5
The Use of the Dental Endoscope and Videoscope for Diagnosis and Treatment of Peri-Implant Diseases
Thomas G. Wilson Jr.
Overview
Inflammation is frequently found around failed or failing implants. Some feel that these are infections engendered by some of the same bacteria associated with periodontal diseases [1]. Others have suggested that this inflammation is caused at least in part by a foreign body reaction [2]. An inflammatory response limited to the soft tissues surrounding implants is referred to as peri-implant mucositis. If the inflammation results in progressive bone loss, the condition is currently termed “peri-implantitis.” These two inflammatory responses are categorized under the super heading of peri-implant disease.
Chapter objectives
This chapter outlines treatments available for peri-implant diseases using minimally invasive procedures. The use of the dental endoscope in diagnosis and the endoscope and videoscope in the treatment of peri-implant disease will be emphasized. Clinical and scientific information currently available indicates that if the inflammation associated with peri-implant mucositis is diagnosed and treated at an early stage, loss of bone may not occur. It should also be understood that our understanding of these inflammatory processes is at an early stage. It should also be stated that appropriate treatment for periodontal diseases may not be totally applicable to the inflammatory responses seen around dental implants. However, current information suggests that appropriate treatment of peri-implant disease may slow down or in some cases halt further bone loss, although reintegration of the lost bone has not yet been demonstrated in humans [3]. At present, most peri-implantitis is treated in its early stages using flap surgery and in its advanced form by implant removal. However, in some of these cases, the disease can be halted or delayed in the early stages by the use of the dental endoscope alone. The videoscope is suggested for more advanced lesions.
Diagnosis and technique
The diagnosis and treatment of peri-implant diseases begins with gathering appropriate clinical and radiographic information. The current data gathering mimics that used for periodontal diseases. This means that probing depths around implants need to be measured and recorded. Signs of inflammatory changes (bleeding upon probing, suppuration, color changes associated with inflammation, etc.) should be noted and recorded. Periodic right-angle radiographs are also appropriate. Because of the relatively high incidence of peri-implant disease, it is imperative that implants be followed on a regular maintenance schedule. This will allow for the comparison of clinical and radiographic findings over time and enhance the clinicians’ ability to determine when treatment beyond routine maintenance therapy should be performed.
Treatment is currently based on the diagnosis and characterization of the inflammatory lesion. Patients who present with clinical signs of inflammation but whose probing depths have not increased and have no radiographic signs of increased bone loss are diagnosed as having peri-implant mucositis. Patients so diagnosed should have their oral hygiene reinforced, the peri-implant space (sulcus) and the implant/restorative surfaces debrided using curettes or ultrasonic devices. Attempts should be made to remove surrounding “granulation” tissue. They are usually placed on chlorhexidine rinse twice a day for 30 days. Some clinicians will elect to place the patient on 7–10 days of broad-spectrum antibiotics at this time; but in the absence of suppuration, this does not appear to be routinely indicated. Evaluation and possible treatment of any occlusal disharmonies on the implant prosthesis is also strongly suggested. The patient should be reevaluated after 30 days. If at that time continued signs of inflammation are detected, further treatment is indicated. In these cases, the use of the dental endoscope will enhance the evaluation and treatment of the subgingival environment and help elucidate the source of peri-implant inflammation.
Individuals who present with increased probing depths or radiographic signs of progressive bone loss are given a diagnosis of peri-implantitis. Aggressive treatment of the underlying cause of these clinical findings is indicated when this diagnosis is made. The endoscope is valuable in both the diagnosis and treatment of early peri-implantitis and should be employed as soon as feasible on these individuals. However in cases with significant bone loss, the videoscope provides better visibility for removal of “granulation tissue” and foreign bodies.
Endoscopic or videoscopic examination of patients with peri-implant diseases often reveals foreign material attached to the implant surface or to the prosthetic superstructure. The most common finding is a blue-gray film (Figure 5.1) attached to or surrounding the surface of the implant or its superstructure. This material is easily displaced by the tip of the endoscope explorer. It is assumed that this material is a biofilm similar to bacterial plaque found around teeth. White highly reflective material (Figure 5.1) is often seen attached to the implant or its superstructure. This material is dental cement. Subgingival calculus similar to that seen around teeth has never been observed by the author.
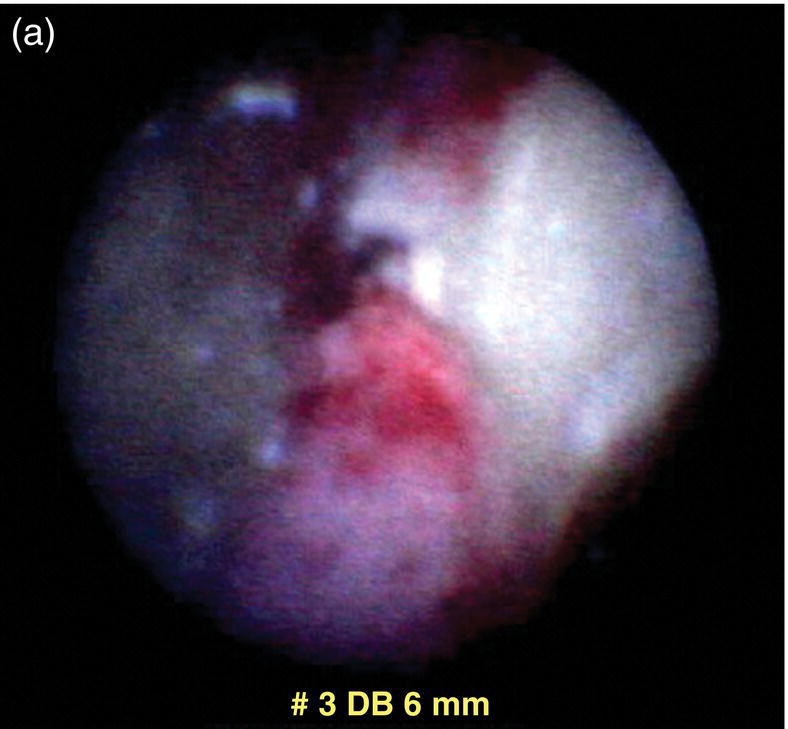
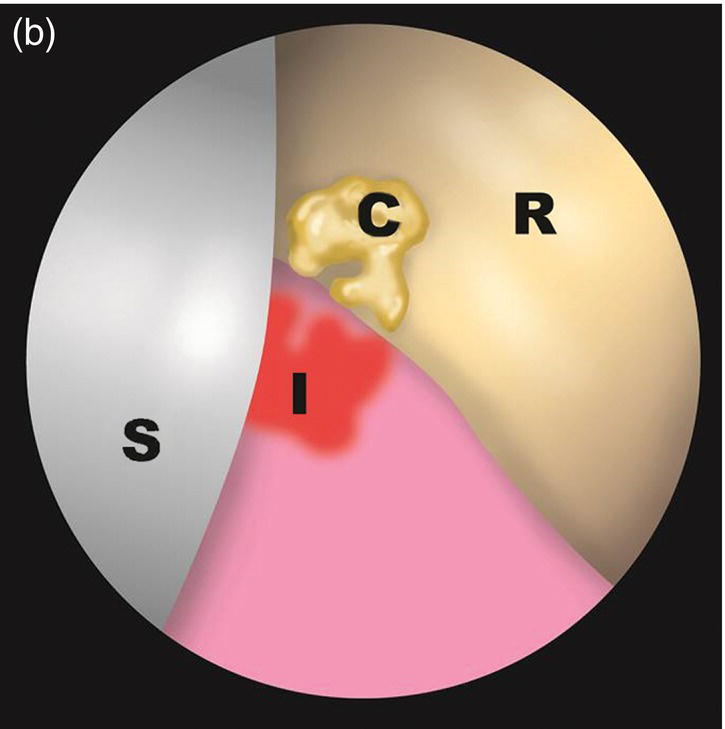
Figure 5.1 An endoscope view (a) and drawing of the field (b). Cement (C) shows up as a highly reflective white areas. Biofilm is usually blue-gray.
After inspection of the implant and the attached superstructure, the endoscopic explorer is rotated 180° and the peri-implant soft tissue (sulcular tissue) is evaluated. Foreign material is often seen in these tissues. This material shows up as very small white dots apparently embedded in the soft tissues. This material represents flecks of cement. Evaluation of human biopsies of soft tissues around implants suffering from peri-implantitis has routinely found deposits of cement and titanium surrounded by inflammatory cells [2].
The use of an endoscope greatly improves the clinicians’ ability to debride the area. Current clinical experience in the treatment of peri-implant mucositis indicates that when the endoscope is used to treat the peri-implant inflammation; in a vast majority of cases, this results in a long-term elimination of the clinical manifestations of inflammation.
Individuals with a diagnosis of peri-implantitis present greater challenges. By definition, these individuals have lost bone that is assumed to have been originally attached to the implant surface. Since reattachment of this bone (re-osseointegration) has not been demonstrated in humans, the clinician must decide on the most appropriate treatment based on the circumstances found around each individual implant. Treating early bone loss (<25% of the implant rough surface exposed) with the endoscope can often result in elimination or reduction of the clinical and radiographic signs of inflammation. It should be understood that recession of the soft tissues is likely to occur and this may create esthetic problems. In general, implants with 75% or more of the implant exposed should be removed. The quandary exists for those individuals between these two extremes.
Individuals who have greater than 25% bone loss and less than 75% bone loss can often have the progress of the disease halted (at least in the short term) by removing any implant-borne accretions and surrounding effected soft tissue. The videoscope is suggested for these procedures. This result is apparently because removal of peri-implant soft tissues reduces or eliminates the number of foreign bodies found surrounding the implant. The author’s opinion is that most surgical interventions should involve reduction of one- and two-wall bony craters, removal of affected soft tissues, and judicious smoothing of any exposed roughened surface of the implant followed by apical positioning of the flaps [3]. This is because adequate methods for removing biofilm and its products such as lipopolysaccharides from the implant surface have not yet been shown to be predict/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


