Chapter 5
Hand hygiene
HANDS AS A SOURCE OF INFECTION
Microbial colonisation of the hands
The entire surface of the human body is colonised by microorganisms. High bacterial counts in the region of million colony forming bacteria per millilitre are found on the skin below the waist particularly in the warm moist perineal and inguinal areas. Lower numbers of bacteria colonise the skin of the hands, trunk and underarms. Skin colonisation increases dramatically in chronic skin conditions, e.g. dermatitis or acne. Most people shed about a million skin scales (squames) per day. Attached to the shed skin scales are microorganisms, mainly desiccation-resistant species such as staphylococci and enterococci. The shed bacteria are deposited on clothes, uniforms, masks and in the surrounding local environment.
Resident and transient bacteria
Skin of the hands harbours two main types of microorganisms, resident and transient, that colonise and survive on the hands for differing amounts of time. Resident microorganisms, as their name suggests, make up the persistent microbial flora of the hands living on the surface and within the superficial structures of the skin without causing infection. For most of the time, the bacterial relationship with the host is symbiotic. However, if the intact skin is breached by surgical interventions such as suturing then resident species (e.g. Staphylococcus epidermidis) can become opportunistic pathogens causing wound or deep-seated infections, whereas transient microorganisms that include environmental and pathogenic bacteria, fungi or viruses colonise the skin for short periods of time, usually only hours or days.
Following even brief episodes of personal contact, shaking hands or touching a patient’s face, 100–1000 bacteria are transferred onto the dental health care personnel’s hands. Not surprisingly, even higher rates of bacterial transfer can occur during patient treatment, as hands become progressively colonised with organisms from the respiratory tract and mouth. After the initial contamination of the skin, the rapidly dividing bacteria are transferred to previously uncontaminated parts of the hands, wrists or cuffs as the latter brush over the hands. Bacterial replication will continue in a linear fashion until the hands are cleaned. It is then easy to inadvertently transfer the patient’s pathogenic microbes growing on the hands and inoculate your own mouth and eyes. Direct contact via hands is the major route of spread for a number of organisms including MRSA, influenza viruses and herpes viruses that cause cold sores and shingles (see Chapter 2).
HANDS AS A SOURCE OF HOSPITAL-ACQUIRED INFECTION
Hands of health care workers and patients are instrumental in the spread of multi-drug-resistant bacteria such as MRSA and Clostridium difficile. About 5–10% of patients during their hospital stay will pick up a healthcare associated infection (HCAI). Some of them may have fatal consequences, but all infections will add to the cost of patient treatment and cause unnecessary suffering and inconvenience to the patient and their family and friends. In the USA, 2 000 000 patients become seriously ill as a result of acquiring an infection in hospital with approximately 80 000 deaths annually. In England, healthcare associated infection costs in the region of £3–8000 per infection. Yet, this unwelcome chain of events can be broken simply and expediently by effective use of hand hygiene. Results from the data collected over the last 30 years provide strong evidence that hand hygiene is the single most important method of reducing cross-transmission of infectious organisms (Pratta et al., 2007).
HAND HYGIENE AND TEAMWORKING
The foundation for the World Health Organization (WHO) campaign to promote hand hygiene was the compelling results from the longitudinal study by Pittet et al. (2000) working in hospitals in Geneva, Switzerland. They introduced alcohol/chlorhexidine gluconate 0.5% hand rub solution as the focal point of a hospital-wide hand hygiene campaign. With the cooperation of the hospital staff their campaign achieved an impressive 44% reduction in HCAI and a 50% fall in patient colonisation with MRSA. An important lesson was learnt from their work of direct relevance to dental practice. Long-term success (the study was conducted over 6 years) was dependent on the active involvement of senior personnel who were publically seen to endorse the campaign. Posters and other promotional material reinforced the main message of the campaign and staff received regular feedback from local audits evaluating their compliance with hand hygiene measures. Similarly, dentists as team leaders can influence the behaviour of other members of their team by acting as positive role models. Staff are more likely to follow suit and embrace protocols, if dentists or, in the case of dental schools, professors are witnessed to actively comply with infection control measures.
Choosing the correct hand hygiene product
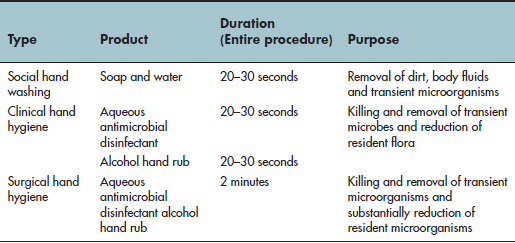
The new term ‘hand hygiene’ encompasses traditional hand washing with soap and water or aqueous antimicrobial detergents and the newer technique of hand rubbing with alcohol-based products (gels, rinses and foams) that do not require running water.
Not all skin-cleaning agents are equally effective at removing organic material or killing microbes (see Table 5.1). So, choosing the most appropriate agent for hand hygiene will depend on when and why the hands are being cleaned. Hand hygiene is used in three circumstances: social, antiseptic and surgical (see Table 5.2). It is impossible to completely sterilise the hands as resident bacteria survive in the deep skin hair follicles and sebaceous glands, but if hands are cleaned effectively only very low numbers of bacteria will remain (see Figure 5.1).
Table 5.1 Comparison of the properties of common hand hygiene products
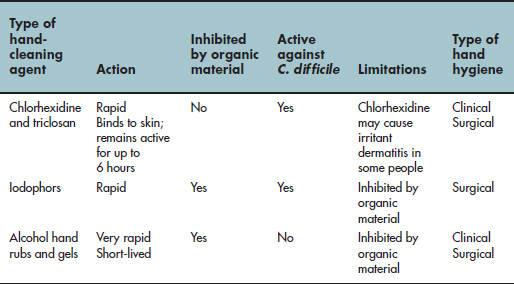
Table 5.2 The three types of hand washing
Alcohol hand rubs
Alcohol hand rubs were originally promoted by health care campaigners to encourage improved compliance and overcome perceived and real barriers to hand washing. In surveys, conventional detergents and soaps were shunned by health care personnel as being damaging to the skin. Inconveniently located sinks and time constraints were also cited as reasons not to wash hands.
Alcohol hand rubs have the advantage of containing an emollient to protect the skin, are inexpensive and hand hygiene can be performed at the chair side. Hand rubs are available in an individual dispenser that can be carried in the pocket or on a belt and are ideal where there is limited access to a sink such as on a domiciliary visit. Commercial products are diluted from 10 to 40% by weight with water to enhance denaturation of microbial proteins. Alcohols demonstrate rapid action against a wide range of Gram-positive and Gram-negative species including MRSA and vancomycin-resistant enterococcus. As little as 15 seconds of vigorous hand rub/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


