43
Orthognathic surgery
Table 43.1 Examples of orthognathic surgical procedures.
| Surgical procedure | Notes |
| Maxillary | |
| Le Fort 1 | Addresses AF and vertical maxillary discrepancies |
| Le Fort 2 | Addresses deficiency of the naso-maxillary complex |
| Le Fort 3 | Addresses deficiency of the naso-maxillary complex and zygoma |
| Wassermund | An anterior maxillary segmental osteotomy for setbacks and setdowns |
| Mandibular | |
| BSSO | For anterior-posterior and asymmetrical mandibular movements |
| Geniop lasty | To move the chin point in three dimensions |
| Total subapical osteotomy | For correction of dento-alveolar retrusion |
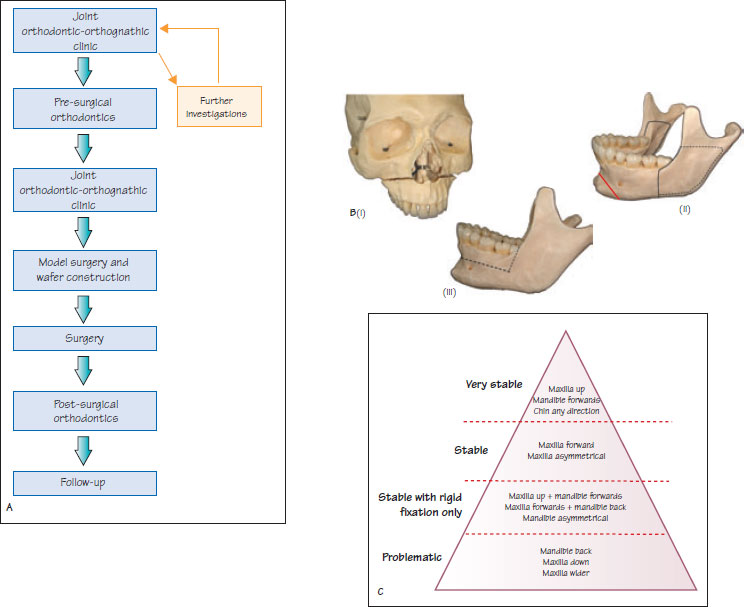
Figure 43.1 (A) Outline of the patient journey through joint orthodontic-orthognathic surgical treatment. (B) Surgical anatomy (i) Le Fort 1 osteotomy, (ii) Genioplasty (red line) and B550 osteotomy, and (iii) total subapical osteotomy. (C) The hierachy of surgical stability. The surgical procedures progressively become less stable as one moves down the list.
Orthodontics in combination with orthognathic surgery is undertaken for the comprehensive management of malocclusion associated with severe skeletal discrepancies in the anteroposterior (AP), vertical and transverse dimensions. This form of treatment is normally undertaken at the end of growth to improve post-treatment stability.
Successful management requires a multidisciplinary team approach involving an orthodontist, oral and maxillofacial surgeon, liaison psychiatrist, general dental practitioner, clinic co-ordinator, technician and sometimes a prosthodontist. Figure 43.1A outlines the patient journey during this form of treatment. The time period between the first multidisciplinary clinic appointment to the end of treatment is usually 2.5–3 years.
Joint orthodontic-orthognathic clinic
Full records, including study models, radiographs and photographs, should be available for the consultation. The purpose of the first joint orthodontic-orthognathic appointment is to introduce the patient to the multidisciplinary team, identify their main concerns, discuss the feasibility of treatment and obtain informed consent (risk-benefit analysis). Understanding and addressing the patient’s main concerns is essential for a successful treatment outcome. Computerised prediction software (e.g. Dolphin) is available to allow visualisation of proposed treatment changes.
At the end of this consultation, there should be a cl/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


