Silver Amalgam and Current Applications
Clinical Properties
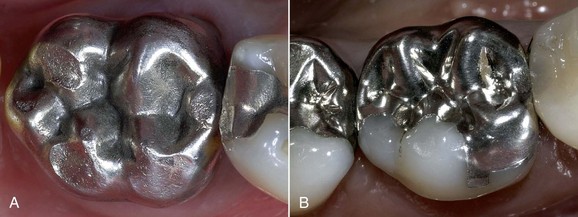
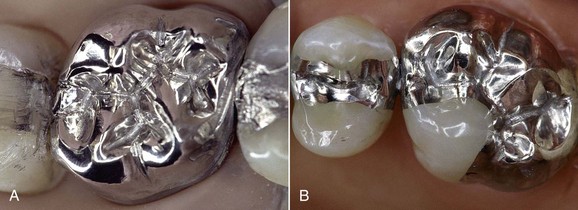
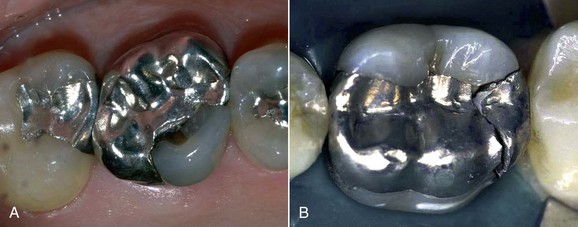
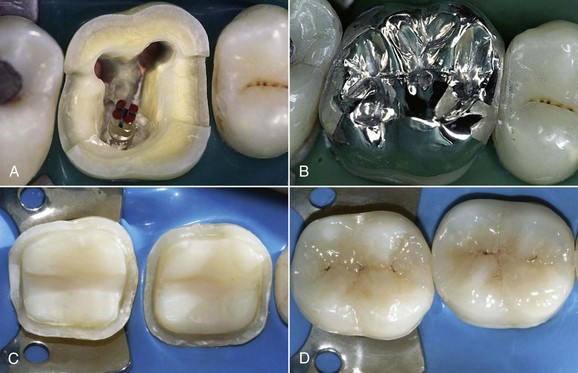
Silver amalgam has a clinically adequate resistance to compression and abrasion. Amalgam restorations exhibit good biomechanical behavior even over time and retain their morphology and margins (Figure 5-1). Marginal self-sealing ability (Figure 5-2) resulting from the production of surface oxides is an important factor.
Excellent polishability is another important feature (Figure 5-3). During polishing it is advisable to use a rubber dam to protect the patient against the absorption of mercury vapors.
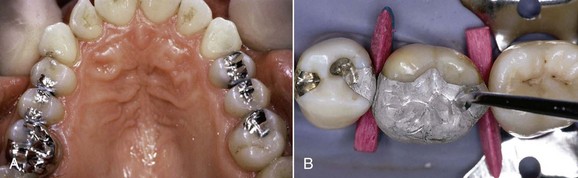
Amalgam can be used for small, midsize, and large restorations, including extensive cuspal coverage restorations, demonstrating its versatility and relative ease of use (Figure 5-4).
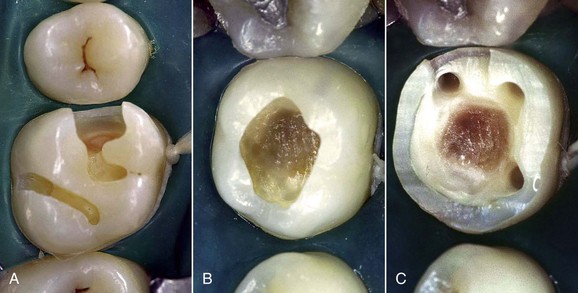
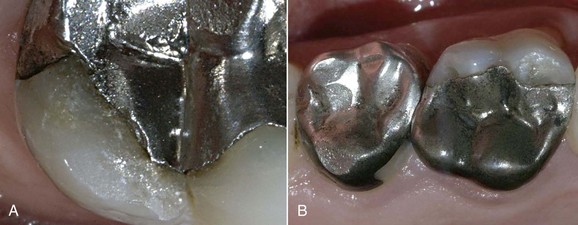
The most important drawback, however, is the lack of adhesion to the residual tooth structure (Figure 5-5, A). This necessitates preparation of retentive cavities, sometimes sacrificing healthy tissue and inevitably weakening the residual dental structure. In fact, cavities for amalgam require a specific configuration and geometry. In order to be retentive and resistant they must have a flattened floor, undercut walls, and adequate depth and width, both occlusally and at the isthmuses. Sometimes complex restorations require the preparation of wells in the sound dentin (amalgapin technique) (Figure 5-5, B and C), possibly sacrificing the pulp in order to exploit the pulp chamber for retentive purposes (Bergman, 1990). Other disadvantages (Bergman, 1990) include low resistance to torsion and fracture, necessitating the placement of amalgam layers that are at least 2 mm thick (Figure 5-6); the possibility of oxidation, mercuroscopic expansion (the reaction of the mercury when combined with the other alloys in amalgam; secondary expansion occurs 1 to 7 days after placement owing to moisture contamination before the complete setting of the amalgam), and corrosion (Figure 5-7); amalgam tattoos of the soft tissues (Figure 5-8); and poor esthetic qualities (Figure 5-9).
Clinical Considerations: Amalgam Versus Adhesive Restorations
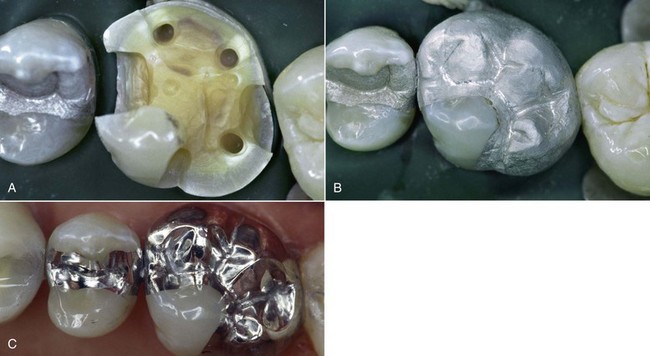
The first important aspect is that cavity design is dictated primarily by the retentive needs of the material rather than the real extent of the caries lesion. Partially undermining midsize lesions (Figure 5-10) often necessitates the removal of tooth walls to avoid cuspal fracture and create retention wells, for the sole aim of attaining additional retention for the restoration (Figure 5-11).
Similar considerations apply to complex extensive cuspal coverage restorations (Figures 5-11 and 5-12) that require at least one amalgapin for each missing cusp (Shavell, 1986), with inherent risks of pulpal involvement. If we compare amalgam with adhesive techniques, we find that the latter are better attuned to the “tissue-saving” principle, which is the basis of modern minimally invasive restorative dentistry—that is, a lesion that once required a Class I amalgam filling can now be treated with simple and minimal preventive adhesive restoration (Figure 5-13). Similarly, Class I restorations (Figure 5-14) no longer call for designing, shaping, and flattening of the cavity floor, as cleansing and margin regularization are sufficient today. Amalgam Class II slots in upper premolars (Figure 5-15) had clear limitations because of retention issues and the angle between the amalgam and cavity walls (amalgam margin angle [AMA], cavosurface angle [CSA]), which was often too sharp owing to very inclined cusp slopes. This meant the risk of complete detachment of the material or occlusal margin fractures, problems that can now be managed completely with adhesive techniques.
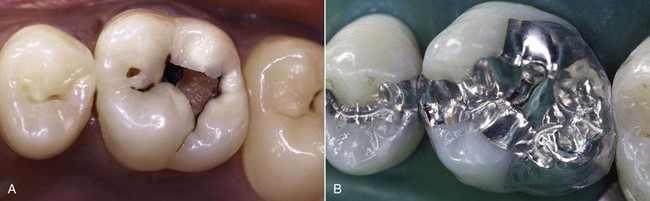
Figure 5-12 Deep caries of tooth 14 in young patient (A). Complex amalgam restoration with full cuspal coverage (B).
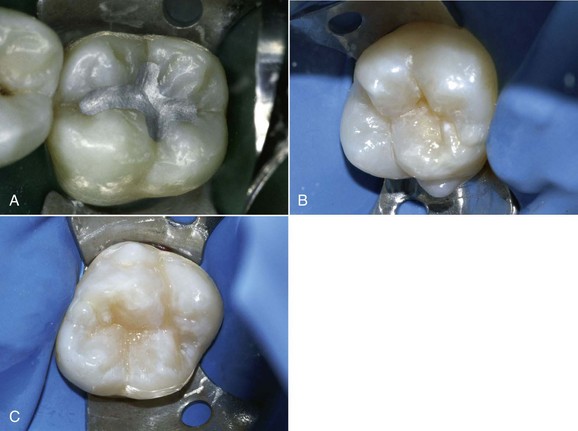
Figure 5-13 Preventive restorations.

Figure 5-14 Class I restorations.
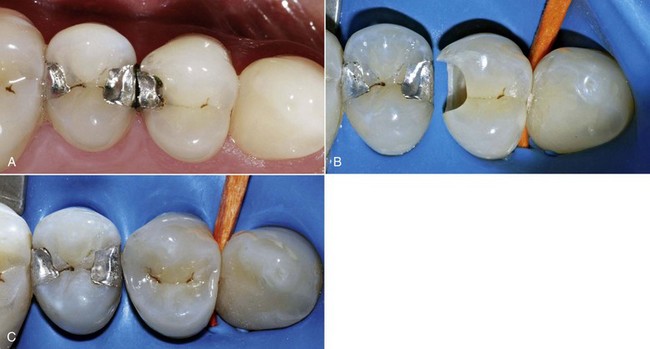
Figure 5-15 Class II slot restorations.
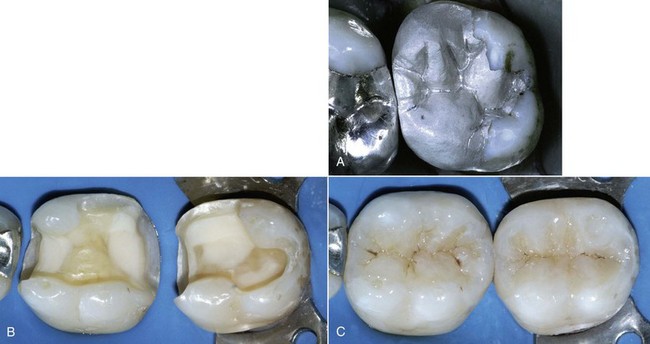
Midsize Class II amalgam restorations require a geometric design with a flattened floor, diverging walls, and dovetail retentions (Figure 5-16, A), whereas the shape of adhesive cavities (Figure 5-16, B) is dictated by the carious lesion topography, with selective removal of caries and subsequent finishing of the margins; the box is rounded and the restoration is much more conservative, with good esthetic results (Figure 5-16, C).
Adhesive techniques also permit complex onlay restorations with partial cuspal coverage (Figure 5- 17) up to the overlay with full cuspal coverage (Figure 5-18), yielding good esthetic results compared with traditional techniques, but especially a more conservative approach that—as in the case shown in the figures—makes it possible to preserve both sound dentin and pulp vitality, even in severely compromised teeth in which the use of amalgam would entail root-canal treatment for mere retentive purposes. Moreover, silver amalgam restorations of endodontically treated teeth (Figure 5-18, A) require a much more aggressive approach with the use of titanium posts, which have a lower modulus of elasticity compared with the fiber posts associated with the adhesive technique. The life of overlays is excellent in both cases, but today patients prefer “invisible” restorations. In addition, in the event of possible future prosthetic work, a composite adhesive restoration with fiber posts is more appropriate (also because of the better modulus of elasticity) than a silver amalgam restoration in which mechanical retention is conferred by titanium or steel posts.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses