CHAPTER 42
Rhinoplasty
Jon D. Perenack and Shahrouz Zarrabi
Department of Oral and Maxillofacial Surgery, Louisiana State University Health Sciences Center, New Orleans, Louisiana, USA
Procedures aimed at improving the form and/or function of the nose and associated structures.
Indications
Correction of Functional Nasal Deformities
- Septal deformity: deviated nasal septum, bone spurs, and internal and external nasal valve deformities
- Intranasal abnormalities: turbinate hypertrophy, septal perforations, synechiae, and intranasal pathology
Correction of Aesthetic Deformities as a Result of Congenital and Acquired (Trauma) Deformities
- Upper nose deformities: high or low dorsal hump, lateral dorsal hump, elongated nose, thin or broad nasal dorsum, and nasal deviations
- Lower nose deformities: poorly defined nasal tip, nasal tip deviation, over– or underprojection of the nasal tip, large or asymmetrical nostrils, and excessive columella show
- Posttraumatic deformities: crooked nose and saddle nose deformities
- Revision rhinoplasty: undesired cosmetic result from prior rhinoplasty
Contraindications
- Uncontrolled systemic illness
- Large septal perforations
- Unstable nasal support structures secondary to trauma
- Multiply operated rhinoplasty patient with a scarred or avascular skin–soft tissue envelope (S-STE)
- Heavy smoker
- Psychological disorders, such as body dysmorphic disorder, depression, and personality disorders
Anatomy
- Membranous septum: The portion of the septum located between the cartilaginous septum and the columella.
- Nasal septum: The nasal septum is a combined bony and cartilaginous structure that separates the nasal vault into two halves, provides support to the nasal tip, and stabilizes the upper and lower lateral cartilages (LLC). The anterior aspect of the nasal septum is cartilaginous, and the posterior and cephalic aspect of the nasal septum is osseous. The cartilaginous septum is quadrangular in shape and is fused to the paired upper lateral cartilages (ULC) dorsally and to the anterior nasal spine and maxillary crest anteriorly and inferiorly. The osseous septum is composed of the bones of the vomer and the perpendicular plate of the ethmoid. The vomer bone articulates with the posterior maxillary crest. The perpendicular plate of the ethmoid articulates with the nasal bones, frontal bone, and cribriform plate.
Septal Procedures
- Caudal septoplasty: Procedures performed to address the deviated cartilaginous portion of the nasal septum to improve obstructive nasal breathing, correct cosmetic deformities or deviations, and/or harvest a section of cartilage for adjunctive grafting procedures. A large quantity of cartilage may be harvested from the central cartilaginous septum (quadrangular resection). It is paramount to leave at least a 10 mm dorsal and caudal cartilaginous strut (Figure 42.1) for support of the nasal complex. During revision rhinoplasty, if the septum has been previously harvested, alternative sites for cartilage harvesting include the conchal bowl of the ear and the costochondral cartilage obtained from the sixth and seventh ribs.
- Septal repositioning: Repositioning of a deviated cartilaginous septum within the midline of the nasal cavity. The cartilaginous septum may be repositioned with or without cartilage resection. A mucoperiochondrial dissection is initiated along the inferior aspect of the cartilaginous septum to mobilize the septum from the anterior nasal spine and maxillary crest. The cartilaginous septum is mobilized and positioned along the midline of the nasal cavity. More commonly, a “swinging-door” technique is utilized to resect a conservative inferior strip of cartilage to allow repositioning along the midline of the nasal vault. A nonresorbable suture is frequently placed through the anterior and inferior portion of the cartilaginous nasal septum and secured to the anterior nasal spine or the periosteum overlying the anterior nasal floor or maxillary crest (Wright suture).
- Cartilage scoring: Cartilage scoring is performed to facilitate septal cartilage straightening. Scoring is done perpendicular to the orientation of the deviation and is frequently required on both sides of the involved cartilage to soften and reform deviated cartilage.
Spreader grafting: A section of cartilage, typically harvested from the nasal septum, is positioned bilaterally between the superior articulation of the cartilaginous septum and the ULC (see Figures 42.31, 42.32, and 42.33 in Case Report 42.2). Spreader grafts are utilized to open the internal nasal valve (increase nasal airflow), to reconstruct or widen a narrow middle nasal vault, to increase nasal length in patients with a short nose, and to reconstruct hump deformities during revision rhinoplasty.
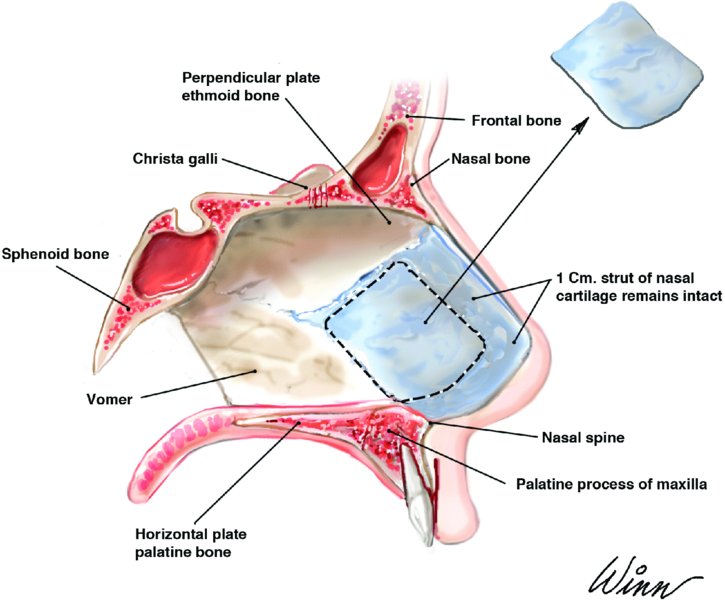
Figure 42.1. Anatomy of the nasal septum and quadrangular cartilage harvest.
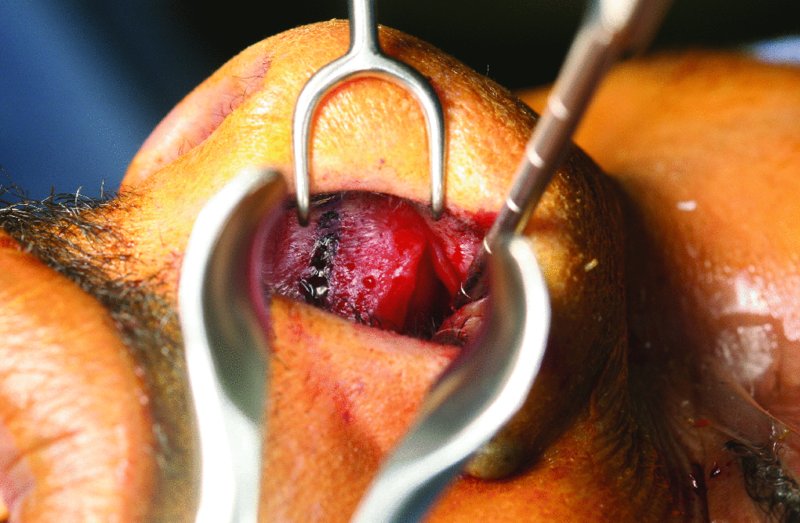
Figure 42.2. A Killian incision placed 5 mm posterior and parallel to the caudal margin (blue surgical marking) of the cartilaginous septum.
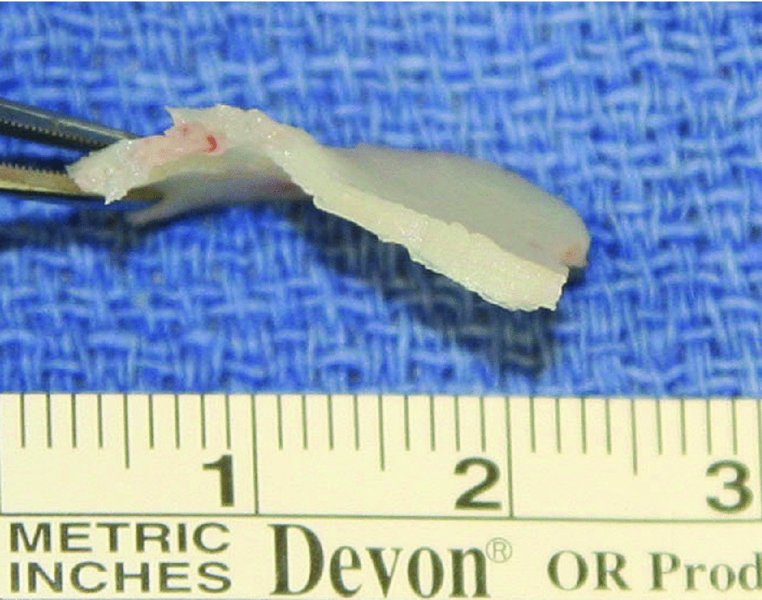
Figure 42.3. Resected deviated cartilage. A 10 mm dorsal and caudal strut of the cartilaginous septum was preserved.
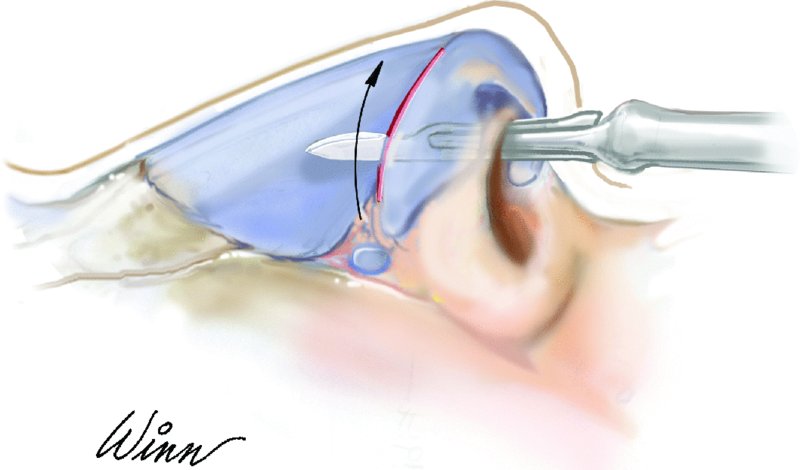
Figure 42.4. Endonasal rhinoplasty incision transecting the scroll area.
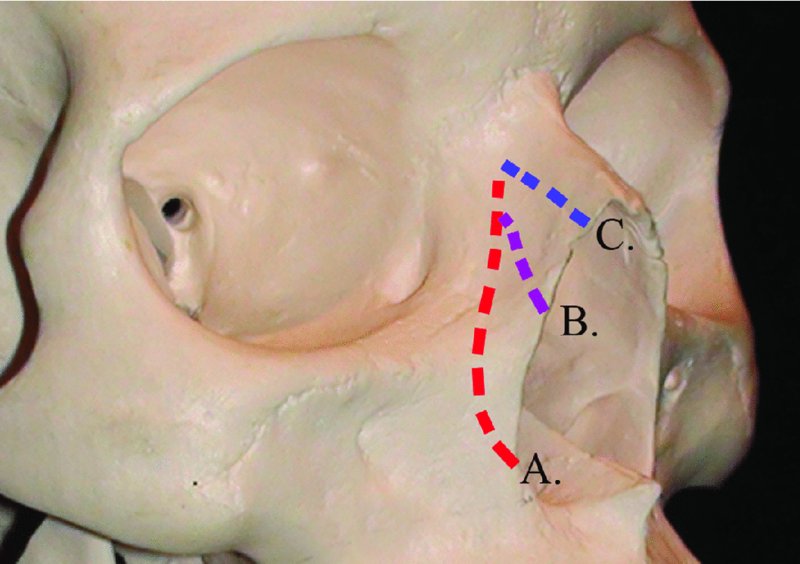
Figure 42.5. Sites of (A) lateral, (B) intermediate, and (C) medial nasal osteotomies.

Figure 42.6. Preoperative anterior-posterior view.

Figure 42.7. Preoperative three-quarters view.

Figure 42.8. Preoperative lateral view.

Figure 42.9. Preoperative worm’s-eye view.

Figure 42.10. Software generated before and after anterior-posterior views depicting correction of the excessively wide nasal vault, nasal vault deviations and asymmetries, and the bulbous nasal tip.

Figure 42.11. Software generated before and after lateral views depicting correction of the high nasal dorsum, ptotic nasal tip, and excessive columella show.
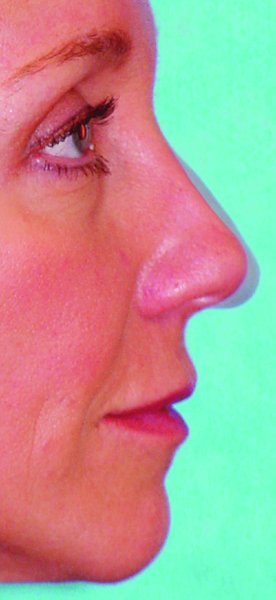
Figure 42.12. Software-generated lateral view depicting before and after results within the same image.
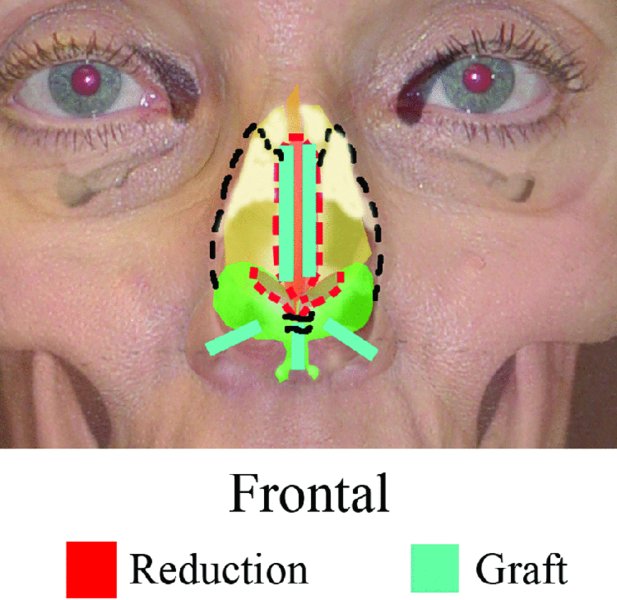
Figure 42.13. Schematic treatment plan, anterior-posterior view.
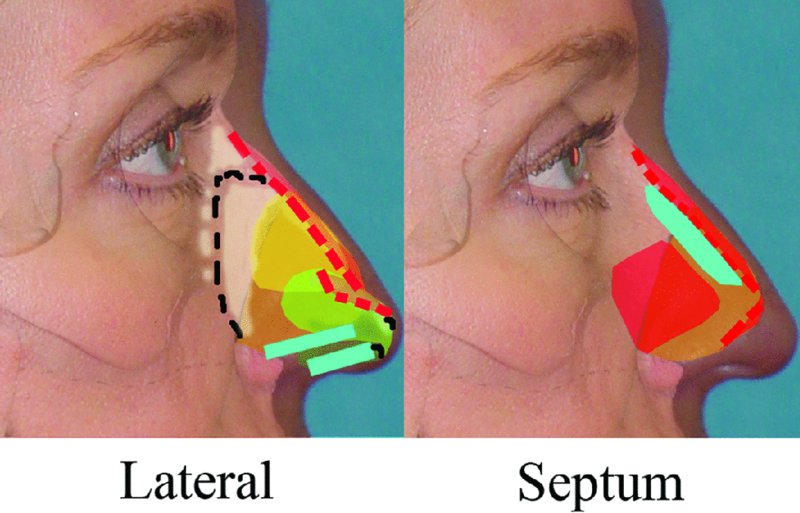
Figure 42.14. Schematic treatment plan, lateral view.

Figure 42.15. Marking of W-shaped transcolumellar incision.
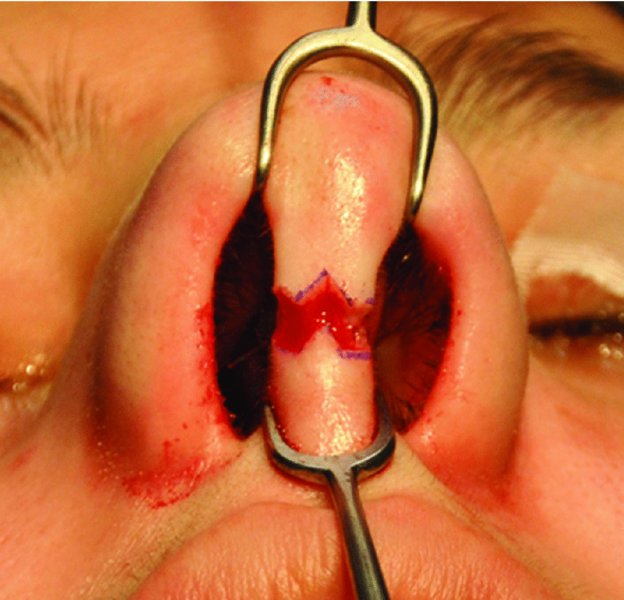
Figure 42.16. Initiation of transcolumellar incision.

Figure 42.17. The marginal incisions are carried medially to join the transcolumellar incision.

Figure 42.18. Angled scissors are used to dissect superficial to the medial crura to connect the bilateral marginal incisions with the columellar incision.
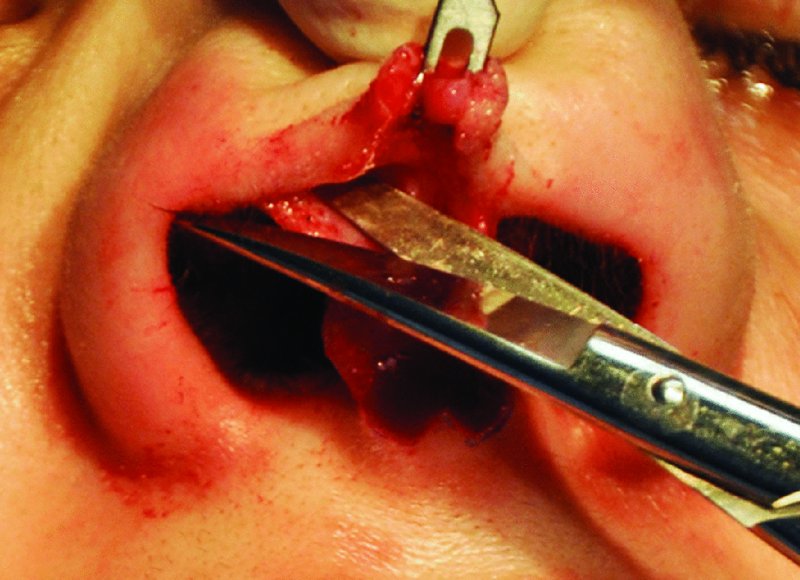
Figure 42.19. Marginal incision is completed along the caudal aspect of the lower lateral cartilages, and iris scissors are used to dissect the overlying skin–soft tissue envelope.
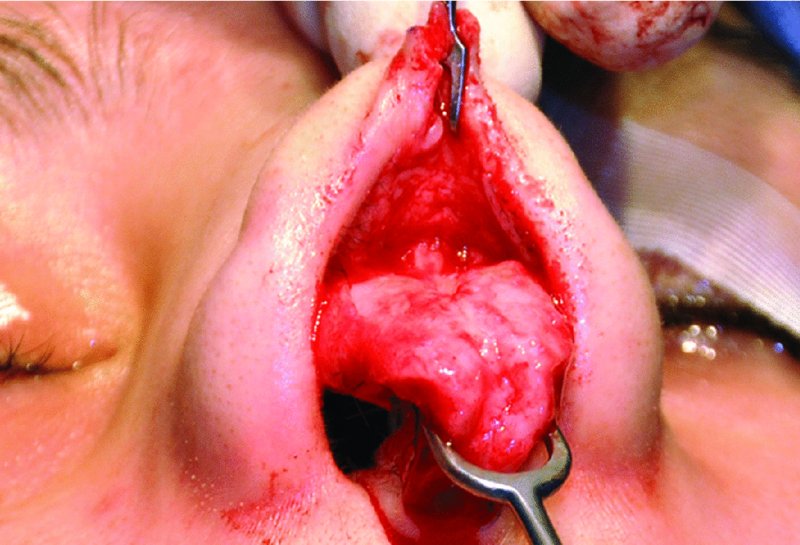
Figure 42.20. The lower lateral cartilages are freed from the skin–soft tissue envelope and fully exposed.
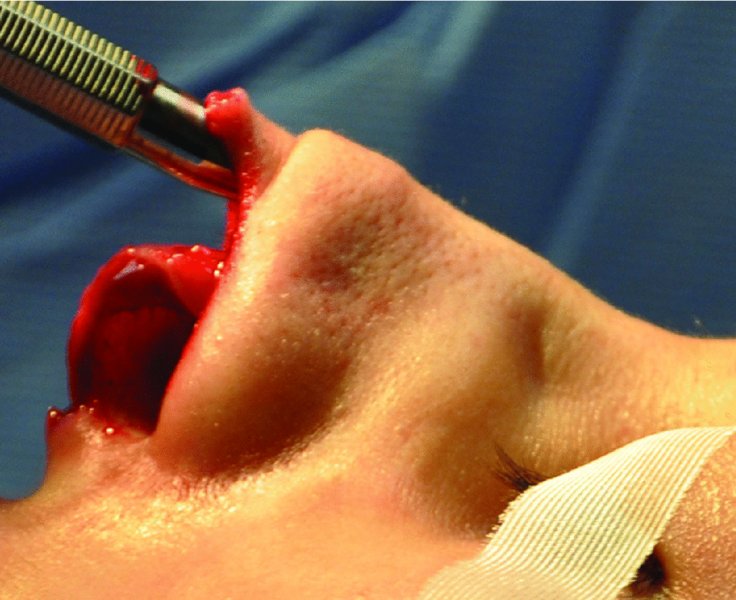
Figure 42.21. A #9 periosteal elevator is used to expose the upper lateral cartilages and the nasal bones.
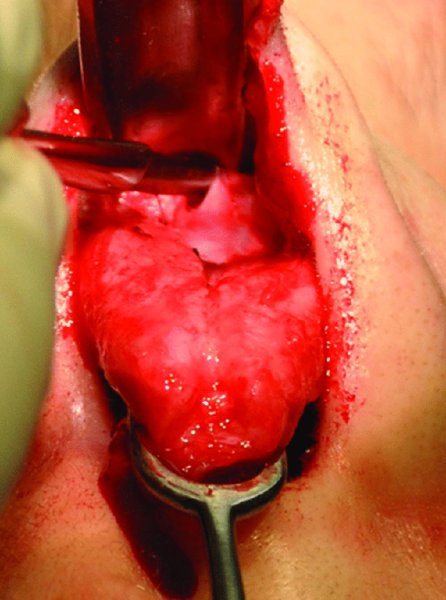
Figure 42.22. An Aufricht nasal retractor is placed to expose the upper vault, and a Joseph knife is used in a sweeping motion to remove residual fibrous attachments from the lateral aspect of the upper lateral cartilages.

Figure 42.23. Open view reveals septal deviation, a bulbous nasal tip, and deviation of the nasal tip.

Figure 42.24. After correction of the deviated nasal septum, a 2×12×1 mm columellar strut is placed within a pocket formed between the medial crura to further correct the deviated nasal tip and to provide tip projection.

Figure 42.25. The columellar strut is secured with interrupted prolene sutures, and a cephalic trim is performed with a #15 blade.
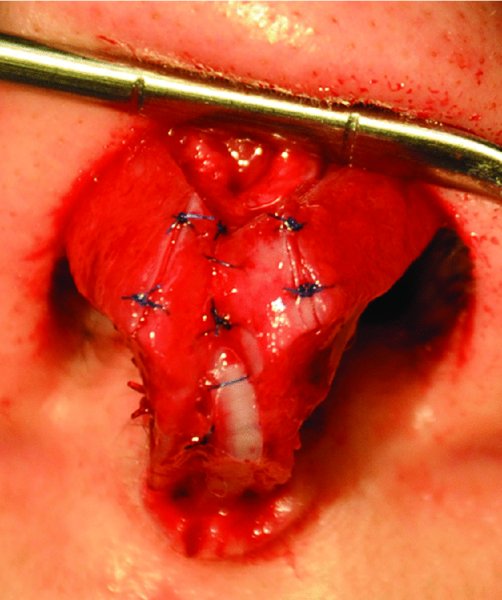
Figure 42.26. Cephalic trim completed, and interdomal sutures placed.

Figure 42.27. An 8×5×1 mm shield graft is fashioned from the quadrangular septal harvest, the edges are beveled to minimize visibility, and the graft is fixated to the infratip region with 6-0 nylon sutures. Shield grafts provide definition and added support to the nasal tip.
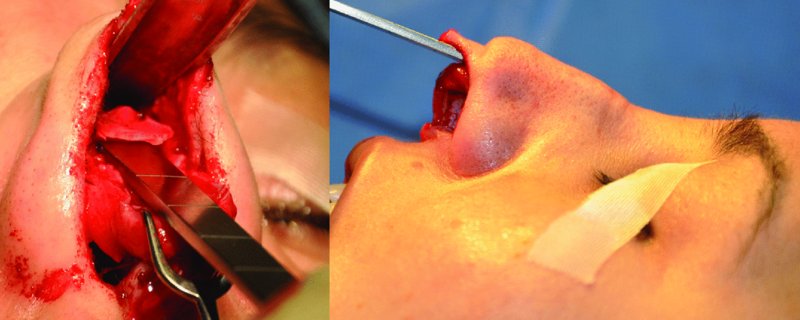
Figure 42.28. A #15 blade and a sharp monobevel chisel are used to resect the dorsal hump.
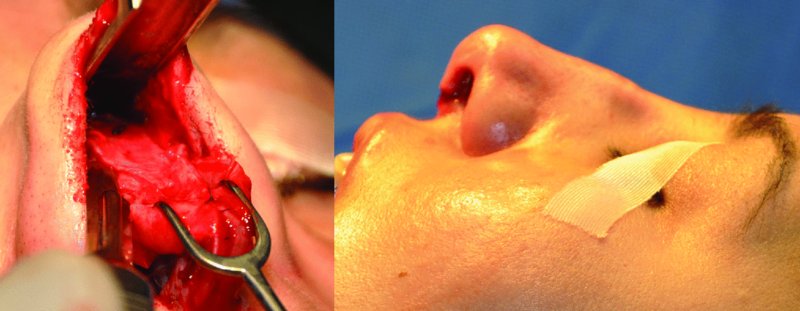
Figure 42.29. An Aufricht nasal retractor is inserted to directly visualize the dorsal reduction. The skin–soft tissue envelope was redraped to evaluate the dorsum after hump reduction.
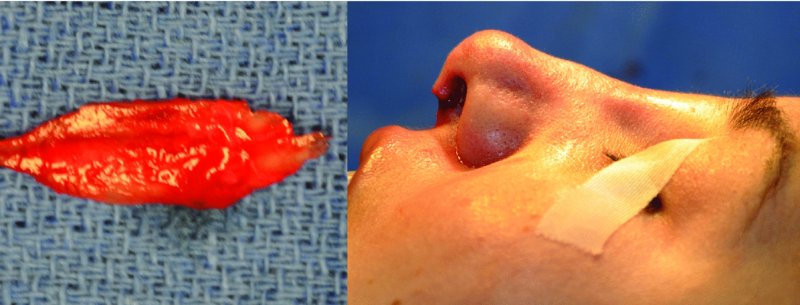
Figure 42.30. The resected portion of the cartilaginous-bony dorsal hump. A push rasp was used to further reduce the dorsum and to remove any irregularities. The skin–soft tissue envelope is redraped to assess hump reduction and symmetry.
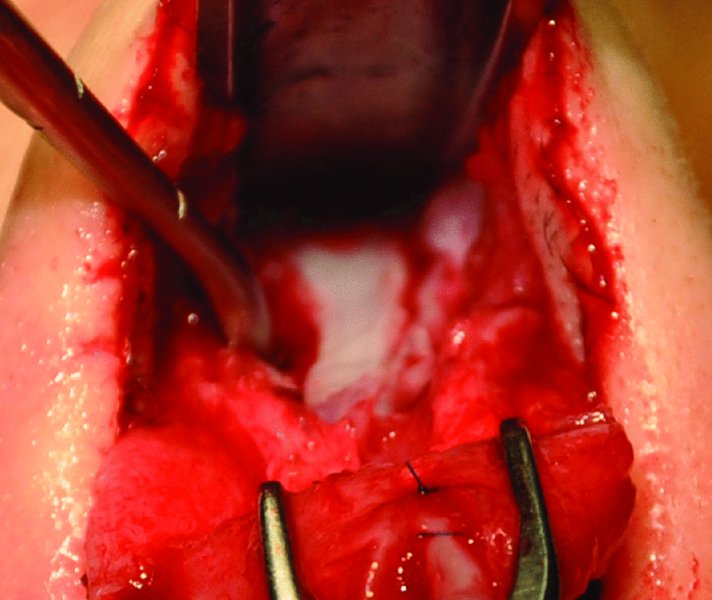
Figure 42.31. The development of pockets between the nasal septum and the upper lateral cartilages for the placement of spreader grafts.
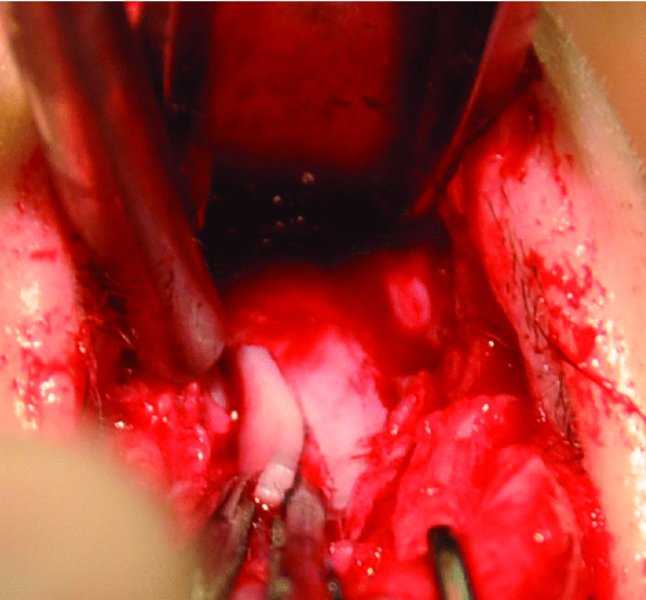
Figure 42.32. Spreader grafts were fashioned from the inferior straight segment of the quadrangular septal cartilage and placed within pockets adjacent to the septum.
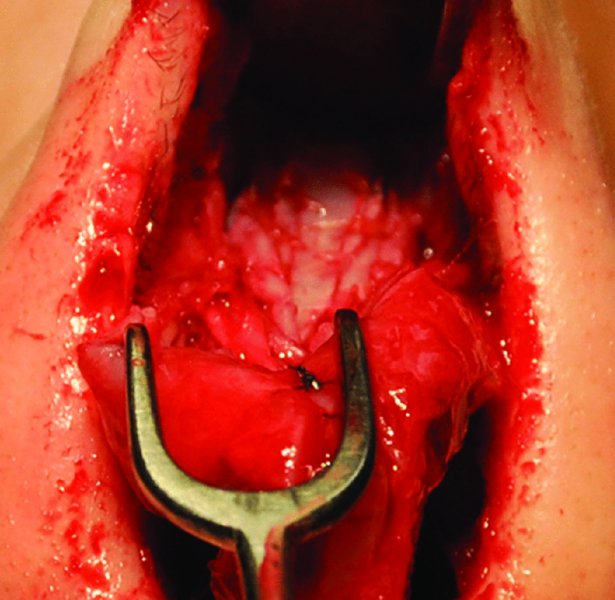
Figure 42.33. Spreader grafts in place and secured with interrupted 5-0 gut sutures.
Turbinate Anatomy and Procedures
- Turbinates: The three paired nasal turbinates (superior, middle, and inferior) are positioned along the lateral nasal wall via thin turbinate bones. Their function is to humidify and warm inspired air. The inferior turbinate is a common cause of obstructive nasal breathing.
- Total inferior turbinectomy: Involves the out-fracture of the turbinate bone and the resection of the entire inferior turbinate along its lateral attachment to the lateral nasal wall. This procedure is infrequently performed due to its alteration of nasal physiology, which leads to postoperative epistaxis, crusting, atrophic rhinitis, and dryness.
- Partial anterior turbinectomy: Involves the removal of the anterior one-third to one-half of the affected inferior turbinate. Minimizes the risks associated with total inferior turbinectomy.
- Submucous resection: Involves removal of the inferior turbinate bone while preserving the overlying mucosa. By maintaining the overlying mucosal flaps, the normal mucosal functions are preserved and complications (crusting, atrophic rhinitis, and dryness) are minimized.
Other methods of turbinate treatment include electrocautery, radiofrequency and laser reduction, cryosurgery, and out-fracture without reduction or removal.
Nasal Valves: Anatomy and Procedures
- Internal nasal valve: The junction of the nasal septum and the caudal margin of the ULC (normally, 10–15°). The internal nasal valve comprises the narrowest portion of the nasal airway and is commonly associated with obstructive nasal breathing. Narrowing of the internal nasal valve is corrected with spreader grafts to increase the internal valve angle and to stent the airway open.
- External nasal valve: Located caudal to the internal nasal valve and bounded laterally by the ala and medially by the septum and columella. The external nasal valve is essentially the vestibule that serves as the entrance to the nose. A collapsed external nasal valve frequently presents as a collapse of the alar rim during inspiration. Collapsed external nasal valves are treated by correcting any underlying septum deviations and with alar rim grafts to open the angle of the external nasal valve.
Nasal Skin–Soft Tissue Envelope (S-STE)
- Thick S-STE: Thick and sebaceous tissues are more adapt to concealing deformities and hiding minor irregularities and asymmetries. However, it is more difficult to obtain well-defined cosmetic results with thicker nasal tissues.
- Thin S-STE: Underlying definition of the nasal skeleton is readily visible. Allows for well-defined nasal tip anatomy. Readily shows nasal irregularities, imperfections, and asymmetries.
Nasal Skeleton
- Nasion: The intersection of the nasal bone and the frontal bone. Represents the deepest aspect of the nasofrontal angle. A deep nasion can be augmented with alloplastic (expanded polytetrafluoroethylene) and/or autogenous (morselized septal cartilage, costochondral cartilage, and temporal fascia) grafts to increase the nasofrontal angle.
- Nasal bones: The paired nasal bones form the bony roof of the nose and articulate with each other medially, with the maxilla laterally, the frontal bone superiorly, the ULC inferiorly, and the perpendicular plates of the ethmoid posteriorly.
- Upper lateral cartilages: Attach to the midline septum and form the cartilaginous midvault. The cephalic portion of the ULC is attached and overlapped by the paired nasal bones.
- Lower lateral cartilages (or alar cartilages): The C-shaped and paired LLC are each composed of a medial, middle, and lateral crura. Supported inferiorly by the caudal aspect of the septum and the pyriform aperture. The LLC determine the majority of the nasal tip shape, size, and projection.
- Scroll region: The junction where the LLC overlap the ULC.
- Keystone area: The junction of the ULC, the nasal bones, and the septum.
Initial Nasal Examination
- Discussion regarding the patient’s chief complaints regarding nasal function and aesthetics.
- Preoperative photographs are taken that will allow the surgeon to manipulate the images in their preferred computer software package (to be used as a visual aid for evaluation with the patient) and will allow for an intraoperative reference during the rhinoplasty surgery.
- Aesthetic evaluation of the entire face and nasal anatomy to include the nasal tip, dorsum, nasal base, alar rims, columella, nasal bones, radix, and S-STE, as well as overall symmetry during both animation and repose.
- Intranasal examination with a nasal speculum to view the nasal septum to identify areas of deviation, mucosal condition, septal perforations, synechiae, and intranasal masses. Particularly important in patients with functional complaints, with previous nasal surgery, and requiring septal harvest and grafting. The inferior turbinates are also evaluated for hypertrophy contributing to obstructive nasal breathing.
- Either a treatment plan may be created at the initial visit and reviewed with the patient, or it may be developed and reviewed with the patient at a subsequent visit prior to surgery. The treatment plan should address both functional and aesthetic patient concerns and allow for an open discussion with the patient and surgeon regarding treatment.
Septal Access: Killian and Transfixion Incisions
Killian Incision
Indications
- Provides access to harvest a quadrangular graft specimen
- Provides access to the midseptum (quadrangular septum), vomer, and ethmoid
- Minimal disturbance of adjacent structures
Contraindications
- Poor access to caudal and dorsal septal deformities
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


