Chapter 5
Periapical and Bone Inflammation
Aim
The aim of this chapter is to provide the practitioner with an understanding of the radiology of common inflammatory conditions affecting the periapical regions and bone.
Introduction
Inflammation is the most frequent cause of altered radiological appearances in the periapical region. Demineralisation of between 30% and 60% of hard tissue is necessary before radiological signs of pathosis become apparent. This process can take up to ten days, hence the delay between the onset of clinical signs and symptoms and their radiographic appearance.
Choice of Radiographs
The traditional method of assessing the status of the periapical region of a tooth is by intraoral periapical radiography. The paralleling technique is preferable to the bisecting angle technique as the latter can result in geometric inaccuracies that may distort or obscure apical pathology (Fig 5-1).
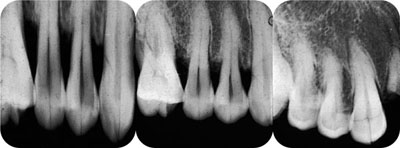
Fig 5-1 The effect of beam angulation in bisecting angle radiography on root length. The film in the centre was taken with the correct beam angulation, that on the left with too shallow an angle and that on the right with too steep an angle. The steep angle has also masked the periodontal bone loss.
The ideal periapical radiograph should display optimal image geometry and at least 3 mm of periapical bone to allow an adequate assessment of the apical status. Panoramic radiography is also used to assess periapical pathology although, as outlined in Chapter 4, the technique has severe limitations especially in the incisor, canine and premolar regions of the oral cavity.
Sensitivity values for periapical radiography in detecting apical change are high ranging from 65% to 84%. By comparison, panoramic radiography produces lower overall sensitivity levels falling to 29% for the mandibular incisor/canine region.
An effective way to identify the majority (90%) of apical lesions is by the use of referral criteria in combination with patients’ clinical signs and symptoms and certain radiographic features (i.e. gross caries, previous endodontic therapy and heavily restored teeth) seen on bitewing radiographs. Panoramic or lateral oblique radiography may be useful in those patients with extensive inflammatory pathology.
Classification of Inflammatory Lesions
Inflammatory pathology will be discussed using the following headings.
periapical inflammatory disease
-
chronic periapical periodontitis
-
acute periapical periodontitis
-
lesions associated with periapical periodontitis
pericoronitis
osteomyelitis
-
acute osteomyelitis
-
chronic osteomyelitis
-
chronic suppurative (or rarefying) osteomyelitis
-
sclerosing osteomyelitis
-
Garrè’s osteomyelitis
-
osteoradionecrosis.
Periapical Inflammatory Disease
Pulpal necrosis represents the most common cause of changes to the periapical tissues. Periapical inflammation of pulp origin results in a variety of radiological signs that are summarised in Table 5-1.
| Acute apical periodontitis | Chronic apical periodontitis | |
| Loss of lamina dura | ✓ | |
| Widening of periapical periodontal ligament |
✓ | ✓ |
| Rarefying osteitis | ✓ | |
| Sclerosing osteitis | ✓ | |
| Well-defined rounded radiolucency |
✓ |
Chronic Periapical Periodontitis
Chronic periapical periodontitis represents a condition in which the inflammatory response is controlled by mechanisms within the host and is generally asymptomatic for the patient. The response of bone to low-grade and long-standing infection is specific and the radiological features are characteristic.
The following radiological signs are associated with the presence of low-grade chronic inflammation within the periapical tissues:
widening of the periodontal ligament space
widening of the periodontal ligament space and sclerosing (or condensing) osteitis
well-defined apical radiolucency.
Clinical features
The patient is usually asymptomatic or exhibits mild discomfort.
Radiological signs
The initial radiographic feature is a widening of the periodontal ligament space due to the accumulation of inflammatory exudate in the periapical tissue (Fig 5-2). The slow inflammatory process causes the remodelling of the lamina dura further from the tooth apex.

Fig 5-2 Widening of the periapical periodontal ligament on 22.
In the posterior maxilla, widening of the periodontal ligament space may elevate the antral floor. Periapical inflammatory toxins stimulate extra bone production and hypertrophy in the overlying antral mucosa (Fig 5-3). This appearance has been referred to as an “antral halo”.
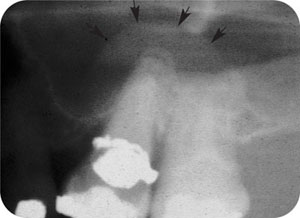
Fig 5-3 The first molar tooth has a widened periodontal ligament and an intact lamina dura. Above this the mucosa of the antral floor (arrowed) has thickened in response to the periapical inflammation, forming an “antral halo”.
It is important to recognise that chronic periapical periodontitis can result in bone formation, in the form of a sclerosing (or condensing) osteitis (Fig 5-4). This appearance will often remain evident for many years subsequent to tooth extraction or successful endodontic therapy.
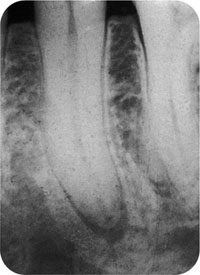
Fig 5-4 Periapical sclerosing (condensing) osteitis around a lower premolar.
The development of a well-defined round apical radiolucency marks the development of a periapical granuloma (Fig 5-5) or a radicular cyst (see Chapter 9). Radiological differentiation between granuloma and cyst is related to the size of the lesion, but there is no clear cut-off point. A threshold of 10 mm is often given as a “rule of thumb” threshold. However, one-third of smaller radiolucencies will be cystic, while one-third of those with a diameter exceeding 15 mm will be granulomas. It is rare for a granuloma to exceed 20mm in diameter.

Fig 5-5 Periapical granuloma on 11. The radiolcency is well-defined and the lamina dura is absent from around the tooth apex.
Acute Periapical Periodontitis
Acute periapical periodontitis may occur de novo or result as an acute exacerbation of an established chronic periapical periodontitis. Conversely, of course, an acute lesion can evolve into a chronic state. It is important to remember that no radiological features may be evident during the initial stages of the acute inflammatory episode, although the patient may be symptomatic.
The following radiological features are associated with the presence of acute inflammation within the periapical tissue and periapical bone:
-
Loss of the lamina dura with/withou/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


