5 Removal of unerupted teeth
ASSUMED KNOWLEDGE
It is assumed that at this stage you will have knowledge/competencies in the following areas:
INTENDED LEARNING OUTCOMES
At the end of this chapter you should be able to:
INTRODUCTION
Teeth fail to erupt into functional positions for a variety of reasons:
PREOPERATIVE ASSESSMENT OF THE IMPACTED LOWER THIRD MOLAR
History
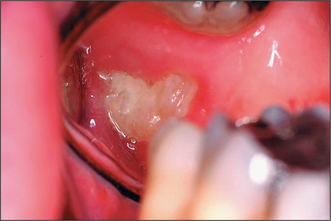
Most patients attending hospital with impacted teeth are referred because of pain and infection, associated with partially erupted teeth (Fig. 5.2); however, many impacted or displaced teeth are unerupted and asymptomatic and therefore an incidental finding following radiographic examination. Occasionally, unerupted wisdom teeth, in the absence of any obvious infection, can give rise to discomfort (often described by patients as ‘pressure’ at the back of the mouth). It is important to exclude other possible causes such as temporomandibular joint pain and pulpitis/periapical abscess from another tooth.
Pericoronitis
Signs and symptoms of pericoronitis include swelling, soreness, erythema of the overlying soft-tissue operculum, trismus, facial swelling, raised temperature, regional lymphadenopathy and general malaise. The disorder may be precipitated by trauma from an over-erupted upper wisdom tooth or entrapment of food debris and bacterial infection of the operculum.
Pericoronitis may be treated by removal of the upper wisdom tooth (if this is traumatizing the operculum overlying the lower wisdom tooth), irrigation under the operculum with chlorhexidine, the careful application of a medicament such as trichloroacetic acid beneath the operculum, hot salt-water mouthwashes and analgesics (e.g. ibuprofen). If there is systemic involvement, then antibiotics are indicated (e.g. amoxicillin or metronidazole). Severe infections may require admission to hospital as they can spread through the fascial planes and compromise the airway (see Ch. 7).
Clinical examination assesses the wisdom tooth and excludes other causes of symptoms:
Radiological assessment
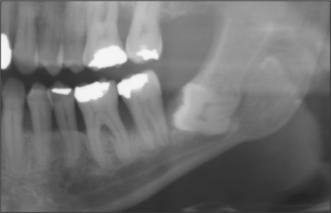
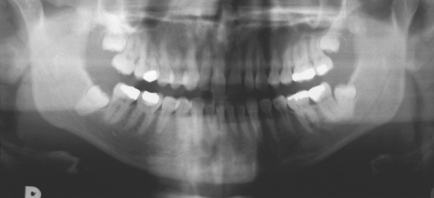
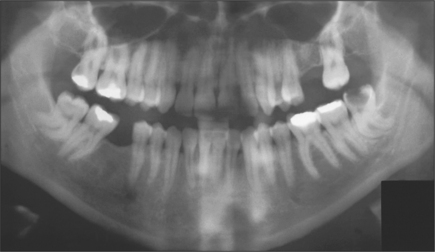
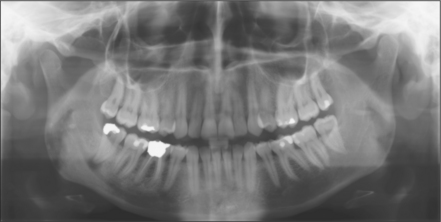
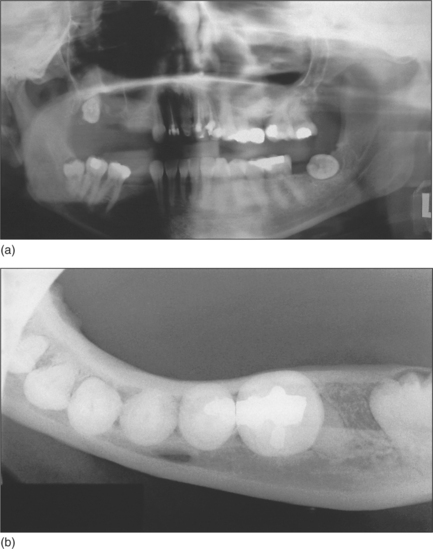
The radiographic examination of choice is a panoramic radiograph such as an OPT (Fig. 5.3), although periapical or oblique lateral views of the mandible may be taken as an alternative. When referring a case for treatment all recent relevant radiographs should be included to avoid further exposure to ionizing radiation.
The following radiological assessment of the lower third molar should be made:
Diagnosis
Patient preference should be taken into account when deciding on the form of anaesthesia: local anaesthesia, intravenous sedation, general anaesthesia.
Reasons for removal
The US National Institutes for Health (NIH) consensus on indications for removing wisdom teeth (published in 1980) (see also SIGN 2000 and NICE 2000) listed the following points as definite indications for removal:
Contraindications to removal
There is no strong indication to extract asymptomatic contralateral or unerupted maxillary teeth simultaneously if they are disease-free.
Informed consent for the removal of wisdom teeth
Factors influencing the decision to refer to a specialist include:
Type of impaction
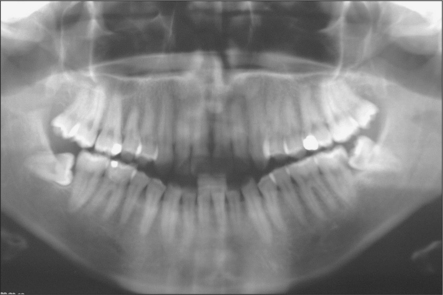
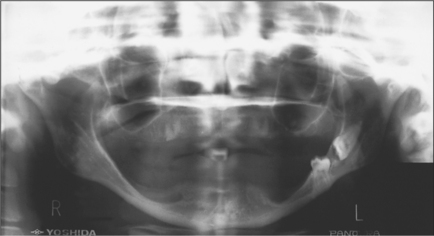
Lower third molars may be impacted mesioangularly (Fig. 5.3, right), vertically (Fig. 5.6), distoangularly (Fig. 5.3, left), horizontally (Fig. 5.10) or ectopically placed.
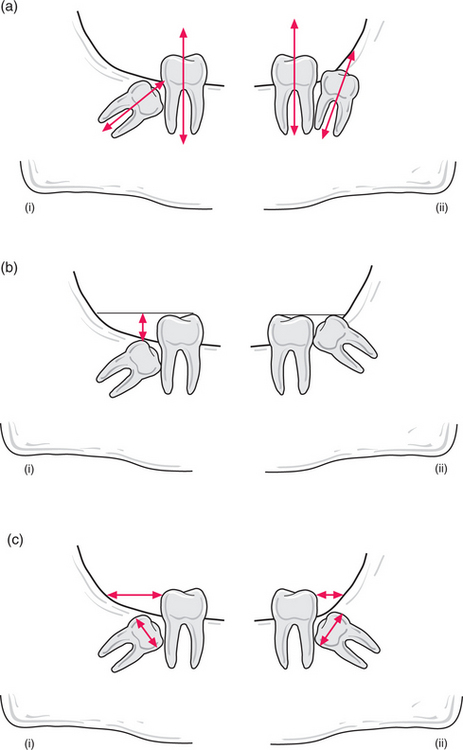
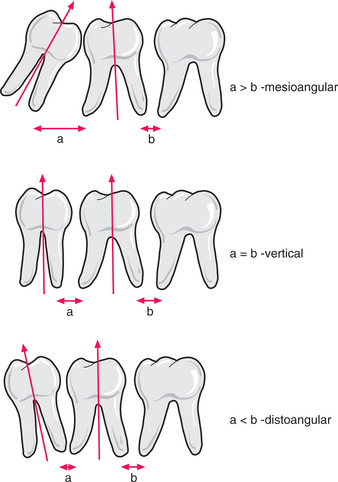
One simple method of determining the type of impaction involves comparing the distance between the roots of the third and second molar (a) with the distance between the roots of the second and first molars (b) (Fig. 5.11). If (a) is greater than (b) it is a mesioangular impaction; where (a) is less than (b) it is a distoangular impaction; where (a) is equal to (b) it is a vertical impaction. If the first molar is missing, the impaction can be determined by comparing a line drawn down the long axis of both the second and third molars: if parallel, it is vertical; if lower 8 leans towards lower 7 it is mesioangular; if the lower 8 long axis diverges from that of the 7, then it is a distoangular impaction.
A horizontal tooth (i.e. where the line down the long axis of the tooth is roughly parallel with the occlusal plane) usually has its crown facing the second molar but occasionally lies buccolingually (Fig. 5.12). An occlusal view can be taken to identify which way the crown lies. Pell and Gregory (1933) have classified the position of the impacted lower wisdom tooth according to (1) distance between distal surface of lower second molar and anterior aspect of ramus and (2) depth of the occlusal surface of the wisdom tooth in comparison to the occlusal plane of the second molar.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses