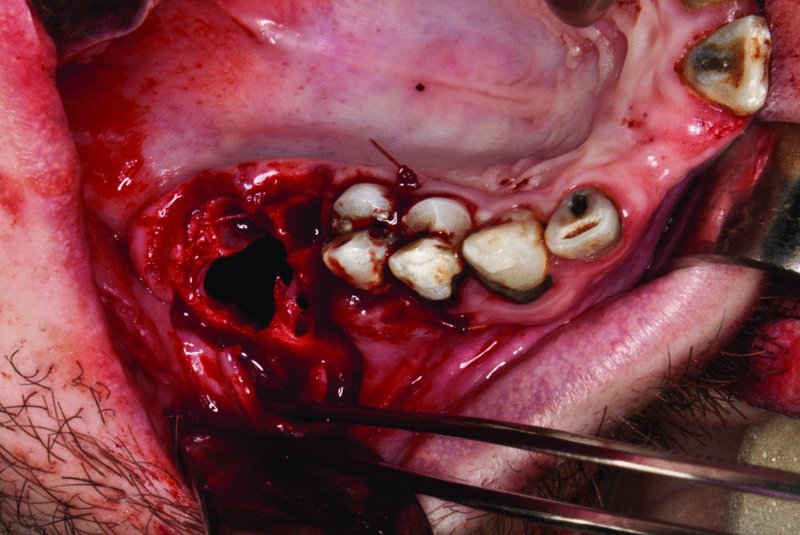
Figure 52.7. Mobilization of the buccal flap and scoring of the periosteum to allow for increased flap mobility and buccal advancement.
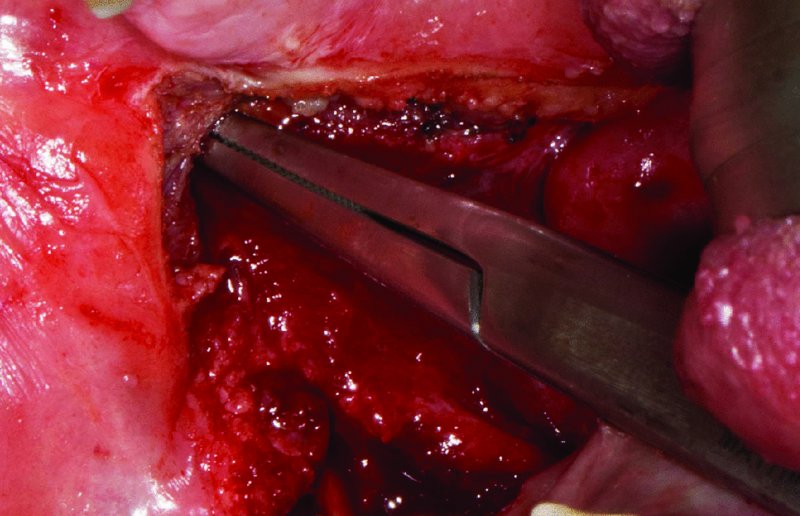
Figure 52.8. Insertion of hemostats within the area of the buccal fat pad (lateral, posterior, and superior to the maxillary tuberosity). Gentle traction is used to deliver the buccal fat pad after disrupting the interlobular septa by spreading the hemostats.
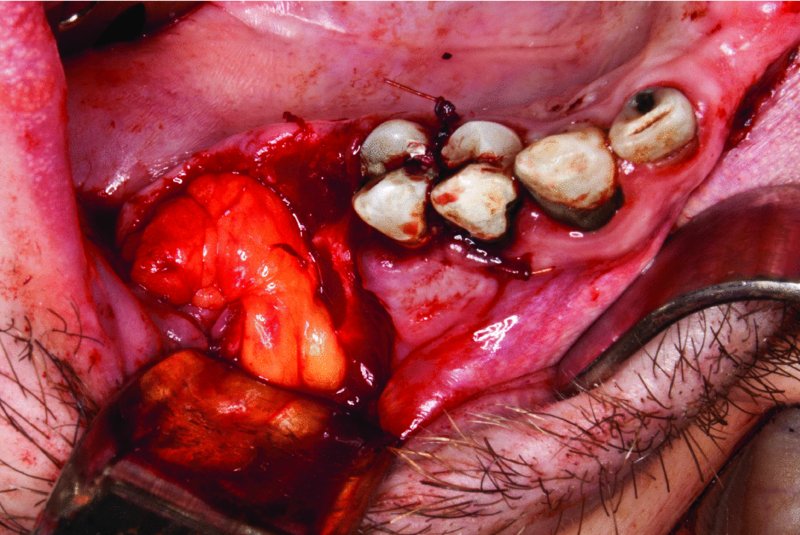
Figure 52.9. Buccal fad pad is advanced into the oral-antral communication and secured to the submucosa with interrupted resorbable sutures.

Figure 52.10. A sliding buccal advancement flap is sutured above the buccal fat pad advancement to provide a layered closure of the OAC defect.
Palatal Rotation Advancement Flap
Indication
- Secondary alternative for closure of defects with insufficient soft tissue available for primary closure
- Previously failed closure with a buccal advancement flap
Contraindications
- When the thick palatal tissue cannot be adequately mobilized for defect coverage due to scarring or large defect size
- Relative contraindication: Where previous surgeries or trauma have disrupted the blood supply of the greater palatine artery. However, random pattern flaps of the palate have been reported successful in most cases
Surgical Anatomy
The palatal flap is a full-thickness axial flap based on the greater palatine artery, which exits the greater palatine foramen. The artery courses along the lateral aspect of the palate and anastomosis with the incisive and contralateral artery, allowing the entire palate to be elevated based on a single greater palatine arterial supply. The palate consists of oral mucosa, submucosa, and periosteum, which attaches to the hard palate by Sharpey’s fibers. The soft palate consists of the tensor veli palatine, levator veli palatini, and uvula muscularis muscles. The tensor muscles pass around the hamulus, insert into the palatal aponeurosis, and may tether flap rotation.
Technique: Palatal Rotation Advancement Flap
- The greater palatine foramen and neurovascular bundle are identified by manual palpation.
- The necessary pedicle length is measured from the buccal aspect of the defect to the greater palatine foramen. The flap design is outlined with a sterile marking pen (Figure 52.2).
- A full-thickness incision is made lateral to the neurovascular bundle and carried anteriorly, up to the palatal mucosa of the central incisors, or extended to the contralateral side as necessary for the defect size and location.
- At least 1 mm of mucosa apical to the gingival sulcus is preserved.
- In the edentulous patient, the incision may extend just palatal to the alveolar crest.
- Unilateral flaps may be rotated up to 180°, allowing the flap to be positioned with the mucosal side oral or nasal.
- A full palate flap has the additional flexibility of 360° rotation, allowing the flap to fold back onto itself for oral and nasal coverage when necessary.
- When elevating a full palatal flap, the neurovascular bundle of the incisive canal must be severed and cauterized or tied.
- The full-thickness mucoperiosteal flap is raised from anterior to posterior and rotated into place (Figure 52.3). Care is taken to preserve the vascular supply of the flap.
- The flap is sutured in place with 3-0 resorbable sutures to obtain a tension-free closure (Figure 52.4).
- If further laxity is necessary to obtain passive approximation, the hamulus can be fractured, which will provide additional length to the flap. Alternatively, an island flap can be created with a circumferential incision, leaving the pedicle as the only anchor of the flap.
- A soft plastic surgical stent may be placed over the flap and denuded palate for patient comfort. Care should be taken to avoid any pressure on the pedicle. The stent is removed 7 to 10 days after surgery.
- Separation of the pedicle is usually required for small lateral defects when the flap bridges normal palatal tissue to reach the surgical site. This can be performed at 3 weeks. Prior to separation of the pedicle, verification of sufficient collateral supply can be assessed by tightly fastening a suture around the pedicle. If sufficient collateral blood supply is present, the flap will remain pink and well perfused. The pedicle may then be taken down, excess tissue trimmed, and inset at the new margin.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


