CHAPTER 41
Upper and Lower Lid Blepharoplasty and Tear Trough Implants
Dustin M. Heringer1 and L. Angelo Cuzalina2
1Department of Ophthalmology, University of Arizona, Tucson, Arizona, USA
2Cosmetic Surgery Fellowship Director, American Academy of Cosmetic Surgery, Tulsa, Oklahoma, USA
Upper Lid Blepharoplasty Procedure
The excision of excess upper lid skin and/or fat for cosmetic or functional improvement.
Indications
- Dermatochalasis
- Psuedoherniation or prolapsing of central and medial orbital fat that is cosmetically troublesome to the patient
- Upper lid ptosis
- Asymmetries
- Vision blocked by excess upper lid skin (lateral hooding). In order to qualify for a functional procedure, loss of the visual field must be documented with visual field testing and photographs
Contraindications
- Blepharoptosis: Blepharoptosis will not be corrected with blepharoplasty alone and requires identification prior to surgery. Blepharoptosis and lid malposition should be addressed prior to, or concurrently, with blepharoplasty to minimize postoperative complications.
- Eyebrow ptosis: Eyebrow ptosis is frequently the patient’s chief complaint, and should be recognized and treated with a brow lift instead of upper blepharoplasty.
- Active thyroid disease: Patient’s with active thyroid eye disease should avoid cosmetic upper and lower lid blepharoplasty until their disease has been stable for 12 months.
- Refractive eye surgery: upper and lower lid blepharoplasty should be avoided in patients who have undergone lamellar refractive surgery within the previous 6 months or surface ablative refractive surgery within the previous 3 months.
- Severe dry eye syndrome (relative contraindication): An upper lid blepharoplasty may exacerbate the condition, especially if postoperative lagophthalmos is present. It is important to obtain a detailed ophthalmic history with attention to eye drop and ointment usage. Basal tear secretion testing (Schirmer testing) can be helpful, but the results of this test are sometimes unpredictable.
- Lack of orbicularis oculi strength and/or absent Bell’s phenomenon (relative contraindications): Both increase the incidence of postoperative corneal trauma.
Anatomy and Definitions: Upper Lid
- Dermatochalasis: Excessive or redundant skin of the upper and lower eyelid. Often associated with excessive skin laxity as well.
- Blepharoptosis: Ptosis of the upper eyelid resulting in a low-lying upper eyelid margin.
- Lagophthalmos: The inability to completely close the eyelids.
- Bell’s phenomenon: The ability of the eyeball to move superiorly with eyelid closure. A protective reflex that aids in preventing corneal trauma, especially if postoperative lagophthalmos is present.
- Marginal reflex distance (MRD): A means of identifying the position of the upper and lower lids in reference to the eye by measuring the distance of the upper and lower lid margin from the pupillary light reflex.
- Margin reflex distance-1 (MRD1): The distance from the center of the pupillary light reflex and the upper eyelid margin with the eye in primary gaze. The normal range for MRD1 distance is 4–5 mm. An MRD1 of less than 4 mm may indicate blepharoptosis. An MRD1 of greater than 5 mm may indicate proptosis from hyperthyroidism.
- Margin reflex distance-2 (MRD2): The distance from the center of the pupillary light reflex and the lower eyelid margin with the eye in primary gaze. The normal range for MRD2 distance is 5 mm. An MRD2 of greater than 5 mm may indicate lower lid retraction.
Layers of the upper eyelid superior to the tarsal plate (9–10 mm high centrally), from external to internal (Figure 41.1):
- Skin
- Orbicularis oculi
- Orbital septum
- Preaponeurotic fat
- Levator palpebrae superioris
- Müller’s muscle
- Conjunctiva.
- Orbicularis oculi muscles: Innervated by the frontal (temporal) and zygomatic branches of the facial nerve located on the underside of the muscle. Functions to close the eyelid.
- Orbital septum: A tough fibrous layer that lies anterior to the preaponeurotic fat and posterior to the orbicularis muscle. The orbital septum extends from the orbital rim to the tarsal plate and separates the eyelid from the orbit.
- Preaponeurotic fat: Consists of fat pads that lie anterior to the levator aponeurosis and posterior to the orbital septum. The upper lid contains only two fat pads: a central and a medial fat pad. The central fat pad is more yellow in appearance, whereas the medial fat pad is whiter in appearance. There is no lateral fat pad. The lacrimal gland lies in the preaponeurotic space laterally and appears whitish-gray, glandular, and irregular.
- Levator palpebrae superioris muscle: Innervated by the oculomotor nerve and is the primary muscle responsible for opening the eyelid. Fibrous extensions from the levator palpebrae superioris muscle pass through the orbicularis muscle to insert on the skin and help create the upper lid crease.
- Müller’s muscle: Innervated by sympathetic nerves and functions to involuntarily open the eyelid. Müller’s muscle is located between the conjunctiva posteriorly and the levator muscle anteriorly. Originates on the inferior aspect of the levator palpebrae muscle and inserts onto the superior border of the tarsal plate.
- Conjunctiva: A mucous membrane that lines the posterior surface of the eyelid (palpebral) and anterior eyeball (bulbar). The conjunctiva is composed of nonkeratinized squamous epithelium that contains goblet cells that protect and lubricate the eye.
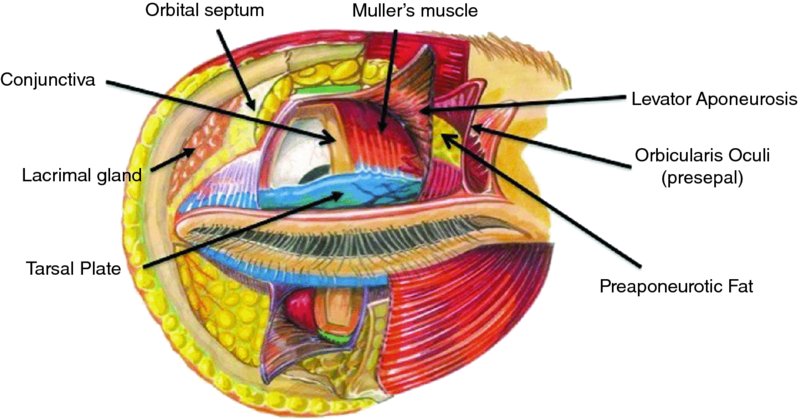
Figure 41.1. Anatomy of the upper eyelid. Image by Randy Sappo.
Upper Blepharoplasty Preoperative Assessment and Markings
-
Prior to any upper and lower blepharoplasty procedure, a thorough history and physical should be performed that assesses and documents visual acuity, facial nerve function, asymmetries, dryness of the eyes, lagophthalmos, orbicularis oculi strength, and Bell’s phenomenon. Preoperative photographs should be taken and should include frontal, three-quarter, and lateral views (Figures 41.2 through 41.7).
- Preoperative markings are performed with the patient in a seated and upright position. The patient’s natural upper lid skin crease is marked. The upper lid skin crease is typically 7–8 mm superior to the lid margin in males (Figure 41.8) and 8–10 mm superior to the lid margin in females. A pinch test is performed to define the upper extent of the excision. A pinch test is conducted by gently pinching the excess skin superior to the marked eyelid crease with blunt pickups until there is slight eversion of the upper lid eyelashes without lagophthalmos. The upper mark for the blepharoplasty incision is designed to maintain 10–15 mm of skin between the inferior brow hairs and the upper mark to prevent overresection. Therefore, the total amount of skin remaining from the lid margin to the inferior brow hairs is at least 20 mm. When marking laterally, make sure to extend the skin incision upward into one of the crow’s feet starting at the lateral canthus to prevent the incision from extending too low.

Figure 41.2. Frontal preoperative view depicting a tired and aged look to the eyes.

Figure 41.3. Three-quarters preoperative view depicting upper lid dermatochalasis, nasal asymmetry, and a dorsal nasal hump deformity.

Figure 41.4. Lateral preoperative view depicting lateral hooding of the upper, lateral quadrant of the upper lid.

Figure 41.5. Frontal postoperative view depicting a more youthful appearance of the eyes after correction of dermatochalasis with upper lid blepharoplasty.

Figure 41.6. Three-quarters postoperative view depicting correction of dermatochalasis, nasal asymmetries, and dorsal hump reduction.

Figure 41.7. Lateral postoperative view depicting correction of lateral hooding.

Figure 41.8. Preoperative markings for upper lid blepharoplasty are shown in red.
Upper Lid Blepharoplasty Procedure
- The procedure may be performed with local anesthesia alone, intravenous sedation, laryngeal mask airway (LMA), or endotracheal anesthesia.
- After induction of anesthesia, the patient is placed supine, and 1 to 1.5 mL of local anesthetic containing epinephrine is injected just below the skin within the areas of excision in both upper lids with a 30-gauge needle.
- The patient is prepped and draped in a sterile fashion.
- The incision is initiated along the preoperative markings with a #15 blade, CO2 laser, or needlepoint cautery. If using a CO2 laser, make sure to place metallic eye shields prior to making an incision. The depth of the incision extends through the orbicularis muscle to the septum. You will observe a color change from pink to white when the septum is reached.
- Remove the excess skin and orbicularis muscle with needlepoint cautery or scissors within the tissue plane just anterior to the septum (Figure 41.9).
- If prolapsing pre-aponeurotic fat removal is required, needlepoint cautery is utilized to open the septum and to expose the central and medial fat pads. The medial fat pad is easily differentiated from the central fat pad due to its whiter appearance than the central fat pad. In the preaponeurotic space laterally, the lacrimal gland may prolapse and create fullness or a contour irregularity. A 6-0 polyglycolic acid suture (Vicryl) can be used to suspend and reposition the prolapsing gland to the medial aspect of the superolateral orbital rim periosteum.
- If performing the procedure under local anesthesia alone, local anesthesia is injected into each fat pad prior to removal to minimize patient discomfort.
- The herniated fat is gently teased out with a hemostat or forceps and excised with needlepoint cautery using the coagulation mode (Figure 41.10). Attempt to remove equal amounts of fat from each side for symmetry, unless an asymmetry was identified preoperatively.
- If lower lid laxity or malposition is present, a canthopexy procedure can be performed through the upper lid incision to resuspend the lateral canthal tendon. Scissors are used to dissect down to the lateral canthal tendon posterior to the skin and orbicularis oculi muscle. Using forceps, the tendon is identified, and a 6-0 polyglycolic acid suture (Vicryl) is passed first through the tendon and then through the medial aspect of the superolateral orbital rim periosteum. The suture is tightened until the canthus has a pleasing appearance. The lateral canthus usually has a slight superior angle in females and is level with the medial canthus in males.
- Skin closure is performed with a running 6-0 polypropylene (Prolene) or fast-absorbing gut suture. If the patient exhibits a poorly defined lid crease, fixation of the inferior skin edge to the levator aponeurosis at the superior aspect of the tarsal plate with a 6-0 polyglycolic acid suture (Vicryl) will help define the fold. One suture should be placed centrally with additional sutures placed at the medial and lateral limbus.

Figure 41.9. The skin and orbicularis muscle of the upper lid are excised together as a unit with needlepoint cautery. Note the white septum beneath the orbicularis muscle.

Figure 41.10. The medial fat pad is gently teased out from its capsule with forceps, and the prolapsing fat is removed with cautery to coagulate small perforating vessels within the fat pad. After fat removal is completed, the skin incision will be closed with a running suture.
Complications
- Asymmetry: Minimized with a thorough preoperative examination with eyelid measurements to identify preexisting conditions (i.e., blepharoptosis) and asymmetries, meticulous preoperative markings, and surgeon experience.
- Blepharoptosis: Typically occurs secondary to postoperative edema and resolves within 2–4 weeks after surgery. Occasionally, prolonged edema can lead to attenuation of the levator palpebrae superioris muscle, resulting in a persistent blepharoptosis. Excessive tension during the surgical removal of upper eyelid skin can result in a dehiscence of the levator palpebrae superioris, causing ptosis. Blepharoptosis that persists for greater than 6 months after surgery usually requires surgery for correction.
- Lagophthalmos: Frequently the result of the removal of excessive upper eyelid tissue. A good rule of thumb is to leave 20 mm of skin between the eyelid margin and the inferior brow hairs. In addition, incorporating the septum into the closure can cause adhesions and prevent adequate closure. Untreated or unrecognized lagophthalmos will lead to corneal exposure and dry eye. Mild cases of lagophthalmos are managed with lubricants and massage until the condition resolves. Severe cases are managed with skin grafting to the upper lids.
- Hematoma: Typically result from bleeding of the orbicularis oculi muscle postoperatively. Small hematomas are observed and resolve without sequelae. Larger hematomas require evacuation to prevent fibrosis and scarring of the eyelid. Expanding hematomas require immediate surgical exploration with evacuation and control of the source of bleeding.
- Retrobulbar hematoma: Minimized with appropriate use of cautery and wound hemostasis prior to the termination of the procedure. Posterior bleeding may result in a compartment syndrome, which places pressure on the blood supply to the retina and, if unrecognized or untreated, can lead to permanent vision loss. Signs and symptoms include severe ocular pain, proptosis, massive edema, limited or absent extraocular movement, elevated intraocular pressure, vision loss, and an unreactive pupil. Retrobulbar hematomas are a medical emergency and require immediate action to prevent permanent loss of vision. Initial treatment involves opening the surgical incision and attempting to visualize and evacuate the forming hematoma. If the evacuation of the hematoma though the incision site fails, a lateral canthotomy with cantholysis of the upper and lower limbs of the lateral canthal tendon is performed to increase the volume of the orbit. In rare cases, decompression of the bony orbit may be accomplished by pushing a hemostat through the medial wall and orbital floor. After decompression, an ophthalmology consult is warranted to monitor vision and for serial intraocular pressure checks.
- Infection: Rare due to the rich blood supply to the eyelids. Signs and symptoms of an eyelid infection include increased erythema, edema, pain, and purulent discharge from the surgical site. Infections are treated with the administration of broad-spectrum oral antibiotics. If an abscess is present, drainage of the abscess with culture and sensitivities is indicated.
- Corneal abrasion: Present as pain and increased light sensitivity in the affected eye after surgery. Diagnosis may be made via symptoms alone or in conjunction with fluorescein drops and a cobalt blue light to visualize the abrasion and to confirm the diagnosis. Treatment consists of ophthalmic antibiotic ointment to the affected eye 4–6 times per day until symptoms resolve. Corneal abrasions typically heal in 24 to 48 hours depending on the size of the abrasion.
Key Points
- Excessive fat pad removal is avoided to prevent creating an “A-frame” deformity or hollow appearance to the upper lid. Only fat that prolapses anterior to the septum with light pressure to the globe should be excised.
- Always remove herniating fat with coagulation in order to cauterize small vessels traveling through the fat and to minimize postoperative bleeding and hematoma formation.
- Avoid removing excess skin. The surgeon should leave approximately 20 mm of skin between the eyelid margin and lower brow hairs to avoid postoperative lagophthalmos.
- Always evaluate the patient to see if he or she has brow ptosis and would benefit from a brow lift instead of, or in addition to, an upper lid blepharoplasty. Always perform the brow lift first to ensure the upper eyelid skin is not over-resected. Performing upper lid blepharoplasty in a patient with brow ptosis will further lower the position of the brow.
References
- Gentile, R., 2005. Upper lid blepharoplasty. Facial and Plastic Surgery Clinics of North America, 13, 511–24.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


