Chapter 5
Pulp Protection Regimes. Sealers, Liners and Bases
Aim
Pulp protection regimes have changed dramatically over recent years. The aim of this chapter is to update the practitioner about contemporary pulp protection regimes.
Outcome
At the end of this section practitioners will be familiar with modern pulp protection regimes and recognise the clinical indications for sealers, liners and bases.
Introduction
Bacterial contamination of dentinal tubules and subsequently the pulp is the principal cause of pulpal inflammation. The direct toxic effects on the pulp of restorative materials have been shown to be mild and transitory. The pulp may have been inflamed prior to a restoration being placed but this inflammation will largely resolve following treatment (reversible pulpitis) provided further bacterial contamination is prevented. The pulp may also be damaged due to sudden and excessive rises in temperature generated during the restorative procedure through inadequate water-cooling of burs, use of worn burs and/or inadequately maintained handpieces and excessive dehydration of the pulp during operative procedures. It is important, therefore, to maintain handpieces with regular servicing and to replace burs which have become worn. Single-use burs offer obvious advantages in this respect.
Accidental entry into the pulp chamber (pulpal exposure) by a hand or rotary instrument (traumatic exposure) will damage the pulp. Accurate knowledge of the anatomy of each tooth is therefore essential to ensure that tooth preparation is completed with the minimum of iatrogenic damage. An important consideration is the age of the patient, as younger patients have larger pulp chambers than older patients. Previous restorative treatment and other insults to the pulp will have resulted in a reduction in the size of the pulp chamber due to secondary dentine being laid down.
To prevent noxious stimuli reaching the pulp it has been custom and practice to apply protective materials to the floor and/or the pulpo-axial wall of preparations. These materials were commonly placed under amalgams and resin composites to prevent thermal stimulation of the pulp and acid contamination of dentine respectively. It has been demonstrated that thermal stimulation of dentine is not normally a problem clinically and that routine basing of preparations for amalgams, to prevent thermal stimulation, inherently weakens the restoration without benefit to the continuing vitality of the tooth. It is also accepted that dentine can be etched without deleterious pulpal effects and therefore routine lining of preparations for resin composites is now contraindicated.
It is currently suggested that the routine placement of a preparation liner or base is contraindicated. All preparations should, however, have some form of sealer applied and some preparations (usually deep) will require a liner and/or base (Fig 5-1). There is some merit in etching preparations prior to placing a sealer, liner or base, as etching will remove the smear layer, which is contaminated with bacteria. Removal of the smear layer in this way affords gross debridement of the preparation and will also improve the quality of the interface between the sealer/liner and the dentine substrate.
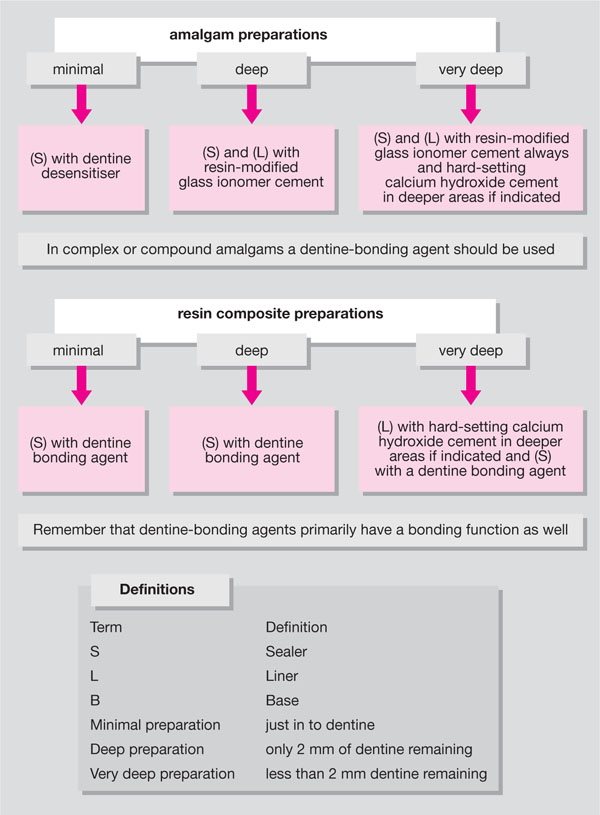
Fig 5-1 Algorithm for pulp-protection regimes.
Sealers
A preparation sealer is a material which seals the dentinal tubules and provides a protective coating for freshly cut dentine. Examples of sealers include copal ether cavity varnish and dentine desensitisers.
Liners
Preparation liners also seal freshly cut dentine but have additional functions such as adhesion to tooth structure, fluoride release, and/or antibacterial action. Preparation liners are applied in thin section (>0.5 mm), and materials currently used include resin-modified glass ionomer cements, dentine-bonding agents, flowable resin composites and hard-setting calcium hydroxide cements. It has been suggested that resin-modified glass ionomer cements have greater resistance to microleakage than dentine-bonding agents. This feature can be used to good advantage when planning to place an amalgam in a deep preparation.
It has been recommended that the resin-modified glass ionomer cement liner should be applied to the preparation and not cured with the amalgam packed directly onto the liner. The rationale behind this approach is that the liner will chemically cure whilst developing adhesion both to the tooth and the amalgam restoration, further enhancing restoration retention. Some clinicians advocate that two layers of resin-/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


