(b) 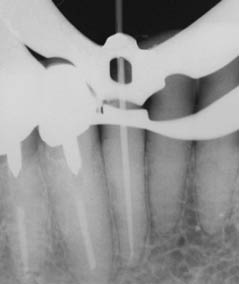 (c)
(c) 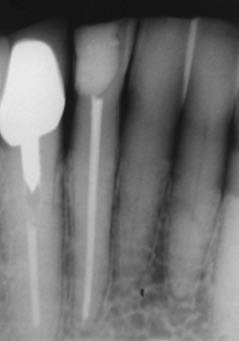
Clinical examination
Extraoral examination revealed the submandibular lymph nodes on the right side to be tender to palpation. Intraoral examination revealed a complete dentition; several of the posterior teeth had been restored with composite restorations and crowns. Periodontal examination revealed a 2–3 mm loss of attachment in the molar regions and around the lower anterior teeth, however, the teeth were plaque-free.
What are the specific routine tests a dentist must perform when examining a tooth for possible endodontic involvement?
- Visual assessment of the adjacent mucosa for signs of erythema, swelling or sinus tracts.
- Inspection of teeth for possible causes of pulpitis and/or periapical periodontitis (for example, caries, marginal adaptation and size of existing restorations, tooth surface loss, cracks and fractures).
- Tenderness to palpation and vertical and horizontal percussion.
- Periodontal probing depths.
- Occlusal assessment.
- Sensibility tests, including electric pulp (EPT) and cold testing.
- Radiographic assessment (periapical radiographs, and when appropriate a cone beam computed tomography scan).
A sinus tract was present on the attached gingivae, lingual to the 42. The 41 and 42, in particular, were tender to percussion, but reacted only mildly to palpation. A fractured composite restoration in the 42 had been temporarily restored one week ago by the patient’s general dentist. All the lower incisors showed marked attrition, resulting in the dentine being exposed at the incisal edges. Periodontal probing depths were less than 3 mm.
A radiograph revealed a periapical radiolucency associated with the root treated 42, which extended to the apex of the 41 and coronally between the two teeth (Figure 5.7.2a).
Figure 5.7.2 (a) A radiograph (3 years later) of the lower anterior area demonstrated a radiolucent lesion around the root apices of the 41 and 42. The lesion extended coronally between the 41 and 42, (b) a size 30 gutta-percha point introduced into the sinus tract on the lingual aspect of the 42, and (c) a diagnostic radiograph with a gutta point tracking one of the sinuses to the apex of the 42.
(Courtesy of Haapasalo et al. Visual Endodontics 2010 multimedia.)
(a)  (b)
(b)  (c)
(c) 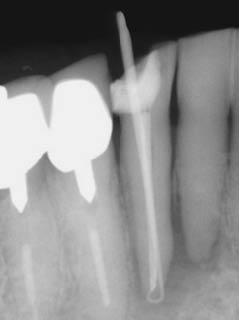
Should more than one radiograph be taken?
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


