Chapter 5
Endodontics in primary teeth
Introduction
The normal pulp
The histological appearance of the normal pulp in a primary tooth is no different from that of the permanent tooth. Physiological aging occurs in both, although the time span during which this occurs is shorter in primary teeth. A common misunderstanding is that the primary tooth is not as sensible to pain as the permanent tooth and that operative treatment therefore would not require local anesthesia to the same extent. Even though it has been observed that the quantity of nerve fibers is smaller in the pulp of primary teeth (62), there is no proof that the primary tooth would not be equally sensible to pain. The only exception would be just before exfoliation, when the number of nerves within the pulp decreases.
Pulpal inflammation in the primary tooth
Even though there has been some controversy in the literature as to the capacity of the pulp of primary teeth to respond to caries by forming reparative dentin, several histological studies have demonstrated a frequent occurrence of reparative dentin in primary molars with deep caries (33, 60, 63, 72). Magnusson and Sundell (42) found a significantly lower frequency of pulp exposure with a stepwise excavation procedure compared with direct complete excavation of deep caries in primary molars, suggesting that the pulp has good potential to produce reparative dentin.
The morphology of the primary molar implies that the clinical symptoms of pulp tissue reactions to damage may differ from those of permanent teeth (Core concept 5.1). Thus, owing to the relatively small distance from the coronal pulp floor to the bifurcation and the frequent presence of accessory canals through the pulpal floor, pulpal inflammation by caries in primary molars more often results in pathological changes in the interradicular area. Fistula and abscesses due to pulp infection also are seen more often in primary teeth, probably because of the relatively thin buccal cortical bone in young children.
Internal root resorption is the most common sequel to inflammation after pulpotomy, the origin of which is not understood. It may be due to the different way in which the pulp tissue in primary teeth reacts to irritating agents. Thus, it has been shown that the physiological process of shedding occurs in areas lacking predentin, which has been shown to increase the risk of internal resorption (50, 78). By using calcium hydroxide as a dressing material after pulpotomy, the presence of a remaining blood clot between the dressing and the wound surface has been suggested to enhance the internal root resorption process (73).
Diagnosis
Pulpotomy, that is removal of the coronal portion of the pulp tissue, has been and probably still is the most commonly used treatment for primary teeth with carious exposure. As a consequence, focus has been on the ability to assess the extent of preoperative pulpal inflammation. Two diagnostic terms are often used in the literature: partial pulpitis, designated for teeth without preoperative clinical and/or radiographic symptoms of pulpal inflammation; and total pulpitis, designated for teeth with pre-operative symptoms of pulpal inflammation extending into the root pulp (10, 11, 72).
Although essential for the outcome of the treatment, there is at present no means of clinically determining the precise histological status of the pulp. Teeth judged to be without signs of total pulpitis might have profound pulpal inflammation. The proportion of correctly diagnosed pulps in histological terms judged from preopera-tive clinical findings has been investigated, with results varying from 56 to 81%. Most investigators have reported a poor correlation between clinical and histological findings (11, 12, 37, 60, 63), whereas others have found a relatively high agreement of about 80% (38, 72). Several of these studies suffer from a relatively small number of teeth and it is often not stated how the teeth were selected. Overall, it seems that the probability of arriving at a histologically correct pulp diagnosis based on clinical symptoms is rather poor.
- The molar has practically no root socle.
- The coronal pulp chamber is comparatively large and wide and the distance to the surface of the tooth is small, in both the occlusal and approximal directions.
- The pulp horns are relatively large, in both the occlusal and approximal directions, making the tooth vulnerable to mechanical and carious exposure.
- The distance from the pulpal floor to the bifurcation is short and the area between the pulp floor and the bifurcation often contains accessory canals. Because of this and a possible less well-mineralized dentin in this area, an interradicular widened periodontal membrane with loss of lamina dura or bone loss is a common radiographic sign of extensive inflammatory changes or necrosis of the pulp tissue.
- The roots are often flared and bent and then converge in the apical part and are in close relation to the permanent tooth. In the coronal part the root canals are reasonably wide and accessible, whereas in the apical part they often show intricate morphology with narrow, ribbon-shaped and curved canals. Instrumentation may therefore be difficult, particularly in upper molars.
In the clinic, it may be sufficient to know whether the pulp is treatable with vital pulp therapy or not, and it has been suggested that if teeth are divided into two treatment categories only, i.e. ‘treatable’ (= partial pulpitis; vital pulp treatment) or ‘not treatable’ (= total pulpitis or necrosis; extraction), the agreement between clinical and histological findings will improve (11, 38). However, these studies also suffer from a small number of selected patients and in one (11) the difference between the two groups was not statistically significant. In the other (38), the basis for grouping the teeth focused on the character of the bleeding of the exposed pulp combined with the character of pain, a variable that is difficult to make unequivocal and reliable.
Along with the introduction of treatment options such as partial pulpotomy, indirect pulp capping and stepwise excavation as alternatives to pulpotomy, the diagnostic terms reversible and irreversible pulpal inflammation have been suggested. However, these terms are not supported by any more reliable or accurate markers than those for partial and total pulpitis.
It follows that there are no clinical means to determine accurately the extent and severity of pulpal inflammation. There are, however, various clinical symptoms that can be used to enhance the probability of arriving at a proper pulp diagnosis (Core concept 5.2). It has to be realized though, that teeth with deep carious lesions without any of these symptoms and accordingly classified as partial pulpitis may be classified correctly in histo-logical terms in no more than 60–70% and at best in 80% of cases.
Importantly, it is less difficult to predict total pulpitis from clinical symptoms than it is to predict a healthy pulp or a pulp with partial pulpitis (11, 12, 37, 60), and the obvious presence of any of the listed symptoms (apart from pain from percussion and/or pressure, which is often difficult to interpret) indicates total pulpitis. Particular notice should be given to radiographic pathological changes such as widened and diffusely outlined lamina dura and the presence of spontaneous pain, particularly at night, both of which strongly suggest total pulpitis. Severe symptoms, such as swelling, fistula or an abscess, suggest pulp necrosis.
- Radiographic pathological changes, such as widened periodontal membrane with loss of lamina dura, interradicular or periapical resorptive periodontitis (owing to superimposed structures, radiographic changes may be difficult to discover in maxillary molars)
- Abnormal tooth mobility
- Spontaneous or persistent pain, particularly at night Radiographic signs of calcifications in the pulp chamber
- Dark red and/or thick-viscous bleeding of the exposed pulp
- Pulp exposed after removal of demineralized dentin – large pulp exposure
- Profuse bleeding of the exposed pulp
- Pain from percussion and/or pressure (often difficult to interpret, particularly in younger children)
Healing
A proper preoperative pulp diagnosis is decisive for successful endodontic treatment in primary teeth. Presupposing that the cause is removed, the extent to which inflammation can be present in the pulp while the pulp recovers and undergoes repair and healing is not known. In other words, the stage at which the inflammatory process is irreversible is uncertain but essential, because endodontic treatment in primary teeth focuses mainly on vital pulp therapy.
Results from recent clinical studies on direct or step-wise excavation of deep carious lesions in young permanent teeth and partial pulpotomy of cariously exposed pulps in both primary and young permanent teeth suggest that the pulp has good potential to recover once the irritants are removed (35, 39, 47, 74, 93). Thus, for example, a 100% clinical and radiographic success rate was observed after stepwise excavation in young permanent molars with deep carious lesions after observation periods of at least 2 years. Important prerequisites for successful treatment were the absence of clinical and/or radiographic pathological symptoms.
The operative technique must be pointed out as an important factor for successful endodontic treatment. It has been shown that presumably infected dentin fragments unintentionally left behind in the pulp tissue cause widespread inflammatory reactions (36). Therefore, meticulous cleansing of the exposed pulp is crucial, particularly when using capping techniques (35).
Repair and healing after pulpotomy where the amputation site is situated at the orifices of the root canals, depend on whether or not preoperative inflammatory reactions also involve the root pulp, on the operative technique and on the characteristics of the wound dressing used. Furthermore, infection due to bacterial leakage is a prime threat to both repair and healing (5), and the importance of a bacteria-tight seal cannot be overemphasized.
Wound dressings – characteristics, modes of action and reported clinical success rates
The ideal dressing material for either unexposed or exposed vital pulps should be bactericidal and enhance the repair and healing of the pulp. The dressing also should be biocompatible and not interfere with the physiological process of root resorption. The cost of the material should also be reasonable. Unfortunately, the ideal dressing has still to be discovered. Meanwhile, various dressing materials are used. A detailed list of clinical success rates observed for different treatment procedures with different dressing materials is presented in Table 5.1.
The most commonly used wound dressings are: calcium hydroxide, formocresol (FC), glutaraldehyde, corticosteroids (Ledermix®), zinc oxide–eugenol cement and ferric sulfate. Although still not used much in clinical practice, mineral trioxide aggregate (MTA) is also described since promising clinical results have been obtained with this material.
Calcium hydroxide
Calcium hydroxide is used as a dressing material on both unexposed and exposed pulps. It is a strong alkaline compound with a pH of about 12 that causes a superficial necrosis of about 1.5–2 mm in the area underneath its placement on an exposed pulp. After the initial irritation of the underlying tissue, the pulp produces new collagen and thereafter a bone-like hard tissue. Avoidance of an extrapulpal blood clot is essential when using calcium hydroxide as a wound dressing, because its presence may interfere with pulp healing (73). Therefore, it is important to use a gentle technique, including cutting with high-speed equipment and diamond burs followed by irrigation with water or saline in order to achieve hemostasis.
The formation of a hard-tissue barrier, although seldom complete, protects the pulp mechanically and gives partial protection from bacterial infection (Fig. 5.1). It should be noted though that the presence of such a barrier, often considered a criterion of successful treatment, is no guarantee of a healthy residual pulp (57, 71).
Unsuccessful outcomes of pulpotomies using calcium hydroxide as a wound dressing have been attributed to a blood clot left behind between the dressing and wound surface (73). An in vitro laboratory study showed that blood and serum substantially lowered the pH of calcium hydroxide and thereby reduced its bactericidal effect (45). The presence of bacteria combined with a blood clot may therefore be an important cause of failure. Because the blood clot probably serves as a buffer, it also prevents calcium hydroxide from exerting its superficial necrotiz-ing effect on the pulp tissue. Another reason for failure could be an incorrect preoperative pulp diagnosis. Thus, it has been suggested that calcium hydroxide has no other effect besides promoting the formation of a hard-tissue barrier and therefore cannot be used successfully on an inflamed pulp tissue (73). The latter suggestion is, however, not consistent with recent reports on relatively high rates of successful treatments using partial pulpoto-my in cariously exposed pulps (47, 74).
Fig. 5.1 Hard-tissue barrier in a primary molar formed after pulpotomy using calcium hydroxide as a wound dressing (H & E, ×40). a = wound surface; b = hard-tissue barrier; c = normal pulp tissue. (Courtesy of M. Cvek.)
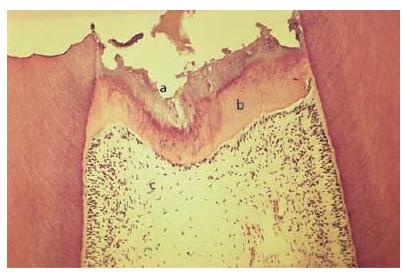
Table 5.1 Reported clinical/radiographic success rates of various vital pulp treatment procedures of primary molars with deep carious lesions along with type of dressing material, number of teeth included in the study and follow-up times.
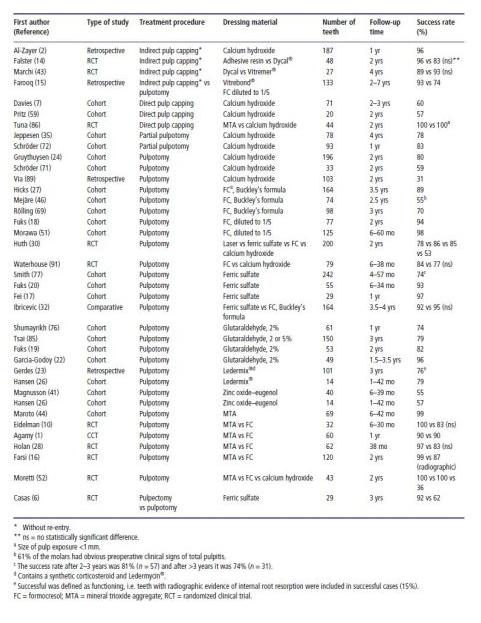
After pulpotomy with calcium hydroxide as a wound dressing, reported success rates vary between 31 and 80% (24, 52, 71, 89). Using the same diagnostic criteria, the overall success rates were higher when calcium hydroxide was used as a dressing material after partial pulpotomy (78–83%) (35, 74) (Table 5.1). As judged from these studies, it seems that the partial pulpotomy technique is more favorable than direct pulp capping. Randomized clinical studies comparing the two techniques have yet to confirm this assumption.
Formocresol
Formocresol (FC) is used as a dressing material after pulpotomy. The original compound, Buckley’s FC, contains concentrated formalin (19% formaldehyde), cresol (35%) and glycerol (7%) in an aqueous solution, the main active component being formaldehyde. Nowadays, Buckley’s formula is often diluted to one-fifth of its original strength. Depending on the concentration and time of exposure to formaldehyde, part of the root pulp tissue is devitalized. Importantly, it has been shown that even after prolonged application of the full concentration of FC the entire pulp was not devitalized (48, 66).
Fig. 5.2 Palatal root of upper second molar. Pulp tissue reactions after pulpotomy with Buckley’s formocresol as dressing, 2.5 years postoperatively: (a) overview (H & E, ×25); (b, c) middle part of the root (H & E, ×60).
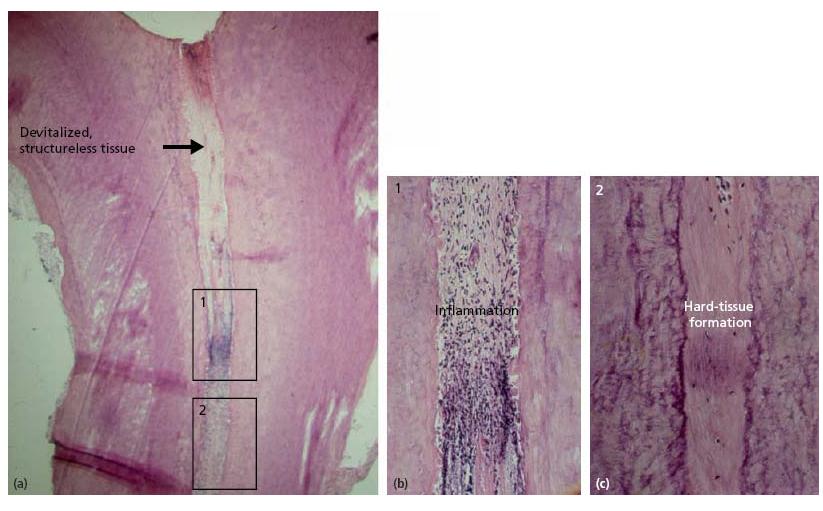
The most common histological appearance when using FC as a wound dressing is devitalized pulp tissue in the upper part of the root canal, inflammatory changes with internal root resorption and apposition of hard tissue in the middle section, with the most apical part usually showing normal pulp tissue (66) (Fig. 5.2). Thus, the use of FC does not result in repair and healing in his-tological terms, and a hard-tissue barrier underneath the dressing is not formed. This makes the tooth vulnerable to contamination from bacterial leakage and emphasizes the importance of a bacteria-tight seal when restoring the tooth.
As shown in Table 5.1, in most studies on pulpotomy the clinical success rates using Buckley’s formula are higher than those obtained with calcium hydroxide as a dressing material (18, 27, 46, 51, 69). Also, when diluted 1:5, the clinical success rates of FC are considerably higher than those of calcium hydroxide (18, 51). Fuks and Bimstein (18), reporting a clinical success rate of 94% after 2 years of observation, recommended the use of the diluted formula of FC instead of Buckley’s FC.
Glutaraldehyde
Glutaraldehyde (GA) – a dialdehyde – has gained increasing attention as a possible substitute for FC as a wound dressing, the suggestion being less pulp devitalization but similar clinical results. Glutaraldehyde has not been produced commercially yet, the main reason being its instability, even when refrigerated.
Like FC, GA can cause allergic skin reactions, and hand dermatitis has been reported in dental assistants after using the disinfecting agent Cidex® (56). There are no unequivocal indications of mutagenic properties of GA. The full concentration or a 1:5 dilution of FC was 2–3 times more cytotoxic to human fibroblasts than 2.5% GA (34). In another study, however, little difference in the relative toxicities was observed between formaldehyde and GA when the data were calculated in terms of molar concentrations rather than dilution (81). Interestingly, GA appeared more toxic to rat nasal epithelium than FC (80). Owing to cross-linking, GA is less penetrative than formaldehyde and consequently causes less immediate damage to pulp tissue. However, in a study on monkeys GA did not result in repair and healing in histological terms (82) and it cannot be ruled out that, under a narrow zone of fixation, partial cell damage and/or a slow death of cells deeper within this zone may lead to chronic cell injury (81).
Studies reporting on the clinical success rate of GA as a wound dressing are listed in Table 5.1. Using 2 or 5% GA, the reported success rates vary from 74 to 96%, the periods of observation being between 1 and 3.5 years (19, 22, 76, 85).
It has been suggested that buffered GA solution is more effective than unbuffered solution. The concentration and time of exposure to the tissue show a strong interaction (81), implying that GA needs a relatively long contact time with the pulp tissue to achieve optimal fixation. Whether this problem can be circumvented in the clinic by raising the concentration is debatable. Thus, the optimal strength of GA is, as yet, uncertain and there are also varying opinions about whether it should be included in the permanent dressing of zinc oxide–eugenol cement or not. Considering the suggested similar cyto-toxicity of GA and FC, it is doubtful whether GA has any advantage over FC as a wound dressing material.
Corticosteroids
The concept behind using corticosteroids as a wound dressing is to suppress and, ideally, reverse any inflammatory reactions in the pulp tissue. Ledermix® – the only commercially available dressing material for this purpose – is a synthetic glucocorticoid with some Ledermycin® (demethylchlortetracycline) added to it, mixed with calcium hydroxide, zinc oxide and eugenol.
There is a great deal of controversy associated with the efficacy of corticosteroids and their capacity, when used locally, to reverse pulpal inflammation. Hansen (25) showed that the active component of Ledermix was decomposed after 18 days. It has been argued also that any anti-inflammatory effect is restricted to the contact area between the dressing and the pulp tissue (3). Furthermore, the dressing does not induce the formation of a hard-tissue barrier, a characteristic considered to be important in protecting the pulp of primary molars from bacterial leakage and subsequent infection. These factors may explain why Ledermix has not gained widespread acceptance as a dressing material.
Hansen et al. (26) compared zinc oxide–eugenol with Ledermix as a wound dressing after pulpotomy in cari-ously exposed pulps and found less severe internal root resorptions and inflammatory reactions in teeth where Ledermix was used. Although a lenient material without any observed side-effects, only a few studies report on the success rate with a corticosteroid as the wound dressing. In a small study of 30 molars and varying observation times, Hansen et al. (26) reported a success rate of 79%. In a 3-year study with 101 molars, Gerdes et al. (23) reported a success rate of 76% (defined as functioning teeth and including 12 teeth with internal root resorptions and four teeth with radiographic and clinical symptoms). From these studies it might be expected that corticosteroids are superior to calcium hydroxide as a dressing material (see Table 5.1). However, because of the lack of randomized prospective clinical studies using different wound dressing materials, it is not possible to propose the best material.
Zinc oxide–eugenol cement
Zinc oxide–eugenol cement is probably not so often used today as a dressing material alone after pulpotomy; it results in a high percentage of internal resorptions and reported clinical success rates are low (55–57%) (26, 41).
Ferric sulfate
Ferric sulfate (Fe2(SO4)3) in a 15.5% solution has been used as a coagulative and hemostatic agent in crown and bridgework. Blood proteins agglutinate when they are exposed to the ferric and sulfate ions but the exact mechanisms of action are still debated.
When used as a wound dressing after pulpotomy, a metal–protein blood clot forms at the site of pulp exposure. Ferric sulfate has been investigated as a possible alternative to FC (17, 19, 77). The reported clinical success rates are similar to those of diluted FC and vary from 78 to 97%. In the retrospective study by Smith et al. (77) the clinical success rate was 74% after 3 years of observation (n = 242); Fei et al. (17) reported a 97% success rate after 3–12 months (n = 29); and Fuks et al. (19) found a success rate of 93% after observation times varying from 6 to 34 months (n = 55). Three systematic reviews comparing formocresol and ferric sulfate medicaments conclude that they are likely to have similar clinical/radiographic results (21, 40, 58).
Mineral trioxide aggregate (MTA)
MTA is a powder composed of tricalcium silicate, bismuth oxide, dicalcium silicate, tricalcium aluminate, tetracalcium aluminoferrite and dicalcium sulfate dihy-drate. It sets via hydration to become a collodial gel with a pH of 12.5, similar to that of calcium hydroxide.The setting time is 3–4 hours, and its compressive strength is comparable to that of IRM® (Intermediate Restorative Material, Dentsply, York, PA, USA) (75, 83, 84). MTA in a set state is biocompatible, has good sealing properties and promotes hard-tissue formation (28).
Overall, high success rates (>95%) have been achieved with MTA as dressing material for treating cariously exposed pulps in primary teeth (1, 10, 16, 28, 44, 52, 86). The studies are summarized in Table 5.1. One study compares MTA with calcium hydroxide for direct pulp capping (86). Both materials gave 100% success rate after 2 years. This is contradictory to the other two studies on direct pulp capping where relatively low success rates were obtained. According to the authors, the main reason for the high success rates is that a tight seal was secured by using resin-bonded zinc oxide–eugenol. Other reasons could be that only small exposures (<1 mm) were accepted, and that only occlusal lesions were included. Furthermore, it cannot be ruled out that some pulp exposures were of traumatic origin.
In five studies evaluating MTA as an alternative to formocresol (FC) in pulpotomized primary molars, the success rate of MTA was equal or superior to FC. As a consequence, the authors suggest that MTA is a proper alternative to FC as a pulp dressing material. Moretti et al. (52) compared MTA with FC or calcium hydroxide as dressing material and found MTA and FC superior to calcium hydroxide.
To summarize, MTA seems to be the dressing material of choice for treating cariously exposed pulps in primary teeth. Longer follow-up periods are, however, needed before any definite conclusions can be made as to the suitability of MTA as dressing material in pulpotomized primary molars. At present, the major drawbacks with MTA seem to be its cost and perceived problem with storage. Commercially available MTA is expensive and once the package is opened, the material should be sealed in an airtight and waterproof container.
Objectives of pulp treatment
Strictly, the objectives of pulp treatment are repair and healing of the residual pulp tissue in histological terms and a well-functioning tooth until normal exfoliation. At present, calcium hydroxide is the only dressing that, theoretically, has the potential to fulfill these criteria.
Because of the relatively low clinical success rate reported for calcium hydroxide after pulpotomy and because of the restricted lifespan of the primary tooth, less strict criteria for the success of pulp treatment />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


