Chapter 5
The Contribution of Periodontics to Endodontic Therapy:The Surgical Management of Periradicular Periodontitis
Over the past century, surgical endodontics has been performed for treatment and conservation of teeth with persistent post endodontic treatment infections.
In 1964, with the formation of the American Association of Endodontists and establishment of endodontics as a dental specialty, surgical endodontics began to take a new face. Early on, much emphasis was placed on development of a root-end filling material that would provide a hermetic seal.
While magnification and the use of a microscope for operations date back to the early 1920s, it was not until 1984 when it was used in conjunction with an apical surgery (Reuben and Apotheker 1984). With the addition of the surgical operating microscope (SOM) to the armamentarium, the technique and outcome for apical surgeries became more conservative and predictable. After all, one cannot treat what one cannot see, and with the magnification of up to ×30 and illumination of up to ×12 with the dental overhead light, the SOM can reveal details previously unseen to the surgeon. The use of the SOM has become the standard of care in all endodontic procedures, and since 1998, all postgraduate programs in endodontics in the United States are required to train their residents to perform procedures under the SOM. As a result, instruments have been either newly designed or modified by scaling them down to a fraction of their original size to be used with the SOM. Ultrasonic tips and micromirrors were developed in the mid-1980s for the purpose of retropreparation and inspection under the SOM. Along with the introduction of new root-end filling material such as ProRoot mineral trioxide aggregate (MTA; Dentsply Tulsa Dental, Tulsa, OK, USA), the art of endodontic surgery has shifted toward endodontic microsurgery and has reached new heights in its levels of precision, predictability, and success.
Today, microsurgical endodontics is considered to be the standard of care. With the advent of SOM, microinstruments, superior retrofilling material, and more advanced hard and soft tissue management techniques, procedures are more conservative and outcomes have become more successful. Smaller osteotomy windows are made to conserve cortical bone. Root resection with shorter or no bevel angles, previously impossible due to lack of ultrasonic tips, are now feasible and conserve more root structure in order to preserve a more favorable crown-to-root ratio. The SOM allows for locating and treating isthmuses and extra portals of exit along the root’s long axis, ensuring a proper orientation and depth for the placement of a root-end filling. It also enables the surgeon to check for marginal integrity of the apical seal once it is placed. This prevents leaving avenues for leakage, which will prevent the formation of an impermeable seal and may ultimately result in treatment failure. Rubinstein and Kim (1999, 2002) reported the short-term (1 year) and long-term (5 to 7 years) success rates for endodontic microsurgery to be 96.8% and 91.5%, respectively. These results are rather impressive considering that about 60% of the surgeries were performed on premolars or molars.
TOOTH CONSERVATION VERSUS IMPLANTS
With the recent implant paradigm shift in dentistry, some clinicians have made claims as to suggest the placement of immediate load implants is a more logical treatment over treatment of the teeth via endodontics (Ruskin et al. 2005). As clinicians, we must not be easily affected or swept away by advertisements or reading one such article. Rather, our decisions for selecting treatment plans, modalities, and techniques should be made on an evidence-based approach to dentistry and its specialties. Many have attempted to overplay the success of dental implants over nonsurgical and surgical endodontic therapy. However, in a systematic review of the literature (M.K. Iqbal and S. Kim, unpublished data) there were no significant differences between root canal therapy success rates and implants. In fact, comparing the “success” rates of endodontics and implants is sometimes beyond the scope of comparing apples and oranges.
Endodontically treated teeth are evaluated for success on the basis of clinical and radiographic criteria. An endodontically treated tooth that is asymptomatic while in function and displays no periapical radiolucency is classified as a successful treatment. Implants are often evaluated for their “success” based on their survival rate. This disparity in the evaluation criteria between endodontics and implants immediately changes the “level ground” for comparison. In addition, implant studies often exclude patients who have underlying systemic diseases such as diabetes, smokers, and patients with poor oral hygiene. In certain studies peri-implantitis was not regarded as a criterion for implant failure. Also, at least presently, most implants in these studies are being placed by trained specialist.
Meanwhile, the success of endodontic therapy as evaluated by studies did not abide to the same strict patient exclusion criteria as did the implant studies. Persistent radiographic demineralization was considered to be a sign of failure. Last, the success rate of endodontic therapy as reported by such studies as the Toronto Study is based on treatments performed by dental students, general dentists, and endodontists. In 1999, American Dental Association reported that only 25% of all endodontic cases were being performed by endodontists (ADA Report 1999).
It is clear that implants have changed the face of dentistry and the way we treatment plan restoring edentulous spaces. They are a great adjunct when treatment is planned properly and when bone quality and aesthetics allow for their placement. Implants are clearly not an alternative for periodontally sound and endodontically treatable (nonsurgical or surgical) teeth. Retaining our patients’ healthy natural dentition should be our main priority as health care providers.
TREATMENT OF FAILED ROOT CANAL THERAPY
When the initial root canal therapy has resulted in a negative outcome, two revisions are possible:
- Nonsurgical retreatment aimed to eliminate bacteria from the canal
- Surgical retreatment aimed to encapsulate bacteria inside the canal
The decision as to which approach to take should be based on the level of evidence and other criteria such as the dentist’s training and experience, availability of the necessary armamentarium, and the patient’s decision based on informed consent.
Historically, nonsurgical retreatment has enjoyed a higher success rate than the surgical approach. Studies also support that in the event of a surgical approach, prior nonsurgical retreatment will increase the chance of a positive outcome (Zuolo 2000). Therefore, unless nonsurgical retreatment is not feasible due to physical, anatomical, time, or financial hardships, surgical endodontics should not be considered as the treatment of choice.
RATIONALE FOR ENDODONTIC SURGERY
Periapical surgery is performed to eradicate persistent infection/ inflammation associated with teeth with previously negative post-treatment outcome from either initial endodontic therapy or retreatment. With advancement in microsurgical endodontics, surgery should not be labeled as a last option, but it should be performed when either initial endodontic treatment or retreatment is not possible or feasibly cannot secure a better outcome. Factors such as inability to properly access the root canal system in order to adequately clean, shape, and obtain an apical seal may warrant surgery as the treatment of choice. The ability of the clinician to properly diagnose which case is suitable for surgery is as important as his or her clinical skills. It was Dr. Irving J. Naidorf who said, “A good surgeon knows how to cut, and an excellent surgeon knows when to cut” (Kim 2002).
INDICATIONS FOR ENDODONTIC SURGERY
Anatomical Challenges
In certain cases, the tooth anatomy renders itself unwilling to proper debridement and obturation, leaving a portion of canal untreated by nonsurgical methods. Teeth with canal blockages due to severe calcification or with severe radicular curvatures fall under such category.
Also, in a few cases when endodontic therapy is performed at a clinically acceptable level, symptoms may continue to persist when the apex of the root may be fenestrating through the facial cortical plate of bone. In these cases, a small surgical procedure to recontour the root end and align it within its bony housing may solve the problem.
Iatrogenic Factors
Previous endodontic “misadventures” account for the need for surgery in cases with persistent symptoms. These include but are not limited to canal blockages, ledges, perforations, separated instruments or posts, underfilled canals, and canals with dental material extruding beyond the biologically tolerant buffer zone around the anatomical apex (Figs. 5.1 through 5.3).
Fig. 5.1. Persistent inflammation associated with the mesial root of a mandibular molar with a separated instrument.

Fig. 5.2. Surgery reveals a hand file extending 3 to 4 mm beyond the root tip.

Fig. 5.3. Instrument recovery, root resection, and retrograde obturation with MTA.

In most of these cases, proper canal debridement is compromised as is the ability to properly obturate the canal and obtain a proper apical seal.
Relentless Inflammation
Previously missed and untreated canals, bifurcations, fins, and extraradicular infections often harbor bacteria and present themselves as chronically and intermittently symptomatic teeth. Apical surgery can be performed to eradicate such factors (Figs. 5.4 through 5.6).
Fig. 5.4. Persistent inflammation and symptoms associated with the mesial root of a maxillary molar due to the missed MB-2 canal.

Fig. 5.5. Apicoectomy performed in conjunction with finding and obturation of the additional canal and the isthmus between MB-1 and MB-2 canals.
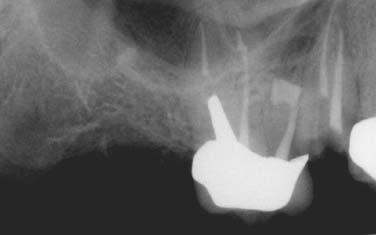
Fig. 5.6. A 4-year follow-up shows complete healing.

Exploratory Surgery
In certain cases, it may be difficult to properly diagnose a problem. In cases of root fractures, for example, a small soft tissue flap followed by dying the area in question with methylene blue and inspection under the SOM can quickly reveal a root fracture, which can then prevent unnecessary endodontic treatment to be performed on a nonrestorable tooth (Figs. 5.7 and 5.8).
Fig. 5.7. Multiple sinus tracts trace to the location of the endodontic lesion.

Fig. 5.8. An exploratory surgery and staining reveal a vertical root fracture.

Also, collection of a biopsy specimen may be another indication for performing an exploratory surgery.
CONTRAINDICATIONS FOR ENDODONTIC SURGERY
Medical History
Patients with recent myocardial infarction, with uncontrolled diabetes, patients who are under anticoagulant therapy, patients who received head and neck radiation, or patients with severe neutropenia are not good candidates for surgery. Surgery should be postponed until they are cleared by their treating physician.
Compromised Periodontium
Periodontal pockets and tooth mobility reduce the success of endodontic surgery. High success rates in endodontic microsurgery was achieved in studies where the prospective teeth did not exhibit any pathologic periodontal pocketing or pocketing that either communicated with the apical endodontic component or had completely denuded the buccal or lingual cortical plate of bone resulting in a dehiscence (Rubinstein and Kim 1999).
Skill, Knowledge, and Proper Instruments
General practitioners must be knowledgeable to properly diagnose and refer patients with surgical needs to surgeons who have the specialized training in diagnosing and treating these cases.
Although the skill levels of the surgeons should theoretically be the same, in reality this may not be the case. A study reviewed the outcome of treatment in the oral surgical and endodontics departments of a teaching hospital 4 years following surgery. Complete healing for cases performed by the endodontic unit was nearly twice as high for those performed in the oral surgery unit. The single most important contributing factor was the quality of the procedure, which in turn translated into the surgeon’s skill and perhaps level of training and understanding of the problem at hand (Rahbaran 2001).
Despite the surgeon’s highest level of clinical competence, proper instrumentation is required for achieving the highest level of technical excellence. It may sound anecdotal, but it is impractical for a world class skier to win any race while skiing on tennis rackets!
Finally, surgeons must keep the welfare of the patient in mind at all times. Case selection for surgery is very important, and indiscriminant use of surgeries to treat endodontic problems is discouraged. Remember, just because you can, does not mean you should (Figs. 5.9 and 5.10).
Fig. 5.9. Apicoectomy was performed on a “calcified” central incisor without treating the tooth by nonsurgical root canal therapy first.

Fig. 5.10. Nonsurgical root canal treatment was performed with the aid of the SOM. The tooth was free of symptoms thereafter.

Anatomical Challenges
Proximity to the maxillary sinus, mental nerve, and inferior alveolar canal and the thickness of the buccal bone in the mandibular second molar area due to the external oblique ridge may serve as a contraindication or deterrent for surgery. As long as a properly trained clinician is aware of such hurdles and conceivably knows how to work around them and manage mid-procedure and postprocedure potential complications, these factors may be downgraded to potential risks or contraindications. Extra caution or modifications in the procedure may be required in order to avoid damage to such structures.
As an example, the roots of many maxillary molars and premolars are separated from the maxillary sinus by a thin layer of cortical bone and the Schneiderian membrane. Care must be taken not to violate this space. However, in the event that the sinus is inadvertently perforated, with proper care, the membrane usually heals uneventfully, without any negative effect on the outcome of the apical surgery (Fig. 5.11).
Fig. 5.11. Osteotomy and stained resected root ends of a maxillary molar. Note the maxillary sinus and its lining deep to the root tips.

Inadequate Root Length
As a critical part of thorough treatment planning, the length of the root before surgery must be estimated. This will allow the clinician to have an understanding whether a favorable crown to root ratio is achievable once the root is resected. If the length of the root after resection is conceived to be inadequate, this may be ground for aborting the surgical procedure and looking for an alternative plan. Although, in select cases where patient is free of periodontal disease, parafunctional habits, and mal-occlusion, teeth have been known to survive with as low as 1:1 crown-to-root ratio (Figs. 5.12 through 5.14).
Fig. 5.12. Failing apicoectomy and sinus tract tracing in a maxillary second premolar.

Fig. 5.13. Conservative apicoectomy and obturation with MTA was performed despite the unfavorable crown-to-root ratio.

Fig. 5.14. Five-year recall revealed complete healing with no signs of the sinus tract or presence of mobility.

Incision and Drainage
Incision and drainage is used for treating necrotic teeth with acute apical abscess. After primary drainage through the tooth is established by performing a pulpectomy, a small incision is made at the base of the fluctuant swelling. Blunt dissection with a curved hemostat facing the bone plate is carried out to dissect tissue plains and establish further drainage. A drain must be placed for up to 48 hours to prevent wound closure. Keeping the incision site open will ensure continuous drainage and patient comfort by allowing the pressure to be relieved (Fig. 5.15).
Fig. 5.15. Incision and drainage of an intraoral abscess. Note the latex drain was sutured to prevent its premature removal.

In addition, by allowing oxygen to gain access to the site of infection, the anaerobic bacteria are killed, the balance of bacteria colony is disrupted, and the rate of healing may be accelerated.
Root Amputation and Hemisection
Root amputation and hemisection involve surgical removal and surgical division of roots of multirooted teeth. Although once performed more frequently, with the increased prevalence of dental implants, the frequency is declining. It is preferred that if a tooth is treatment planned for either of these two procedures, the root canal treatment is performed before the surgical phase. It should be noted that with proper case selection, both procedures are viable options for maintaining the natural teeth. As prudent dentists, we must subdue our urges to perform “herodontics” at all cost in order to maintain a tooth in the oral cavity. Teeth that may serve as strategic abutments, exhibit advanced periodontitis or nonrestorable remaining segment, and have fused roots or very low furcations are not good candidates for these types of surgery.
Intentional Replantation
As defined by Dr. Grossman, replantation is “the purposeful removal of a tooth and its almost immediate replacement with the object of obturating the canals apically while the tooth is out of its socket” (Kim 2001). Intentional replantation is an artificial setting mimicking complete tooth avulsion, and its management as defined by the guidelines of the American Association of Endodontists. However, the circumstancing factors are near ideal. The level of tooth contamination and physical damage is likely to be far less than in the case of an accidental injury. Moreover, the single most important factor in the demise of an avulsed tooth, the extraoral dry time, is not a factor because it is practically nonexistent. During intentional replantation, the tooth is immediately submerged in tissue culture medium, with the tooth out-of-socket times being under 10 minutes.
The procedure dates back to the late 1500s, when Paré re-planted three avulsed teeth (Kupfer 1952). Intentional replantation has been performed for over half a century with success rates being reported between 80% and 95% for follow-ups of 2 to 22 years by Grossman, Kingsbury, and Bender (Kim 2001). Although many of these teeth exhibited some degree of ankylosis and replacement resorption, they were clinically functional and did not exhibit any signs of periradicular pathosis. With the development of new protocols that call for the use of Hanks balanced salt solution (HBSS) (BioWhittaker, Walkersville, MD, USA) as an intermediate storage and operating medium, and the use of enamel matrix derived protein (Emdogain; Straumann, Waldenburg, Switzerland) along with careful extraction techniques to prevent damage to the cementum and the PDL cells, the chances of resorption can be minimized.
Indications and Case Selection
Intentional replantation should not be the treatment of choice if endodontic retreatment or surgery can be performed with a fore/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


