Chapter 5
Root Caries: Aetiology, Diagnosis and Management
Aim
The aims of this chapter are to provide the practitioner with a review of the aetiology, diagnosis and management methodologies for root caries.
Outcome
The practitioner by the end of this chapter should be in a position to use an understanding of the aetiology and diagnosis of root caries to formulate contemporary treatment strategies for root caries.
Terminology
Dental caries is a disease of the mineralised tissues of teeth caused by the action of microorganisms on fermentable carbohydrates. It is characterised by demineralisation of the mineral portion of the tissues followed by the disintegration of the organic material.
Primary root carious lesions may be defined as lesions resulting from a carious attack initiating on root structure below the cemento-enamel junction (CEJ) with no initial involvement of the adjacent enamel or restorations. It can be arrested and remineralisation can occur.
Secondary root caries may be defined as lesions resulting from a carious attack on root structure adjacent to an existing restoration.
Epidemiology of Root Caries
In the older population, prevalence of root caries can vary between 57% and 88%. The greater prevalence is associated with the prolonged retention of teeth in older age groups and increased exposure of root surfaces, coupled with the ageing of the population. Incidence studies have shown that 30–40% of people studied develop root caries. Proximal surfaces may account for up to 54% of root carious lesions.
Aetiology
Root caries is a dynamic disease process with the potential for remineralisation as well as demineralisation to occur. A summary of the factors influencing the dynamics of root caries development is shown in Fig 5-1.
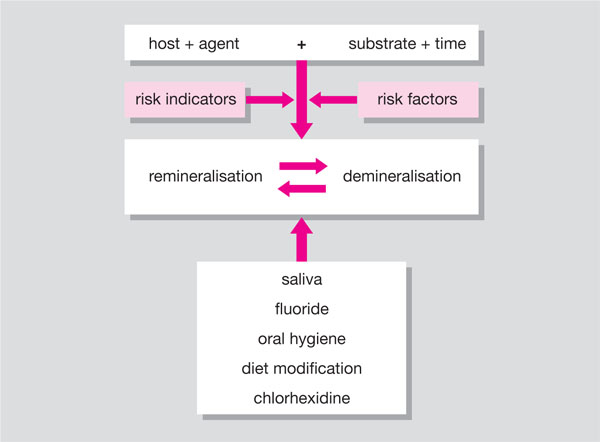
Fig 5-1 Factors involved in the demineralisation/remineralisation of root caries lesions.
Host
Cementum comprises 50% organic and 50% inorganic material. Periodontal fibres called Sharpey’s Fibres traverse it. Cementum exists in a cellular and an acellular form, with the cellular form covering the apical third of the root and the acellular cementum forming a thin layer adjacent to the dentine surface. Cementum is 150–200 mm wide apically but only 20–50 mm wide at the CEJ. In 10% of cases cementum does not reach as far coronally as the CEJ, exposing the underlying dentine. With ageing, there is increased exposure of root surfaces, and when exposure of the root surface occurs cementum is lost, especially on the facial surfaces, and dentine is exposed.
Microorganisms
Various types of microorganisms have been associated with primary root caries, including mutans streptococci, non-mutans streptococci, gram-positive pleomorphic rods (GPPR), including Actinomyces spp. and lactobacilli.
Substrate
Development of root caries has been associated with those patients who give a diet history of more exposures to fermentable carbohydrate per week.
Time
For caries on the root surface to occur, the microorganisms metabolise the carbohydrates and acid is produced which can lead to demineralisation of the dental tissues. The disease process is dynamic, and remineralisation can occur as the pH rises above the critical value for cementum and dentine -pH 6.5. The longer the period that demineralisation is taking place the more likely it is that caries will develop. Consequently, factors that prolong the carious attack, such as xerostomia, repeated carbohydrate intake or partial-denture wearing, will increase the probability of dental decay developing.
Risk Factors and Risk Indicators
Based on epidemiological studies, a variety of risk factors and risk indicators have been determined. The risk factors and risk indicators can help identify individuals who are at increased risk of developing root caries. These are summarised in Table 5-1.
| Risk Indicators | Risk Factors | |
| Sociodemographic | age | age |
| education | ||
| race | race | |
| institutionalisation | institutionalisation | |
| gender | gender | |
| decreased cognition | ||
| Physical/medical | chronic diseases | anxiety level |
| disability/recent illness | ||
| Intra-oral | Mutans streptococci | |
| Lactobacilli | Lactobacilli | |
| Candida albicans | ||
| saliva flow rate | ||
| Environmental | systemic fluoride | systemic fluoride |
| Behavioural | regular check-ups | social integration |
| emergency dental visit | tobacco | |
| tobacco use | ||
| carbohydrate intake | carbohydrate intake | |
| infrequent tooth-brushing | ||
| Oral health status | poor oral hygiene | poor oral hygiene |
| gingivitis | gingivitis | |
| loss of attachment | loss of attachment | |
| calculus | ||
| gingival recession | gingival recession | |
| periodontal pockets | periodontal pockets | |
| > 3 mm | > 3 mm | |
| coronal caries experience | coronal caries experience | |
| root caries experience | root caries experience | |
| few remaining teeth | few remaining teeth | |
| partial denture |
Diagnosis
Increased levels of microorganisms are associated with specific clinical characteristics of primary root caries lesions, namely:
-
Proximity to the gingival margin. The closer a lesion is to the gingival margin the more likely it is to be active.
-
Texture. Lesion texture (specifically lesion hardness as opposed to surface roughness) as a diagnostic criterion for root carious activity was validated when lesions which were categorised as soft on probing were shown to harbour the greatest number of bacteria associated with primary root caries activity.
-
Cavitation. With increasing cavity depth lesion activity increases.
-
Size. Larger lesions are more likely to be active than smaller lesions.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


